Study of changes in higher-order aberrations following non-penetrating deep sclerectomy surgery augmented with sub-Tenon injection of MMC in patients with open-angle glaucoma
2019-11-12AliMostafaei1NazliTaheriAtenaLatifi
Ali Mostafaei1, Nazli Taheri, Atena Latifi
Abstract
INTRODUCTION
Glaucoma is an optic neuropathy with progressive changes in the optic disc and visual field. Surgical treatment is used when IOP cannot be reliably reduced with medication or when there are medication intolerance, poor compliance or funding issues[1]. Trabeculectomy is the most commonly used glaucoma surgery to reduce IOP[2-4]. Nowadays, to reduce complications of trabeculectomy, there is a tendency to use non-penetrating glaucoma surgery method and other (relatively) recent approaches, like MIGS surgeries and micropulse laser.
Studies have shown that patients complained about visual performance related to topographic changes in the cornea following trabeculectomy[5]. There have been complaints from patients regarding postoperative effects on visual quality, but the mechanism and type of the reduced quality have not been accurately identified so far. On the other hand, with advances in wavefront technology, it has been shown that ocular surgeries, including corneal transplantation, pterygium surgery, intraocular lens insertion,etc. affect higher-order aberrations of vision, which can affect patient quality of vision after surgery[6-10].
Fukuokaetal[11]were the first personto show the effect of trabeculectomy on corneal and ocular HOA (higher order aberrations). Other studies have also shown that trabeculectomy causes a change in visual function[12-14]. These visual aberrations can reduce the quality of vision for the patients after trabeculectomy. Eliminating this type of visual aberrations will improve the visual function of these patients following trabeculectomy procedure. The most common and important aberrations related to wavefront in the human eye are defocus disorders: myopia and hyperopia[15]. High-order aberrations include coma, trefoil, spherical aberrations, which can affect the function of vision and its acuity[16].
On the other hand, the formation of scar tissue in the surgical site is the most important factor in reducing the success rate of glaucoma surgery[17-19]. In recent years, the use of mitomycin C (MMC) has led to a significant increase in the success rate of glaucoma surgery. The wound healing delay due to the use of anti-metabolites is associated with an increase in the incidence of hypotony and blebitis.
In this study we evaluated the success of surgery and the IOP reduction in patients following non-penetrating deep sclerectomy surgery which augmented with sub-Tenon injections of MMC. Also we examined the effect of nonpenetrating deep sclerectomy surgery augmented with subenon injections of MMC in patients’ postoperative HOA level.
SUBJECTS AND METHODS
PatientsandExaminationThis study was a non-comparative interventional case series. This study was approved by the Ethical Committee of Tabriz University of Medical Sciences (code: IR.TBZMED.REC.1397.077) and followed the tenets of the Declaration of Helsinki. All patients with open angle glaucoma who were referred to the glaucoma clinic of the Nikoukari Hospital of Tabriz University of Medical Sciences and were candidates for deep sclerectomy were enrolled in the study.
The sampling method was non-random. Inclusion criteria included: patients with open angle glaucoma who did not tolerate anti-glaucoma medications or patients whose IOP was not well controlled with maximum medication and required glaucoma surgery, phakic patients more than 40 years old, patients with proper vision capable of sustaining on the fixation point in the i-Trace analysis device and patients with informed consent.
ExclusionCriteriaIncludedPatients with previous ocular surgery, congenital ocular abnormalities, uveitis, ocular infections, patients with diabetes, or neovascular glaucoma, visual impairments other than refractive errors or mild cataracts (significant lens opacity; 2> LOCS III, Lens Opacification Classification System), pupils less than 4 mm in size after maximum dilatation of the pupil with medication and patients with a need for simultaneous cataract and glaucoma surgeries. After detailing the research purposes of the project, an informed consent form was provided to patients. After signing it, they were enrolled in the study.
All qualified samples underwent the optical wavefrontviai-Trace wavefront analyzer (VFA software version 1.0, Tracey Technologies, Houston, TX) once 1d before surgery and one and three months after surgery.
All of the patients underwent a complete ocular examination before surgery, such as: BCVA by Snellen chart, slit lamp biomicroscopy, intraocular pressure (Goldman Applanation Tonometer), fundoscopy (90 D lens), lens opacity (LOCS III), gonioscopy and the number of drugs was used.
SurgicalInterventionsNon-penetrating glaucoma surgery involves various surgical procedures of which deep sclerectomy was used in this study. The selected patients underwent general anesthesia. After washing the cul-de-sac with povidone/iodine 5% and normal saline solution, 0.2 mL of MMC 0.02% was injected into the sub-Tenon space in the upper cul-de-sac. Then it was distributed by the spatula in the upper quadrant. We then performed the peritomy in the superior quadrant and separated the tenon and conjunctiva with Westcott scissors and rinsed the site with a balanced salt solution. An outer rectangular scleral flap, sized 5×5 mm, approximately 200 μm thick, was dissected about 1-1.5 mm from the clear cornea and followed by an inner 4×4 mm scleral flap under the previous flap. We cut the deep scleral flap and then unroofed the Schlemm’s canal. We separated the Descemet’s membrane and created a trabeculo-descemetic window. The two openings in the Schlemm’s canal were dilated with a slow injection of sodium hyaluronate through a 190-micron cannula. The outer scleral flap was then tightly sutured with 2 nylon 10-0 suture placed in the corners of the flap. Sodium hyaluronate was injected under the flap to temporarily cannulate inner scleral flap and to prevent collapse and scarring in the postoperative period.
After surgery, patients received betamethasone drop (q 2h), which were discontinued for 2mo and chloramphenicol drop (q 6h) were administered for 1mo.
Anti-glaucoma drops were started at any time during the follow-up if IOP was more than 21 mmHg (Goldman Tonometer). Latanoprost was used for the first anti-glaucoma drop and if there was not an acceptable response, a second drop (timolol 0.5%) was used. All patients were followed one day, one week, two weeks, 1mo and three months after surgery.
All patients were evaluated for visual acuity, intraocular pressure (Goldman tonometer), slit lamp biomicroscopy, fundoscopy (90 D lens), bleb morphology at each visit. Bleb morphology of patients were evaluated using the Moorfields Bleb Grading System.
The intent of this study was to evaluate changes in corneal and ocular HOA and the measurement of intraocular pressure and the success rate of surgery within three months after surgical procedure.
A complete success rate was defined as IOP<18 or at least a 20% reduction in IOP from baseline without the use of anti-glaucoma drops at the 3mo follow-up. A relative success rate was defined as IOP<18 or at least 20% reduction in IOP from baseline using one anti-glaucoma drug at the 3mo follow-up. A failure rate was defined as IOP>18 or less than 20% reduction in IOP from baseline after surgery despite maximum drug treatment or the need for further surgical treatment. Any required therapeutic intervention during the follow-up such as starting anti-glaucoma medications was recorded.
StatisticalAnalysisData was analyzed before and after surgery at different times using repeated-measure ANOVA (RMANOVA). Pearson’s correlation coefficient was used to examine relationships between variables. Data were analyzed using SPSS 18 andP<0.05 was considered statistically significant. The results were reported as mean±standard deviation for quantitative and frequency variables (percentages) for qualitative variables.
RESULTS

Figure 1 Changes in the patients’ BCVA.
Twenty-three patients were enrolled in the study. Two patients did not refer to postoperative examinations, and one patient after 1mo of follow-up did not refer to the 3mo follow-up due to a car accident and was excluded from the study. Twenty eyes from 20 patients were followed completely for three months. Patients underwent non-penetrating deep sclerectomy surgery with sub-Tenon injection of MMC. Patients were 3 women and 17 men. The mean age of the patients was 61.9±9.86. There were 10 eyes with primary open angle glaucoma (POAG) and 10 eyes with secondary open angle (SOAG; pseudoexfoliation). Eleven patients had systemic hypertension. The BCVA level of the patients before the surgery was 0.16±0.12 LogMAR, which decreased to 0.19±0.13 LogMAR at 1mo, and then increased to 0.17±0.12 LogMAR at 3mo. The BCVA reduction in the first month was significant (P=0.004), but changes in BCVA were not statistically significant (P=0.16) in the third postoperative month compared to the preoperative period. Changes in the BCVA of the patients are shown in Figure 1 at the 3mo follow-up.
SE before surgery was -0.30±1.47, which increased to-0.37±1.51 at 1mo, then decreased to -0.34±1.48 at 3mo. SE reduction in the first month was significant compared to the preoperative state (P=0.03). However, changes in SE at the 3mo follow-up were not statistically significant (P=0.26).
Changes in Higher-order Aberrations
TotalocularThe HOT RMS before surgery was 0.63±0.17 μm, which significantly increased to 0.69±0.15 μm at the 1mo follow-up (P=0.005) and decreased to 0.67±0.16 μm at the 3mo follow-up, which was not statistically significant compared to the preoperative state (P=0.08). The coma like RMS before surgery was 0.48±0.19 μm, which increased to 0.51±0.15 μm at the one-month follow-up (P=0.90) and decreased to 0.50±0.26 μm (P=1.00) at 3mo, which was not statistically significant at either follow-up. The trefoil RMS before surgery was 0.26±0.08 μm, which increased to 0.27±0.08 μm (P=0.24) at 1mo and decreased to 0.26±0.07 μm at 3mo (P=0.2). These changes were not statistically significant at either period. The spherical like RMS before surgery was 0.35±0.12 μm, which increased to 0.37±0.11 μm at 1mo (P=0.001) and decreased to 0.36±0.11 μm at 3mo (P=0.01). These changes were statistically significant at both time points. There was a moderate correlation between the amount of total HOT RMS and spherical-like total and coma-like total at the 3mo follow-up (r2=0.494,P=0.027). No significant correlation was found between the amount of total HOT RMS and total coma-like and total trefoil, which were (r2=0.067,P=0.78) and (r2=0.115,P=0.63), respectively. The changes in total HOA over three months of follow-up are shown in Figure 2.
Table 1 Changes in higher-order aberrations during 3mo follow-up

ParametersHOTPSpherical-likePComa-likePTrefoilPTotal ocular (μm, RMS) Baseline0.63±0.170.35±0.120.48±0.190.26±0.08 1mo postoperative0.69±0.150.0050.37±0.110.0010.51±0.150.90.27±0.080.24 3mo postoperative0.67±0.170.080.36±0.110.010.50±0.2610.26±0.070.2Corneal (μm, RMS) Baseline0.42±0.180.12±0. 840.25±0.10.34±0.18 1mo postoperative0.44±0.17<0.0010.15±0. 11<0.0010.27±0.080.0060.35±0.150.992 3mo postoperative0.45±0.220.4460.13±0. 090.0040.26±0.10.1480.35±0.311
Spherical-like: Fourth-order Zernike coefficients (C4-4, C4-2, C40, C42, C44); Coma-like: Third-order Zernike coefficients (C3-3, C3-1, C31, C33); Trefoil: Third-order Zernike coefficients; HOT: Higher-order total; RMS: Root mean square.

Figure 2 Changes in total ocular HOT (a), coma like (b), trefoil (c) and spherical like (d) at 3moSpherical-like: Fourth-order Zernike coefficients (C4-4, C4-2, C40, C42, C44); Coma-like: Third-order Zernike coefficients (C3-3, C3-1, C31, C33); HOT: Higher-order total; Trefoil: Third-order Zernike coefficients; RMS: Root mean square.

Figure 3 Changes in corneal HOT (a), coma like (b), trefoil (c) and spherical like (d) at 3moSpherical-like: Fourth-order Zernike coefficients (C4-4, C4-2, C40, C42,C44); Coma-like: Third-order Zernike coefficients (C3-3, C3-1, C31, C33); Trefoil: Third-order Zernike coefficients; HOT: Higher-order total; RMS: Root mean square.
CornealThe corneal HOT RMS before surgery was 0.42± 0.18μm, which significantly increased to 0.44±0.17 μm at 1mo (P=0.001) and decreased to 0.45±0.22 μm at 3mo, which was not statistically significant compared to the pre-surgical state (P=0.446). The coma-like RMS before surgery was 0.25±0.1 μm, which increased to 0.27±0.08 μm in 1mo follow-up (P=0.006) and decreased to 0.26±0.1 μm, which was not statistically significant compared to pre-surgical state (P=0.148). The corneal trefoil RMS before surgery was 0.34±0.18, which increased to 0.35±0.15 μm (P=0.992) at 1mo and reached 0.35±0.31μm at 3mo (P=1). These changes were not statistically significant at either time point. The spherical-like RMS before surgery was 0.12±0.084 μm, which increased to 0.15±0.11 μm at 1mo (P=0.001) and decreased to 0.13±0.09 μm at 3mo (P=0.004) which was statistically significant. There was no significant correlation between corneal HOT RMS and other corneal aberrations such as spherical like, coma like and trefoil at the 3mo follow-up (r2=12.0,P=0.59), (r2=0.06,P=0.78) and (r2=0.25,P=0.28). There was no significant correlation between total HOT RMS and other corneal aberrations. There was a moderate correlation between total spherical-like RMS and corneal spherical-like at the 3mo follow-up (r2=0.58,P=0.006). The changes in corneal HOA over the 3mo of the follow-up are shown in Figure 3. The numerical values of the total and corneal higher-order aberrations are shown in Table 1, by time.
Age had no significant statistical effect on changes in total HOT or corneal HOT (P=0.625 andP=0.559, respectively). IOP had no significant effect on changes in total HOT or corneal HOT (P=0.315 andP=0.616, respectively). The IOP before surgery was 24.05±3.07 mmHg with a mean of 2.85±0.67 medication which reached 11.75±3.33 mmHg at a week and 12.2±3.83 mmHg with 0.75±0.72 medication at 1mo and 12.30±3.32 mmHg with 0.70±0.09 medication at 3mo. The IOP reduction was statistically significant at all periods of the follow-up (P<0.001). IOP changes over the 3mo follow-up are shown in Figure 4. The numerical values of IOP, BCVA and SE are given in Table 2.
Table 2 Changes in IOP, BCVA and SE at 3mo follow-up
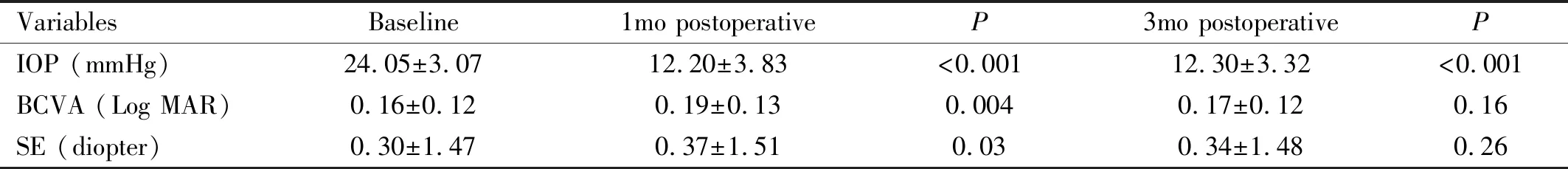
VariablesBaseline1mo postoperativeP3mo postoperativePIOP (mmHg)24.05±3.0712.20±3.83<0.00112.30±3.32<0.001BCVA (Log MAR)0.16±0.120.19±0.130.0040.17±0.120.16SE (diopter)0.30±1.470.37±1.510.030.34±1.480.26
IOP: Intraocular pressure; BCVA: Best corrected visual acuity; SE: Spherical equivalent.
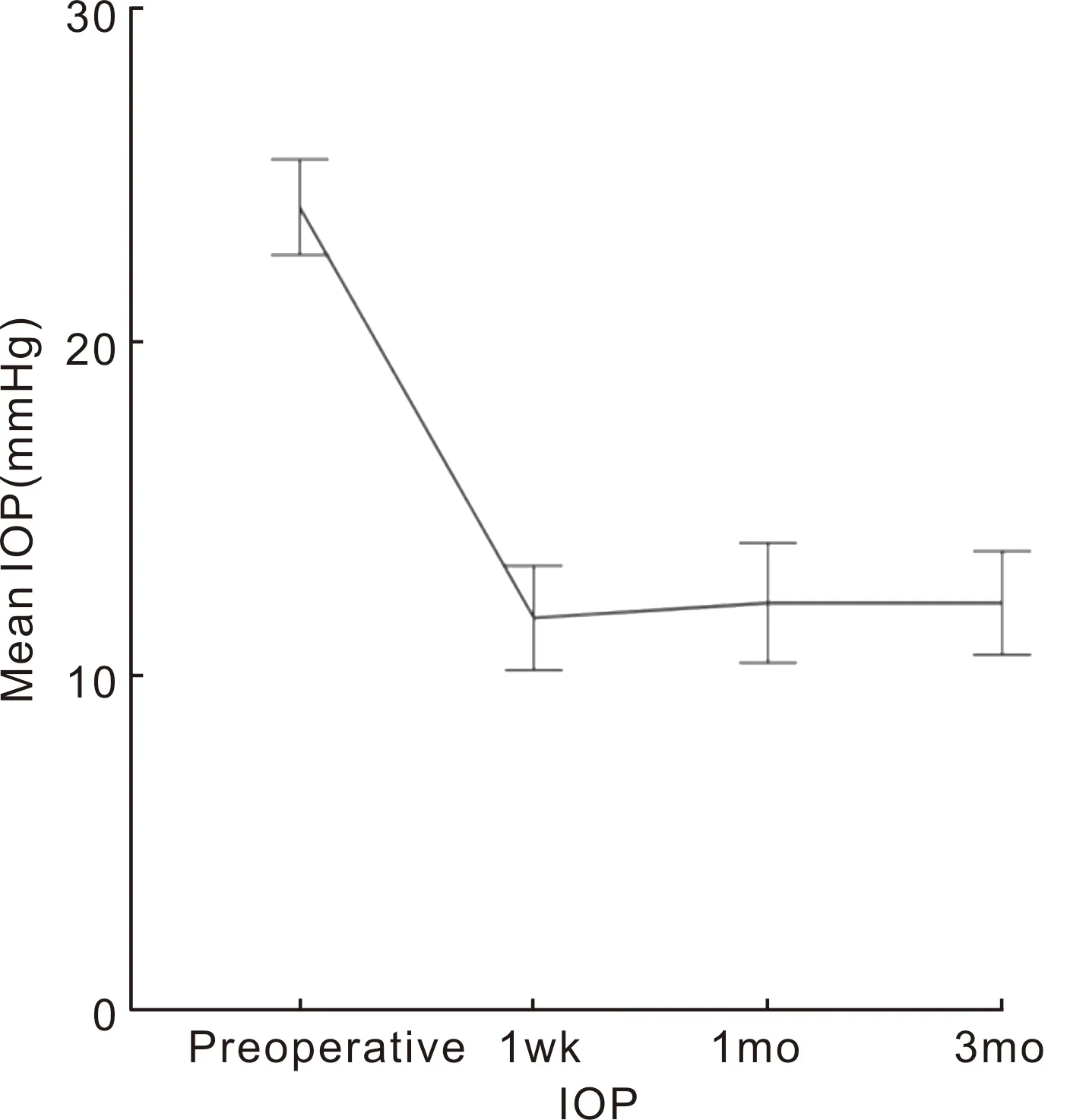
Figure 4 IOP variations before and after deep sclerectomy during 3mo.
Based on Moorfields Bleb Grading System, the bleb vascularity in the first week of the follow-up was significantly decreased during the first and third months after surgery (P<0.001). The bleb height was 2.30±0.47 at the first week of the follow-up, decreased to 1.25±0.44 and increased to 1.70±0.47 in the first and third months after surgery, respectively, which were statistically significant (P=0.001 andP<0.001, respectively). The bleb Extension a (central demarcated area of the bleb) in the first week of the follow-up was 3.15±0.67 and reached 3.45±0.76 in third month, and which were statistically significant (P=0.009). The bleb Extension b (the maximal area of the bleb) of the patients was 3.35±0.95 in the first week of the follow-up and reached 3.75±0.72 at the third month. The changes were statistically significant (P=0.003). Sixteen eyes (80%) had overall success, 14 eyes (70%) had complete success, 2 eyes (10%) had relative success and 4 eyes (20%) were failures within the three month follow-up period. Bleb extension, vascularity and height are shown in Figures 5A, 5B and 5C, respectively.
Of the 20 patients, one had mild early leakage in the bleb site after surgery, which was resolved with tissue adhesive and bandage soft contact lens (Bausch and Lomb) after 1wk postoperatively and no resuturing was required. Endophthalmitis or hypotony maculopathy was not reported in any of the patients. The percentage of complete and relative success and the failure rate is shown in Figure 6.
DISCUSSION
The most important factor that increases the risk of glaucoma surgery failure is scar formation at the level of the conjunctiva, episclera, or Tenon’s capsule in the bleb formation site, which prevents the eye from reaching the target IOP. Today, the use of anti-metabolites with a delay in wound healing response results in decreasing scar and increasing surgical success rates. Studies have been done to reduce the complications of anti-metabolites regarding the time, appropriate concentration and the site used[20-23]. Typically, sponge soaked MMC is used before or after scleral flap dissection in glaucoma surgery, which can prolong the duration of surgery and cause localized or cystic bleb[24]. In previous studies, MMC has been used in different ways and at different levels (under the conjunctiva, under and around the sclera flap)[27]. sub-Tenon injection of MMC allows MMC contact with a wider range of episclera, and since it only applies to the desired tissue site, it requires less concentration of the drug, which ultimately improves the function and morphology of the bleb. Considering that not many studies have been done regarding the effect of sub-Tenon injection of MMC in non-penetrating deep sclerectomy surgery, we decided to study the effect of sub-Tenon injection of MMC on the surgical success rate.
Leeetal[25]conducted a retrospective study examining trabeculectomy and phacotrabeculectomy surgeries augmented with intra-Tenon injection of MMC. Twenty-three cases of combined phacotrabeculectomy and 85 cases of trabeculectomy surgeries were augmented with 0.15 mL of MMC injection at a concentration of 0.2-0.5 mg/mL Intra-Tenon in each case. The mean IOP was 23.6±5.8 before surgery and decreased to 12.2±3.9 after 12mo of follow-up. Transient complications such as hypotension, bleb leak and choroid detachment were observed in 14.8%, 5.6% and 15.7%, respectively. This study showed that intra-tenon injection of MMC is an effective way to reduce IOP in patients.
In a retrospective study, Micheleetal[28]compared the effect of trabeculectomy surgery augmented with intra-Tenon injection of MMC at the beginning of trabeculectomy surgery using an MMC soaked sponge. The success rate of surgery was defined as IOP≤21 mmHg or IOP≥20% reduction from baseline with and without medication therapy and without the need for reoperative treatment of glaucoma. 231 eyes were included in this study. During a three-year follow-up of patients, the success rate of surgery was 80% in the sub-Tenon injection group and 70% in the MMC soaked sponge group. The use of anti-glaucoma drugs in the intra-Tenon of MMC group was lower in the three-year follow-up period (0.49vs0.94). This study showed that intra-tenon injection of MMC in trabeculectomy surgery led to a reduction in IOP and the need for medication therapy and the development of diffuser bleb compared to MMC soaked sponge.
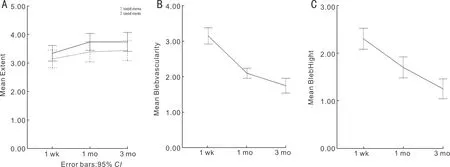
Figure 5 A: Bleb extension variation during 3mo;B: Bleb vascularity variation during 3mo;C: Bleb height variation during 3mo.
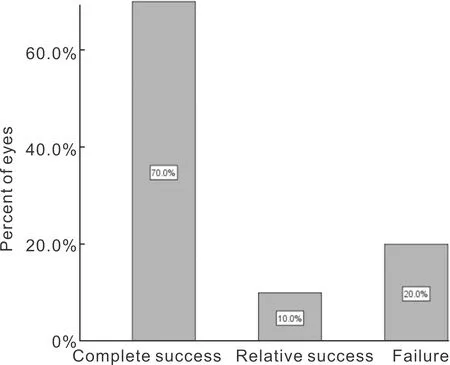
Figure 6 Percentage of eyes with complete and relative success and failure by in 3mo follow-up.
Pakravanetal[27]studied trabeculectomy in a randomized clinical trial comparing the effect of using sub-Tenon injection of MMC and soaked sponge. Patients were included in the study from 2013 to 2015. Eighty patients with open angle glaucoma were divided into two groups, group A: The upper cul-de-sac injected 0.1 mL of 0.01% MMC in the sub-Tenon space and group B: Sponge soaked MMC 0.02% was placed under conjunctiva for 1-3min. Patients were followed-up at 1, 3, and 6mo after surgery. The mean IOP before the operation in group A was 21.8±5.1, which decreased to 10.3±3.7 and was 21.8±5.1 in group B, which decreased to 10.8±3.5. The success in both groups was 82.5%. The blebs tended to be more diffuse, less vascularized and shallower in the sub-Tenon injection group. This study showed that sub-Tenon injection of MMC is a safe and effective alternative to the soaked sponge method and produces more favorable bleb morphology.
In a clinical trial study conducted by Mostafaeietal[29]. At the same center, MMC was compared with Bevacizumab-Methylcellulos mixture (BMM). This study showed that MMC can better control intraocular pressure in these patients.
In previous studies, the effect of trabeculectomy on ocular aberrations was identified and it was mentioned as a cause of decreased vision and patient dissatisfaction after surgery. In this study, we examined the total and higher-order aberrations following non-penetrating deep sclerectomy surgery with sub-Tenon injection of MMC. The total ocular HOT and total ocular spherical-like increased significantly during the 1mo follow-up after surgery and decreased over three months. Changes in total ocular trefoil and total ocular coma like have not been statistically significant at all periods after surgery. The corneal HOT RMS and coma and spherical-like increased significantly 1mo after surgery and decreased at the 3mo follow-up. The corneal trefoil changes were not statistically significant at all periods after surgery.
Jungetal[26]studied high-order aberration changes after combined phacotrabeculectomy and phacoemulsification. In this study, 38 eyes from 38 patients with cataract and glaucoma underwent trabeculectomy and phacoemulsification with MMC. 34 eyes from 34 patients with cataract underwent phacoemulsification. In the group that underwent combined phacotrabeculectomy surgery, IOP decreased significantly and total spherical-like HOA and total coma-like increased two weeks after phacotrabeculectomy and then decreased at three months. Corneal aberration and internal aberration also increased during two weeks after phacotrabeculectomy and then decreased at three months. Total spherical-like HOA and total coma-like and internal aberrations decreased in the phacoemulsification group after surgery.
In a retrospective study by Joetal[5]higher-order aberration changes were examined after trabeculectomy with sponge-soaked MMC (0.4 mg/mL). Sixty-three eyes from 63 patients were enrolled in the study. Patients were divided into phakic and pseudophakic groups. Patients’ HOA was evaluated before surgery and at the first, second and fourth weeks after surgeryviai-Trace analyzer. Total ocular coma-like and HOT in the phakic group showed a significant increase in the first week after surgery, however, it was not significant at the second and fourth weeks, and was not significant in the pseudophakic group at any period after surgery. Corneal HOA in the phakic group showed a significant increase at the first and second weeks after surgery, but it was not significant at the fourth week. Corneal HOA in the pseudophakic group was not significant at any period after surgery. Internal HOA had a significant increase in first, second and fourth weeks after surgery in the phakic group, but it was not significant in the pseudophakic group. This study showed that HOA increased significantly in the phakic group at one and two weeks after trabeculectomy. There was no correlation between HOA changes and age, IOP or depth of AC, which is consistent with our study.
Razmjooetal[7]examined corneal higher-order aberrations and anterior chamber parameters after trabeculectomy. In this retrospective study, from 2011 to 2012, 40 eyes from 40 patients were enrolled. One group underwent limbal- based trabeculectomy and the other group underwent fornix-based trabeculectomy. Corneal keratometry, central corneal thickness, anterior chamber depth, anterior chamber volume, and higher-order aberrations were evaluated using Pentacam before surgery and at three months after surgery. Results showed a significant reduction in the intraocular pressure after surgery in both groups compared with preoperative values (P<0.050). No significant difference was seen in corneal keratometry, anterior chamber depth, anterior chamber volume, corneal thickness or total RMS and trefoil and coma after surgery in both groups (P>0.050). In general, the results of this study showed that corneal keratometric parameters and postoperative anterior chambers were not significantly different from preoperative values in patients with glaucoma after trabeculectomy and most of the HOAs affecting quality of vision did not significantly change after limbal-based or fornix-based trabeculectomy.
In another study, Fukuokaetal[11]examined the effect of trabeculectomy on corneal and ocular higher-order aberrations. Thirteen eyes were enrolled. Ocular coma-like and total ocular HOA significantly increased at 1mo after trabeculectomy, but returned to the normal level three months after surgery. The mean SE was not changed by surgery. A strong correlation between ocular total RMS and ocular coma-like was observed within 1mo. A moderate correlation was observed between corneal and ocular spherical-like at the 1mo follow-up, which is consistent with our study.
In summary, the reduction in IOP was significant at all periods of the follow-up after deep sclerectomy with sub-Tenon injection of MMC and leading to bleb formation with appropriate morphology and no serious complications observed after surgery. Corneal and ocular higher-order aberration increased within 1mo after deep sclerectomy and then decreased over 3mo, with no statistically significant changes compared to preoperative values. Certainly the role of the biomechanics of the cornea, the hysteresis of the biological tissues in possible causes explaining the changes observed in the optical properties of the cornea and their impact on the optical aberrations need to be elucidated.
BCVA and SE changes were not statistically significantat the 3mo follow-up compared to preoperative values. Patients’ age and IOP had no significant effect on changes in total ocular HOT and corneal HOT aberrations. The limitations of this study were low number of samples, short follow-up period for evaluating the success rate of surgery and the internal optic HOA was not evaluated and this present study was not a comparative study. Another limitation of this study is that our study has only discussed cases of OAG and did not investigate cases with ACG or other subtypes.
Further comparative studies with more samples and evaluation of internal aberrations are recommended. Moreover corneal and ocular biomechanics and their relationship with aberrations can be evaluated in future studies.