Single- and double-dose of platelet-rich plasma versus hyaluronic acid for treatment of knee osteoarthritis: A randomized controlled trial
2019-11-12MehdiTavassoliNasserJanmohammadiAkramHosseiniSorayaKhafriSeyedMokhtarEsmaeilnejadGanji
Mehdi Tavassoli, Nasser Janmohammadi, Akram Hosseini, Soraya Khafri, Seyed Mokhtar Esmaeilnejad-Ganji
Abstract
Key words: Platelet-rich plasma; Hyaluronic acid; Osteoarthritis; Knee; Pain
INTRODUCTION
Osteoarthritis is the most common articular disease, and it is an important cause of disability in the elderly[1,2].The knee is the most frequent joint affected by osteoarthritis[3].Osteoarthritis is a multifactorial chronic disease that starts with breakdown of joint cartilage and leads to decrease in joint space, subchondral sclerosis, synovitis and peripheral osteophytes formation[4,5].It was estimated that more than 10% of the people aged ≥ 60 years suffer from this disease, and it is a major expense for all healthcare systems[6,7].Clinical manifestations of the disease include functional pain and joint stiffness.Morning stiffness usually lasts less than 30 min followed by gel phenomenon that is a transient joint stiffness due to short-term immobility[8,9].
Current treatments for osteoarthritis include non-pharmacologic treatment, such as physical activity[10-12], and pharmacologic treatment, such as non-steroidal antiinflammatory drugs, glucocorticoids and hyaluronic acid.These treatments aim to decrease pain and inflammation, but these drugs have restricted and short-term effects on control of symptoms and the patient’s quality of life[13,14].Platelet-rich plasma (PRP) is a plasma that is prepared from each patient’s own blood, and it has a higher platelet concentration in comparison to normal plasma.PRP injection is a simple, low cost and minimally invasive procedure that provides concentrated growth factors for use as an intra-articular injection[15].These growth factors are said to stimulate the healing of cartilage and thus improve arthritis[16,17].Some studies alluded to the potential effect of PRP in treatment of chronic tendonitis, tennis elbow,chronic rotator cuff tendinopathy, jumper’s knee, acute Achilles tendon rupture,muscle rupture, osteochondritis and osteoarthritis and meniscus repair[18-22].The positive effects of PRP in improvement of knee osteoarthritis have been reported in some studies[23-26].Studies have reported the effects of PRP on the proliferation of mesenchymal root cells and their chondrocyte differentiation in anin vitroenvironment[27,28], but evidence about the clinical use of PRP in the treatment of knee osteoarthritis is still insufficient.
Hyaluronic acid is a polysaccharide compound that includes glucuronic acid and acetylglucosamine.In osteoarthritis, the concentration and molecular weight of hyaluronic acid are reduced, and this is the basis of hyaluronic acid injection.Hyaluronic acid provides viscoelasticity of synovial fluid and stimulates formation of endogenous hyaluronic acid[29,30].In addition to its effects on viscoelasticity, hyaluronic acid may be effective for the treatment of osteoarthritis by biochemical effects, such as stimulation of formation and accumulation of proteoglycan, inhibition of inflammatory mediators and analgesic effect[29,31,32].However, because there are inadequate data on the effects of either different doses of PRP or hyaluronic acid in patients with osteoarthritis, we aimed in this study to compare the therapeutic efficacy of intra-articular injection of two different doses of PRPversushyaluronic acid in the management of patients with osteoarthritis of the knee.
MATERIALS AND METHODS
This single-blinded parallel randomized controlled trial study was conducted on patients aged 40- to 80-years-old with knee osteoarthritis who were referred in 2018 to Shahid Beheshti teaching hospital affiliated to Babol University of Medical Sciences,Babol, Northern Iran.
The inclusion criteria were as follows:(1) patients with diagnosis of knee osteoarthritis as defined by the criteria of the American College of Rheumatology[33];(2) patients who were staged using the Ahlback radiological grading; (3) patients having bilateral knee osteoarthritis with the same Ahlback grade; and (4) all knees with full range of motion.
The exclusion criteria were as follows:(1) history of diabetes; (2) history of other joint diseases in the knee, such as rheumatoid arthritis or gout; (3) history of knee surgery; (4) history of knee fracture; (5) intra-articular injection of corticosteroids during the previous 2 wk; (6) intra-articular injection of other drugs, such as hyaluronic acid over the previous 1 year; (7) contraindications for intra-articular injection, such as thrombocytopenia, coagulopathy, articular infection of knee, skin infection in the injection site, impairment of immunity (e.g., acquired immune deficiency syndrome or receiving immunosuppressive medication) and severe intraarticular effusion (in this case, intra-articular injection was started after treatment and cure of effusion); and (8) patients with Ahlback grade 3 or more.
All of the patients were examined by the senior orthopedic surgeon, who was blinded to the intervention groups.Plain radiographs were then taken of the knees with anterior-posterior and lateral views.Drug treatments (such as non-steroidal antiinflammatory drugs, corticosteroids and other anti-inflammatory drugs) and nondrug treatments (knee physiotherapy with modalities, such as transcutaneous electrical nerve stimulation, laser,etc) were stopped for the 48 h before study interventions.
Ahlback radiological grading of knee osteoarthritis is classified as follows[34,35]:I:joint space narrowing < 3 mm; II:joint space obliterated or almost obliterated; III:minor bone attrition (< 5 mm); IV:moderate bone attrition (5–15 mm); and V:severe bone attrition (> 15 mm).
The patients’ information was collected by a checklist, including age, gender,weight, height, body mass index and Ahlback grade.All necessary laboratory tests(complete blood count, erythrocyte sedimentation rate, C-reactive protein) were conducted in the laboratory of Shahid Beheshti hospital.
Outcome measures
For the evaluation of function in all patients, the Persian version of the Western Ontario and McMaster Universities Arthritis Index (WOMAC) and Visual Analogue Scale (VAS) questionnaires were completed by an interview performed by the resident doctor in orthopedic surgery.The WOMAC index consists of 27 questions about three parameters, including pain (five questions), stiffness (two questions) and physical function (twenty questions).Each question is scored from 0 (none) to 4(extreme).The sum of scores of subscales is the total WOMAC score (ranging from 0 to 108).Higher scores indicated worse conditions.Validity and reliability of WOMAC for knee osteoarthritis have been documented in Iran[36,37].The VAS index also assessed the patients’ pain.Its scores range from 0 (no pain) to 10 (worst possible pain)[38,39].
The primary outcome for this study was defined as the percentage of patients experiencing at least a 30% decrease in the summed score for the WOMAC pain subscale from baseline to wk 12 of the intervention.Generally, clinically meaningful pain relief is defined as ≥ 30% reduction in pain intensity from baseline[40,41].The secondary outcomes included change in joint stiffness, physical function and total WOMAC.We also evaluated the patients for pain by VAS score, and this was a secondary outcome.Additionally, we assessed a reduction of ≥ 50% in the scales as another secondary outcome.These data were recorded before injection and at 4 wk, 8 wk and 12 wk after injection.
Sample size calculation
The sample size was estimated as at least 30 patients in each group by a superiority margin of δ = -0.15 that was based on clinical judgement with 80% power, type I error rate of 5% and percentage drop of 10%.The proportion of the primary study outcome in PRP single-dose and hyaluronic acid groups was considered as 35% and 20%.
PRP preparation
The PRP preparation was performed by the Rooyagen kit (Arya Mabna Tashkhis Corporation, Tehran, Iran).For preparation of the PRP, about 40 mL of venous blood was drawn from antecubital vein with an 18-gauge needle.Then 5 mL acid-citratedextrose solution was added as an anticoagulant.The blood sample was then centrifuged for 15 min at 1500 rpm, leading to two different layers, including RBC sediment (inferior layer) and plasma (superior layer).The plasma was separated and then centrifuged for 7 min at 3500 rpm, which created two new (superior and inferior)layers with the lower white sediment containing platelets.Then the upper layer was removed, and the remaining 4-6 mL was mixed with the white platelet sediment by shaking.The final product was 4-6 mL of PRP.A laboratory analyzer Sysmex KX 21(Sysmex Corporation, Kobe, Japan) assessed the quality and quantity of each batch of PRP.
Randomization and intervention
The subjects included in the study were divided by random allocation using computer generated numbers into three groups:(1) group PRP-1 with 31 participants (62 knees)who received a single injection of PRP; (2) group PRP-2 with 33 participants (66 knees) who received two injections of PRP; and (3) group hyaluronic acid with 31 participants (62 knees) who received three injections of hyaluronic acid.
Each patient received the same randomized intra-articular injection into both knees.The injection site on the skin was prepped and draped and under aseptic conditions.PRP was injected using a 22-gauge needle with classic inter-articular approach(through the superolateral corner of patella or mid-portion of patella while the knee is extended).After 15-20 min rest, the patients were asked to flex and extend their knees so that PRP was completely distributed in the joint before becoming a gel.For group PRP-2 (double-dose of PRP), the second injection was performed after an interval of 3 wk.Patients in group hyaluronic acid received three injections of Hyalgan brand hyaluronic acid as a prepared needle, which contains a high molecular weight (500-730 kilodalton) fraction of purified sodium hyaluronate (30 mg/2 mL).Three Hyalgan injections were performed at 1-wk intervals.Before starting each procedure, the patients were evaluated for range of motion on knee joints and also by VAS and WOMAC questionnaires.The patients could use acetaminophen tablets (325 mg) if they experienced pain during the study.They could not use this analgesia for at least 12 h before being examined for follow-up.
Statistical analysis
The collected data were analyzed using SPSS statistical software.The descriptive analysis was used for the determination of the frequency, percentages, mean and standard deviation.Normality of the data was tested using the Kolmogorov-Smirnov test.For comparing the data before and after the treatment with normal distribution,pairedt-test, independentt-test and ANOVA test were applied.To assess the nonparametric data, Wilcoxon signed rank, Mann–Whitney and Kruskal–Wallis were used.Chi-square test was used for qualitative variables.AP-value of < 0.05 was considered to be significant in all tests.Linear and box plot charts were prepared to illustrate the results.
Ethical issues
The informed written consent was provided by all participants.The patients’information was kept confidential.This study was approved by the Ethical Research Com-mittee of Babol University of Medical Sciences (code:IR.MUBABOL.HRI.REC.1397.082).This trial was registered in the Iranian Registry of Clinical Trials with the number IRCT20180129038548N1.
RESULTS
A total of 129 patients were screened initially, of whom 34 were excluded due to failing to meet inclusion criteria or declining to participate.Finally, 95 patients underwent randomization.The flow of subjects from evaluation to participation is shown in the Consolidated Standards of Reporting Trials diagram (Figure 1).Three patients from group PRP-1, five patients from group PRP-2 and four patients from group hyaluronic acid were lost during follow-up.Hence, the final study population for analysis contained 28 patients in groups PRP-1 and PRP-2 and 27 patients in group hyaluronic acid.
The baseline characteristics of the patients are shown in Table 1.There were no significant differences between the groups in age, gender, height, weight, BMI,Ahlback grading, WOMAC score and VAS pain score.
Clinical outcomes
The percentage of patients experiencing at least a 30% and/or 50% decrease in the summed score for VAS pain and all WOMAC subscales from baseline at each followup are shown in Table 2.Analysis of the primary outcome showed that the response rate to a single dose of PRP was 85.7% and to hyaluronic acid was 0% over the 12 wk of follow-up (P< 0.001).This significant difference was also observed when comparing first and second follow-up between the groups, and the two groups of PRP had a significantly higher response rate compared to the hyaluronic acid group.For group PRP-1, no significant differences were identified in the percentage of patients experiencing at least a 30% and/or 50% decrease in the summed score for the WOMAC pain subscale between knees with Ahlback grade 1 and 2 from baseline at each follow-up.It was observed for group II as well.
The mean scores for all WOMAC and VAS pain parameters decreased significantly in the three groups from baseline at wk 4.However, it started a slightly increasing trend thereafter.There were significant differences in percentage change in the mean scores from baseline to wk 4 between the three groups.Group PRP-2 had the highest decreases in the mean scores from baseline to wk 4, which were significantly higher than group PRP-1 and group hyaluronic acid.Group PRP-1 also had significant decreases in the mean scores in comparison with group hyaluronic acid at wk 4.Percentage change in the mean scores was highest in group PRP-2 compared with groups PRP-1 and hyaluronic acid and was significantly higher in group PRP-1versusgroup hyaluronic acid at other follow-ups as well.The findings are shown in Table 3 and Figures 2-6.
Among the patients with Ahlback grade 1, the percentage change in scores from baseline for VAS pain score and all WOMAC subscales at each follow-up was significantly higher for group PRP-2 in comparison with group PRP-1.These differences were also found in the patients with Ahlback grade 2.
Over the study period, no major adverse events or complications were observed in the patients, and mild worsening of pain was noted in seven patients in the PRP groups, which was resolved by doses of acetaminophen.
DISCUSSION
In this study, we attempted to compare the clinical outcomes of PRPversushyaluronic acid injections in patients with bilateral knee osteoarthritis.We divided patients with Ahlback grade 1 or 2 osteoarthritis into the three groups of single and double injection of PRP and three injections of hyaluronic acid.All the patients were followed-up for 3 mo.We used WOMAC and VAS pain scores to evaluate the clinical outcomes.We found that the efficacy of PRP (single or double injection) and hyaluronic acid started from intervention and continued until wk 4 and then started to decrease until wk 12.In other words, the highest efficacy of PRP was seen in both groups at wk 4 with about a 50% decrease in the symptoms compared with about a 25% decrease for those who had received hyaluronic acid.The efficacy of PRP treatment was significantly greater than the hyaluronic acid group at all follow-up times.In addition, two injections of PRP were more effective at each follow-up than a single injection.We did not witness any major complications during the follow-up.No similar studies exist from our region.Therefore, these data are beneficial in this point as well.

Figure 1 CONSORT flowchart.
Few studies have been published comparing these treatments for osteoarthritis of the knee.In a recent systematic review, which collected the data related to the studies comparing outcomes between PRP and hyaluronic acid interventions, the reported studies were mostly in agreement with our research, showing that PRP injection is more effective for the treatment of osteoarthritis of the knee, especially in patients with lower grades of arthritis[42].Two articles did not show any superiority of treatment with PRP over hyaluronic acid[43,44].In our investigation, the trend of efficacy of PRP was demonstrated to continue until the first month after treatment with a decline thereafter.However, there was still a significant difference in the mean scores between follow-ups and baseline.However, in the study by Cerzaet al[45], this benefit continued until the last follow-up at mo 6 without an eventual decline in efficacy.The systematic review by Diet al[42], showed that PRP could improve the WOMAC score at a minimum of 24 wk.However, PRP had no benefit over the control group when assessed by other pain measures, such as the International Knee Documentation Committee, the Knee Injury and Osteoarthritis Outcome Score and VAS[42].When reviewing the literature, it becomes clear that there are variations between the individual studies in terms of number of patients, grading of osteoarthritis (Kellgren-Lawrence[30,43-47]or Ahlback[48]classification), length of followup (variable between 6 mo[30,45,48]and 12 mo[43,44,46,47], outcome scores used (WOMAC,Lequesne[45-49], VAS, the Knee Injury and Osteoarthritis Outcome Score[15,30,44,48,49]and number of PRP injections (one[15], two[46], three[30,43,44,47,48]or four[45]).Hence, the results can only be compared with caution.
One of the mechanisms by which PRP could improve the osteoarthritis of the knee is reported to be its anti-inflammatory effect.It has been shown that PRP can decrease the pro-inflammatory cytokines of interleukin-1 beta and tumor necrosis factoralpha[50].Leukocytes in PRP have been thought to have a role in anti-inflammatory activity, immune regulation and promotion of angiogenesis[51].However, potential harmful effects of leukocytes on cartilage regeneration through the NF-κB pathway (a major pathway involved in the pathogenesis of osteoarthritis) have also been noted[52].Therefore, further experimental and clinical studies are needed to clarify this molecular mechanism of PRP against osteoarthritis.It has been demonstrated that inactivated PRP increased formation of bone and cartilagein vitroandin vivo.Nonactivated PRP was also reported to have an anabolic effect on proliferation of mesenchymal stem cells[53].In addition, thrombin activation of PRP has an inhibitory action on chondrogenesis and osteogenesis[54].Growth factors in PRP potentially affect tissue repair and growth through immigration and cell proliferation, angiogenesis,collagen production and stimulation of articular cartilage anabolism.They may slow down the catabolic process and decrease the synovial membrane hyperplasia[55,56].It was pointed out that plasma rich in growth factors may also decrease NF-kB activation[57].Additionally, platelet-derived growth factor has been stated to promote chondrocyte proliferation and the maintenance of their hyaline-like phenotype[47].Fibrin is another factor that exists in PRP, which is used as a network for the differentiation of root cells and biological glue[58,59].

Table 1 Comparison of baseline characteristics of the patients in the three groups
One limitation of the present study is the lack of a control group that was treated with corticosteroids for comparison.The second one is the short-time period of study.Future studies with longer follow-up are suggested to evaluate long-term efficacy and potential compactions.We also propose that future studies use magnetic resonance imaging to assess and quantify cartilage regeneration, if costs and ethical issues allow.
In conclusion, the results of this study showed that PRP is a safe and efficient therapeutic option for treatment of early stages of knee osteoarthritis by reducing the symptoms and recovering articular function.PRP was indicated to be significantly better than hyaluronic acid.We also found that the efficacy of PRP increases after multiple injections.More studies with longer follow-up and a double-blind comparison of PRP with corticosteroids are suggested for the future.
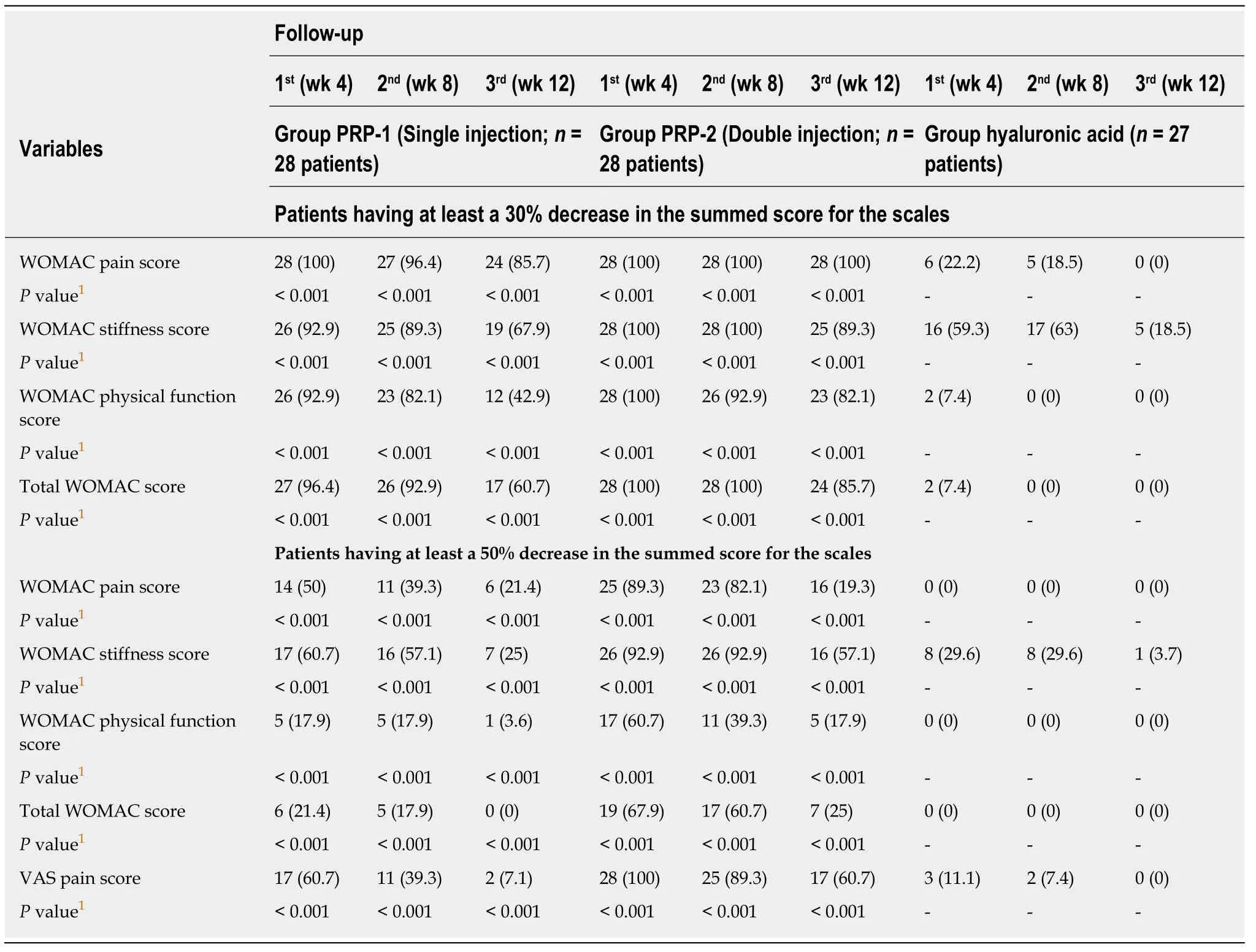
Table 2 Number of patients having at least a 30% and 50% decrease in the summed score for the Western Ontario and McMaster Universities Arthritis Index and Visual Analog Scale, n (%)
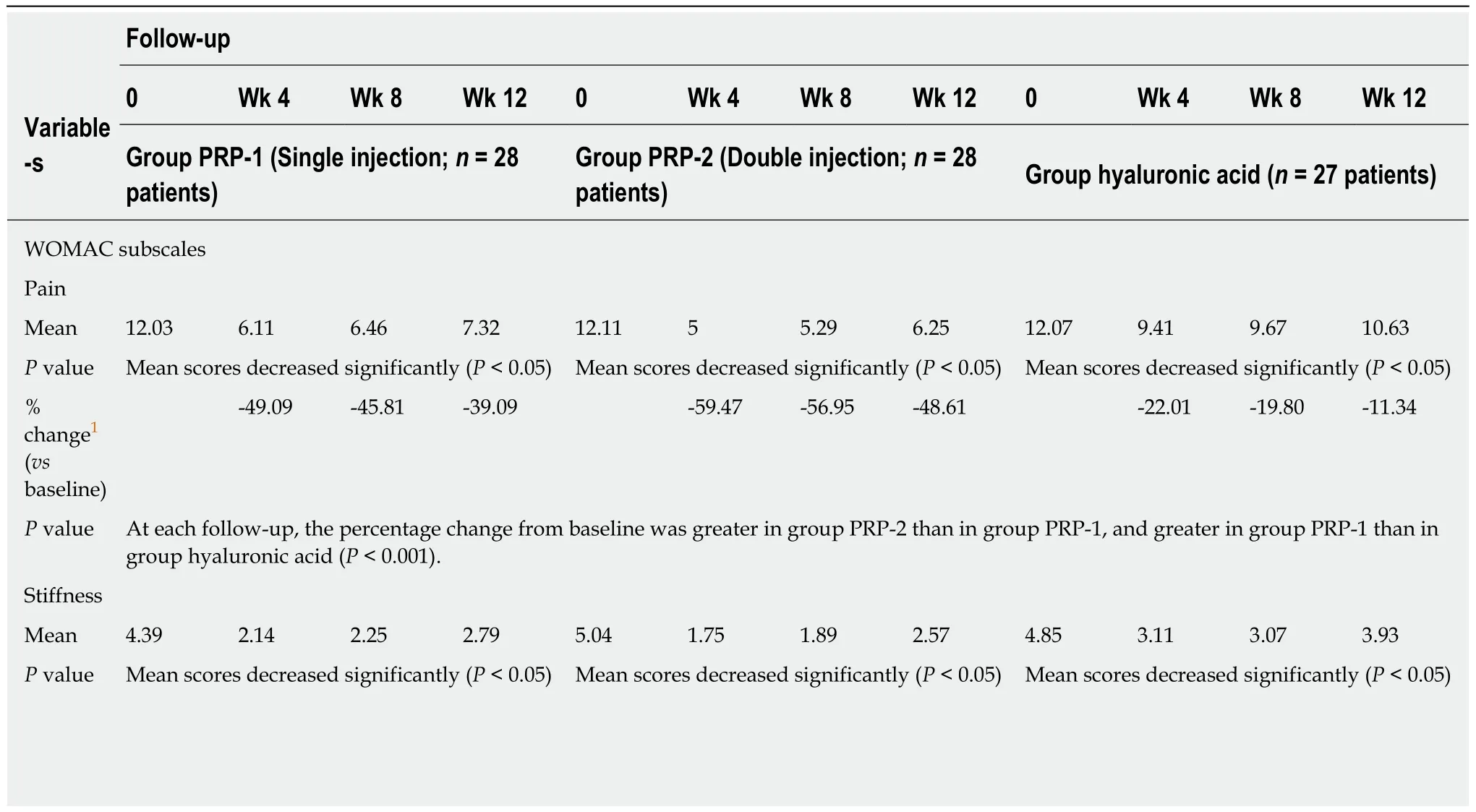
Table 3 Comparison of mean scores and percentage change in each parameter of the Western Ontario and McMaster Universities Arthritis Index and Visual Analog Scale with baseline at each follow-up for the three groups

1Negative percent shows improvement from baseline.VAS:Visual analog scale; WOMAC:Western Ontario and McMaster Universities Arthritis Index.
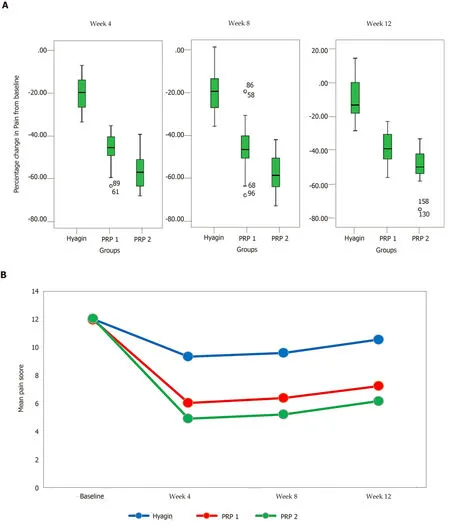
Figure 2 Comparison of the pain score indices between the three intervention groups at baseline and subsequent follow-ups.
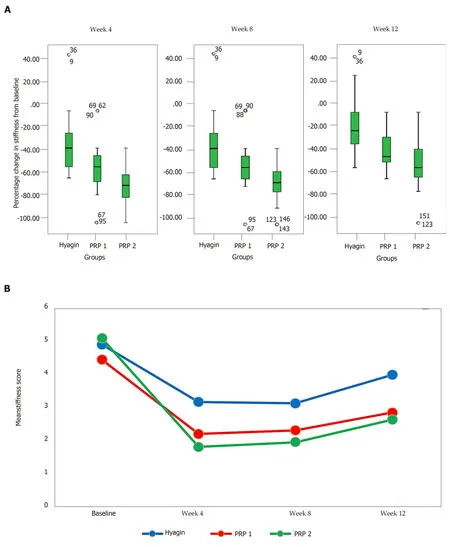
Figure 3 Comparison of the stiffness score indices between the three intervention groups at baseline and subsequent follow-ups.
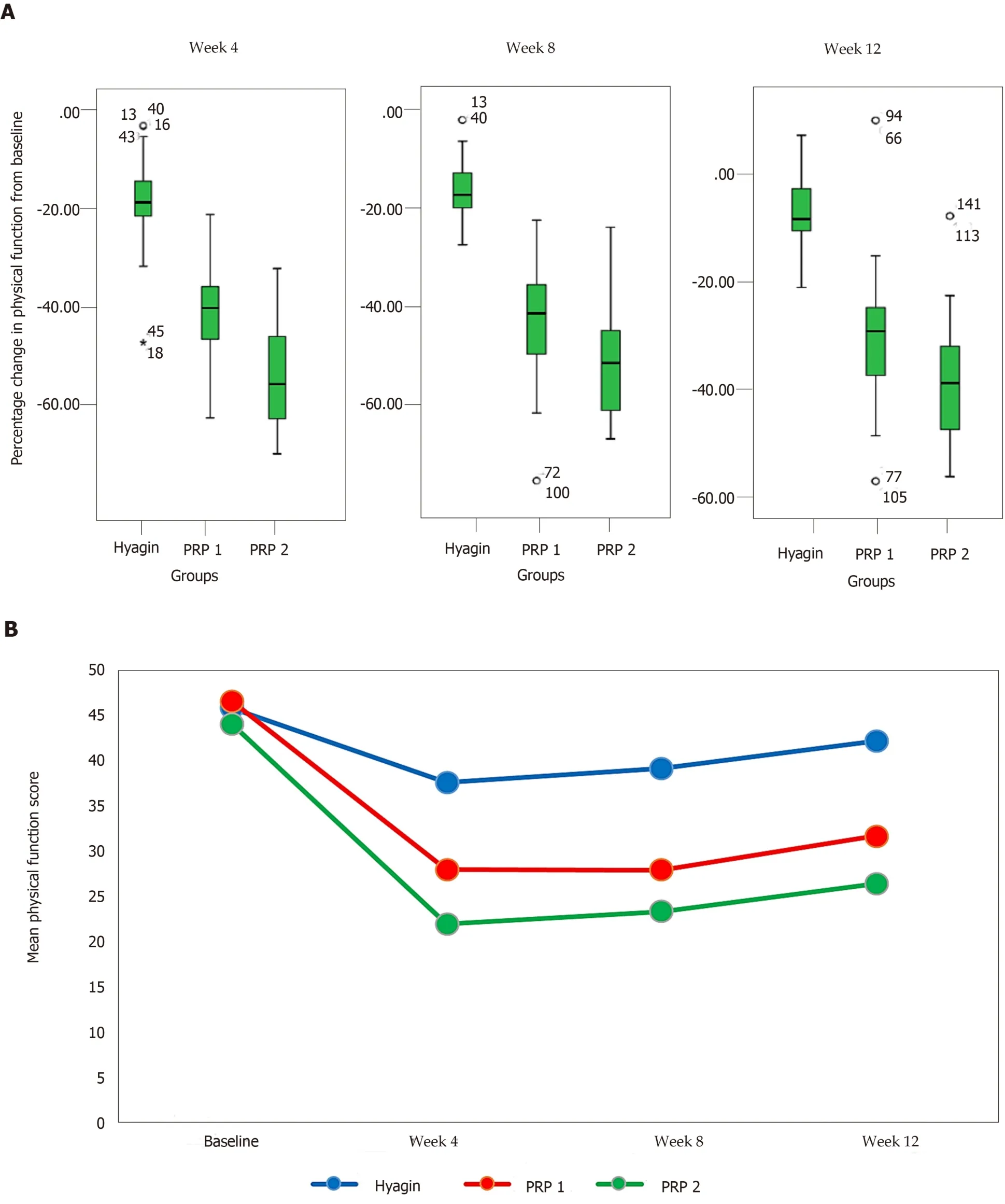
Figure 4 Comparison of the physical function score indices between the three intervention groups at baseline and subsequent follow-ups.

Figure 5 Comparison of the total Western Ontario and McMaster Universities Arthritis Index scores between the three intervention groups at baseline and subsequent follow-ups.
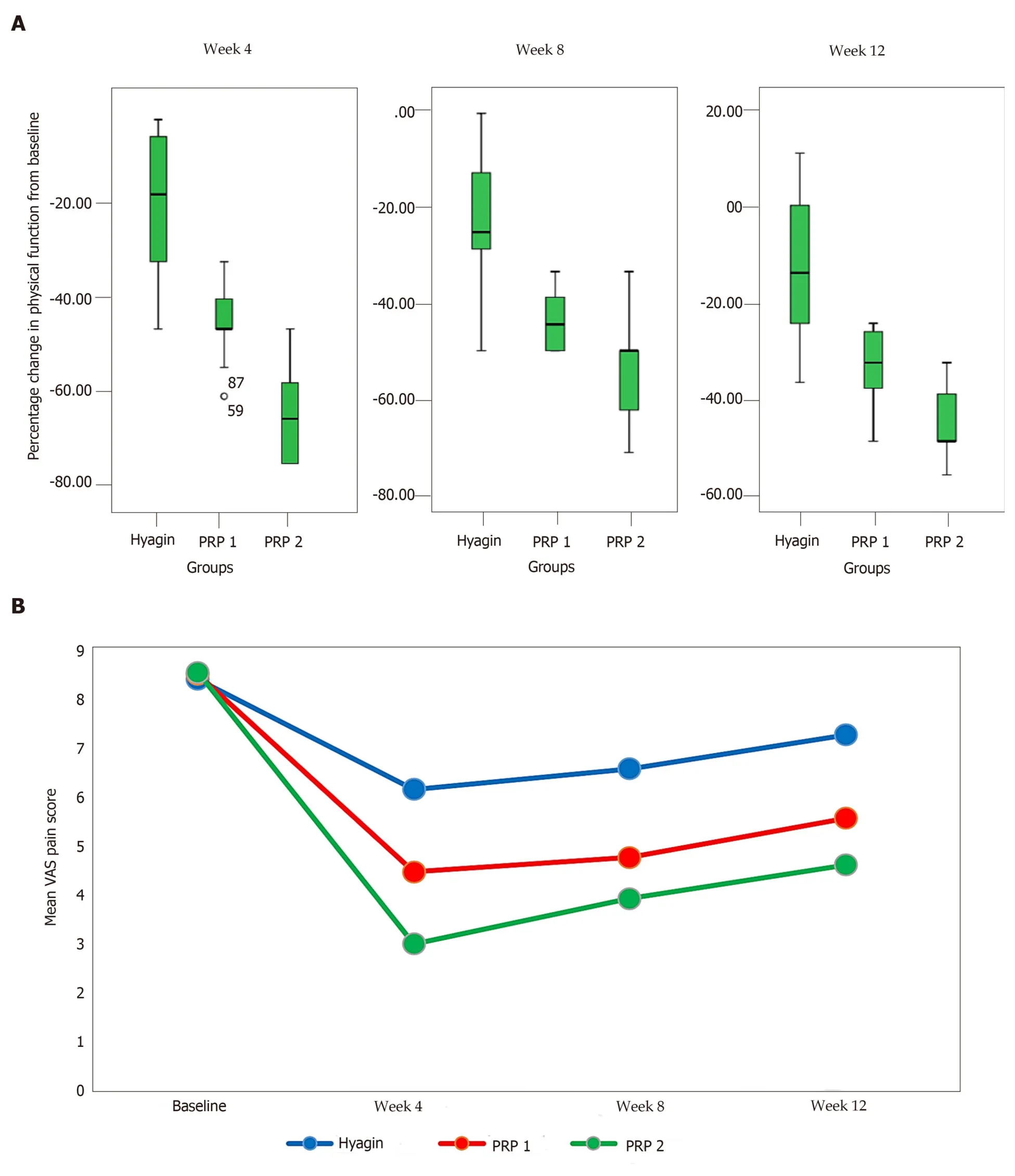
Figure 6 Comparison of the Visual Analogue Scale pain scores between the three intervention groups at baseline and subsequent follow-ups.
ARTICLE HIGHLIGHTS
Research background
Knee osteoarthritis is the most common articular disease that manifests as functional pain and joint stiffness, leading to disability in the elderly.More than 10% of the people aged ≥ 60 years suffer from this disease.
Research motivation
Hyaluronic acid is a therapeutic option for knee osteoarthritis.However, it has short-term effects on control of symptoms.Platelet-rich plasma (PRP) is also suggested for treatment of knee osteoarthritis.However, evidence about the clinical use of PRP is still insufficient.Investigations comparing the efficacy of these two drugs together are also insufficient.
Research objectives
The objective of this study was to compare the therapeutic efficacy of intra-articular injection of two different doses of PRPversushyaluronic acid in three groups of patients with knee osteoarthritis.
Research methods
This single-blinded randomized controlled trial study involved 95 patients with bilateral knee osteoarthritis.Thirty-one subjects received a single injection of PRP (group PRP-1), 33 subjects received two injections of PRP at an interval of 3 wk (group PRP-2) and 31 subjects received three injections of hyaluronic acid at 1-wk intervals (group hyaluronic acid).The patients were investigated prospectively at the enrollment and at 4-, 8- and 12-wk follow-up with the Western Ontario and McMaster Universities Arthritis Index and Visual Analogue Scale questionnaires.
Research results
In the groups PRP-1, PRP-2 and hyaluronic acid, 86%, 100% and 0% of the patients, respectively experienced at least a 30% decrease in the total score for the Western Ontario and McMaster Universities Arthritis Index pain subscale from baseline to wk 12 of the intervention (P< 0.001).The mean total Western Ontario and McMaster Universities Arthritis Index scores for groups PRP-1, PRP-2 and hyaluronic acid at baseline were 63.71, 61.57 and 63.11, respectively, which were significantly improved at final follow-up to 42.5, 35.32 and 57.26, respectively.The highest efficacy of PRP was observed in both groups at wk 4 with about a 50% decrease in the symptoms compared with about a 25% decrease for the hyaluronic acid group.Group PRP-2 had higher efficacy than group PRP-1.No major adverse effects were found during the study.
Research conclusions
PRP is a safe and efficient therapeutic option for treatment of knee osteoarthritis (significantly better than hyaluronic acid).The efficacy of PRP increases after multiple injections.
Research perspectives
Future studies with longer follow-up are suggested to evaluate long-term efficacy and potential compactions.We also propose that future studies use magnetic resonance imaging to assess and quantify cartilage regeneration if costs and ethical issues allow.
ACKNOWLEDGEMENTS
The authors would like to thank Mr.Mohammad Zamani, a member of Student Research Committee of Babol University of Medical Sciences, for his help in statistical analyses and data interpretation.We are also thankful to the Vice Chancellor for Research and Technology of Babol University of Medical Sciences for supporting our study.
