Oesophageal carcinoma mimicking a submucosal lesion:A case report
2019-11-21RevathyMarimuthuShanmugamChitraShanmugamManimaranMurugesanMuthukumaranKalyansundaramSathyaGopalsamyAmiyaRanjan
Revathy Marimuthu Shanmugam,Chitra Shanmugam,Manimaran Murugesan,Muthukumaran Kalyansundaram,Sathya Gopalsamy,Amiya Ranjan
Revathy Marimuthu Shanmugam,Chitra Shanmugam,Manimaran Murugesan,Muthukumaran
Kalyansundaram,Sathya Gopalsamy,Amiya Ranjan,Department of Medical Gastroenterology,Government Stanley Medical College,Chennai 600001,Tamil Nadu,India
Abstract
Key words: Intramural esophageal squamous cell carcinoma; Submucosal lesion of esophagus; Endoscopic ultrasound; Case report
INTRODUCTION
Oesophageal cancer is the fourth most common cause of cancer-related deaths in India. It is prevalent among both men and women. Squamous cell carcinoma accounts for up to 80% of these cancers[1]. The etiologic factors for esophageal squamous cell carcinomas (ESCCs) show a regional variation in different parts of India,but tobacco consumption in various forms,as well as alcohol,hot beverages and poor nutrition remain the predominant predisposing factors. The majority of patients with advanced disease are symptomatic,most often presenting with dysphagia and weight loss.
ESCCs arise from the epithelial layer,and commonly present as polypoidal,ulcerative or proliferative ulcer growth in the oesophageal lumen. In contrast,oesophageal submucosal tumours are a distinct group of tumours arising from the mesenchyme (examples include leiomyoma,fibrovasculoma,lipoma,granular cell tumour or carcinoid),and mostly do not breach the mucosa. Complete intramural growth of an advanced primary ESCC is an exceedingly rare presentation,with only six cases reported in the literature thus far[2-7]. We herein report a case of primary ESCC with complete intramural invasion that endoscopically mimics a submucosal lesion. The diagnosis could only be established by an endoscopic ultrasound (EUS)-guided biopsy. This article was published after obtaining informed consent from the patient.
CASE PRESENTATION
Chief complaints
A 50 year old male presented with a progressive mechanical type of dysphagia for a month,which was associated with a significant loss of weight.
History of illness
There was an occasional history of regurgitation present. He denies loss of appetite,retrosternal chest pain or discomfort. He also denies any history of heartburn,caustic ingestion,fever,cough,haemoptysis,change in voice,difficulty in breathing,hematemesis,melena or any drug intake.
Past history was significant for squamous cell carcinoma of the tongue,which was treated with surgery and chemoradiation 1 year prior. He lost follow up for the above.He quit smoking and alcohol after being diagnosed with tongue carcinoma.
Physical examination upon admission
Upon examination,his vitals were stable and there was no significant lymphadenopathy. Oral examination was significant for a scar on the left lateral border of the tongue. His respiratory and gastrointestinal system examination was unremarkable.
Diagnostic assessment and interventions
He was further investigated. The basic metabolic panel was normal.
Upper gastrointestinal endoscopy was performed,which revealed a large,hemispherical lesion with a normal-appearing overlying mucosa about 4 cm × 5 cm in size and extending from 30-34 cm from the incisors,as shown in Figure 1. That impression was that is was possibly a submucosal lesion of the distal oesophagus.Endoscopic biopsy was not done,and further evaluation of the lesion was planned using EUS.
EUS was done using the linear echoendoscope model MAJ1597 (EUS scope,Olympus,Tokyo,Japan). EUS showed a large hyperechoic lesion arising from the third layer at 30 cm,as shown in Figure 2,with a provisional diagnosis of lipoma.
However,in view of the patient’s past history of malignancy,a fine needle biopsy was done using a 19-gauge Boston scientific acquired EUS fine needle biopsy device,and sent for histopathologic examination.
Histopathology revealed fragments of malignant neoplasm composed of cells arranged in sheets,as in Figure 3. The neoplastic cells were round to polygonal,with moderate amounts of eosinophilic cytoplasm with moderate nuclear atypia. Keratin pearl formation was abundant. Histopathology was reported as well-differentiated squamous cell carcinoma. Immunohistochemistry confirmed the same.
Computed tomography (CT) on the thorax was then performed. CT of the thorax with IV and oral contrast showed heterogeneously enhancing soft tissue thickening noted in the retro cardiac oesophagus,with a thickness measuring 38 mm and a length of 68 mm,with proximal oesophageal dilatation noted. The OG junction was normal. The lesion has contact with the descending thoracic aorta at about 90°. The loss of flat plane was noted between the lesion and left atrium. Cavitatory metastatic nodules measuring 26 mm × 18 mm × 33 mm were noted in the posterior basal segment of the left lower lobe. Bilateral hilar nodes were noted,as shown in Figure 4.The CT of the thorax was finally reported as a Retro cardiac oesophageal growth with lung metastasis.
FINAL DIAGNOSIS
Oesophageal squamous cell carcinoma stage 4.
TREATMEN
The patient is currently receiving palliative care.
OUTCOME AND FOLLOW-UP
Not available.
DISCUSSION
The history of intramural ESCC dates back to a case report from McGregoret al[4],wherein a case of squamous cell carcinoma was found to arise from an oesophageal intramural squamous epithelial cyst. There were reports of oesophageal benign cysts as well as carcinoma arising from oesophageal diverticulum. However,for the first time,they reported a case of ESCC arising from an oesophageal cyst. In their case,esophagoscopy revealed a stricture upper oesophagus,and repeat biopsies only revealed mucosal hyperplasia. However,the patient was started on chemoradiation,but he later succumbed to bronchopneumonia. Autopsy demonstrated a 1.5-cm long intramural oesophageal squamous epithelial cyst,from which arose a locally invasive squamous cell carcinoma,without mucosal involvement or metastases. There are several other rare case reports of advanced primary ESCC masquerading as a completely intramural growth.
For this case report,we reviewed the literature,which elucidated the role of EUS in the evaluation of oesophageal submucosal lesions. We could find only two such cases where EUS diagnosis of a submucosal lesion was made,which upon further investigation turned out to be intramural ESCC. One such study was by Choudharyetal[2],where ESCC presented as a submucosal lesion with repeatedly negative endoscopic biopsies. The patient underwent EUS,and fineneedle aspiration was done.The cytopathological report was suggestive of squamous cell carcinoma. There were no distant metastases in this case. The second case report was from Sonthaliaet al[3]. In their report,EUS revealed a heteroechoic solid mass originating from the muscularis propria of the distal oesophagus. Cytological study of EUS-guided fine needle aspiration from the mass was suggestive of squamous cell carcinoma,which was confirmed upon immunohistochemistry. However,this case had bone metastasis.Also,there are certain limitations in EUS-guided fine needle aspiration cytology(FNAC) for the diagnosis of submucosal tumours,as the average diagnostic accuracy rate of EUS-FNA is 60-80%[3].
Compared to the above case reports,our case differs in that our patient had a past history of malignancy. In addition,an EUS fine needle biopsy was done for the evaluation of a submucosal lesion in the oesophagus,which has not been done in the past.
Gibiinoet al[8]have also advocated that EUS fine-needle biopsy has high diagnostic accuracy,and is expected to move the practice of EUS from cytology to histology. This should thereby expand the utilization of EUS throughout the world,and facilitate targeted therapies as well as the monitoring of treatment response in a more biologically-driven manner.
CONCLUSION
This case report highlights that intramural ESCC may look like a submucosal lesion in endoscopy,and that EUS biopsy is therefore needed for final diagnosis.
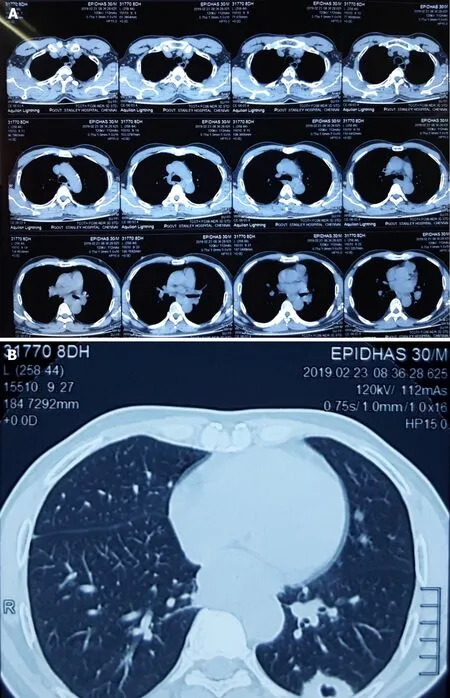
Figure4 Computed tomography images.
