Low-velocity simultaneous bilateral femoral neck fracture following long-term antiepileptic therapy: A case report
2019-10-21MohammedSadiqVikrantKulkarniSyedAzherHussainMohammedIsmailMayurNayak
Mohammed Sadiq, Vikrant Kulkarni, Syed Azher Hussain, Mohammed Ismail, Mayur Nayak
Mohammed Sadiq, Vikrant Kulkarni, Syed Azher Hussain, Mohammed Ismail, Mayur Nayak,Department of Orthopaedics, ESIC Medical College, Gulbarga, Karnataka 585106, India
Abstract
Key words: Case report; Bilateral femoral neck fracture; Antiepileptic drug therapy; Druginduced osteopenia; Bisphosphonates; Vitamin D
INTRODUCTION
Simultaneous bilateral femoral neck fracture is a relatively rare fracture pattern[1-4].Most of these fractures are a result of low-velocity injury or atraumatic fracture over an underlying bone pathology[2]. Disorders of bone metabolism, like osteoporosis,osteomalacia, rickets, hyperparathyroidism and chronic renal failure, have all been reported with this fracture pattern[5-9]. Association with seizure disorders and electric shock injuries has also been reported[10-11]. Finally, this fracture pattern has been seen with long-term use of bisphosphonates, narcotic drug abuse, anti-retroviral therapy,and psychosomatic disorders, like anorexia nervosa[12-15].
Antiepileptic drugs (AEDs) are also a known cause of drug-induced osteoporosis.Enzyme-inducing AEDs cause a greater degree of osteoporosis than their noninducing counterparts. This is explained by the increased metabolism of vitamin D and direct inhibitory effect on the proliferation of osteoblasts. To the best of our knowledge, there is only one previous case report of an atraumatic bilateral femoral neck insufficiency fracture in a patient with long-term intake of carbamazepine[11]. We present here a similar case of simultaneous displaced bilateral neck of femur fractures in a known epileptic on long-term phenytoin therapy following a trivial fall in the home.
CASE PRESENTATION
Chief complaints
A 50-year-old male patient presented to the Orthopaedics outpatient department of our hospital with complains of persistent pain in both hips that had begun 10 d prior,following a fall from the bed.
History of present illness
The patient had sustained injury to both hips following a fall from the bed in his home, after which he was unable to stand up and walk. Considering the trivial cause of injury, he did not consult any doctors for 8 d and received massage therapy from a local orthotist to address the persistent pain. When the pain did not subside, he presented to our hospital on the 10thd after injury.
Past history
The patient was a known epileptic on oral phenytoin treatment for the past 3 years.The last seizure episode was 1 year previous, and the present injury was not associated with any seizure episode. The patient had no other co-morbidities and was not on any other medications.
Physical examination
On examination, the patient was alert, oriented and cooperative. Vital parameters recorded were normal. The patient’s weight was 59.2 kg (body mass index of 21.2 kg/m2). There was tenderness in both groins. Both the lower limbs were in external rotation and passive movements were associated with severe pain.
Laboratory testing
Below normal levels were found for serum calcium (4.2 mg/dL; normal: 8-10 mg/dL),phosphorous (2 mg/dL; normal: 2.5-4.5 mg/dL), and vitamin D (9 ng/mL; normal:20-50 ng/mL). Bone mineral density was assessed using dual-energy x-ray absorptiometry scan (OsteoPro Grand Mini; Aarna Systems, Rajasthan, India) which showed T score of -3. Results from the other blood investigations, including renal and liver function tests, were normal.
Imaging examination
A radiograph of pelvis for both hips showed completely displaced bilateral,transcervical femoral neck fractures (Figure1). The greater trochanter was upridden on both sides. Significant osteopenia was noted (Singh’s grade IV).
FINAL DIAGNOSIS
Based upon the patient’s history and findings from clinical examination and imaging studies, displaced bilateral neck of femur fractures was diagnosed. Based upon the findings from lab investigations and imaging studies, the patient was diagnosed with severe osteoporosis, with possibility of being attributable to the prolonged intake of AEDs.
TREATMENT
Considering the delay in the diagnosis of the patient’s fractures and underlying osteoporosis, a bilateral cemented modular hemiarthroplasty (Life Surgicals, Kerala,India) was performed. Intraoperatively, the bone was found to be weak, and in the process of trial reduction the patient suffered a fracture of the greater trochanter on the left side. The trochanter was fixed with stainless steel wire, and the patient was immobilized for 3 wk post-operatively.
OUTCOME AND FOLLOW UP
Partial weight bearing mobilization with walker was started after 3 wk and unassisted walking was allowed after 6 wk (Figure2). Calcium and vitamin D supplementation was started from the 1stpost-operative day. The patient was put on a weekly risedronate supplementation regimen for 6 mo post-operatively. The post-operative course was uneventful. The Harris hip score at the end of 1 year was 84 (good).
DISCUSSION
Simultaneous bilateral fracture of femoral neck is a relatively uncommon injury[1-4]. It has been seen in all age groups, from early childhood to the 9thdecade of life[5,17]. It has also been reported to result from low-velocity as well as high-velocity injuries, an example of the latter being road traffic accidents[4,5]. The former can also present as a bilateral stress fracture in army recruits[18,19].
The low-velocity fractures have been associated with various underlying bony pathologies; a summary of these publications is presented in Table1. Of all the systemic disorders related to these fractures in general, epilepsy is the most prevalent.For most of those cases, the fracture-inducing injury was related to seizure activity,mostly due to its manifestation of uncoordinated muscle contractions. AEDs are also an independent cause of drug-induced osteoporosis. Among the AEDs currently in use, the drugs which work as liver enzyme inducers have shown a higher negative effect on bone metabolism. The enzyme-inducing AEDs include carbamazepine,phenobarbitone, and phenytoin[23]. Research has uncovered several of the mechanisms by which AEDs affect bone metabolism; these include (1) decreasing growth velocityviasignificant reduction of procollagen; (2) modulating voltage-gated sodium channels and producing a negative effect on osteoblasts; (3) lowering of the levels of vitamin D, calcium and ionized calcium; and (4) decreasing bone mineral density around the femoral neck and lumbar spine.
There have been previous reports of this fracture pattern associated with epilepsy and AEDs[11,20-22]. But, most of these cases involved fractures that had occurred during a seizure episode. To the best of our knowledge, there is only one case of bilateral femoral neck stress fractures reported in the literature, and this involved a 26-year-old female who was on carbamazepine AED treatment for 12 years[11]. The patient presented with a 3-mo history of pain in the bilateral groins and was diagnosed with insufficiency fractures of the femoral necks. Considering that there was no history of trauma and the last seizure episode had occurred 6 mo prior, the authors correlated the femoral neck fractures to AED-induced osteoporosis.
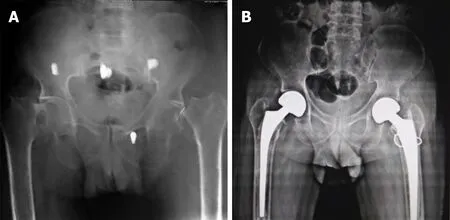
Figure1 Radiograph. A: Preoperative radiograph showing bilateral displaced fracture neck of femur with significant osteopenia. B: Postoperative radiograph at three months. There was a fracture of the greater trochanter on the left side which was fixed with stainless steel wire. There is a good union of the greater trochanter.
In our case described herein, the male patient was on oral phenytoin therapy for the past 3 years and the last seizure episode had been 18 mo ago. The fracture resulted from a trivial fall from the bed at home. The x-rays showed completely displaced fractures. Such displacement in bilateral femoral neck fractures in a physiological young patient is usually associated with high-velocity injury. Considering the low velocity of injury and the patient’s years-long history of enzyme-inducing AED treatment, we also correlated the fractures with primary AED-induced osteoporosis.As such, this is only the second case with such injury pattern resultant from AED-induced osteoporosis.
In most situations, these fractures can be picked up on plain radiographs. However,in the case of insufficiency fractures, MRI is considered the investigation of choice[11].Complete blood investigations to identify the underlying pathology is an indispensable component in the management of these fractures. Usually there is an associated negative calcium balance with decreased serum calcium and phosphorous levels. There may also be associated vitamin D deficiency.
The treatment plan depends upon age at presentation, and likely duration after injury, bone quality, and chances of achieving union with the underlying bone pathology. In our case, since the fracture fragments were completely displaced and because the patient presented 10 d after the injury, we performed a hemi-replacement surgery. For minimally displaced fractures or stress fractures presenting within 24 h,fixation of the fracture can be attempted. Irrespective of the treatment, it is essential to improve the calcium balance in the post-operative period. Supplemental calcium and vitamin D should be provided to all patients. Injectable parathyroid hormone(parathyroid hormone-related protein, ‘PTHrP’) supplementation can also be given to build up the bone stock. Bisphosphonates should be used cautiously, as there is an additional association between their long-term use and these fractures[12].
EXPERIENCES AND LESSONS
Epilepsy is a very common disease among the general population, and AEDs are indispensable in the treatment of these patients. The reporting of this case sheds light on osteoporosis in epileptics, as it is a common adverse effect of the long-term use of AEDs. Regular monitoring of serum calcium levels, vitamin D levels, and bone mineral density is important in the follow-up of patients on AEDs. Prophylactic supplementation of vitamin D, oral calcium, and bisphosphonates should be considered in patients on long-term AEDs. Creating awareness of this problem among patients and the physicians treating them can help to prevent such major fractures and improve the quality of life of patients on AEDs.
CONCLUSION

Figure2 Patient walking unsupported at three months after the surgery.
Simultaneous bilateral femoral neck fractures are most commonly a result of lowvelocity injury in an underlying weak bone. Enzyme-inducing AEDs produce significant osteoporosis and consequent susceptibility to fracture, even from trivial injury. The surgical management of these fractures represents only a part of the complete treatment protocol. The main goal of medical management should include correction of the drug-induced osteoporosis. Bisphosphonates and vitamin D supplementation should be used in the post-operative period for this purpose.Replacement surgery is a good treatment modality for displaced neck fractures with delayed presentation.
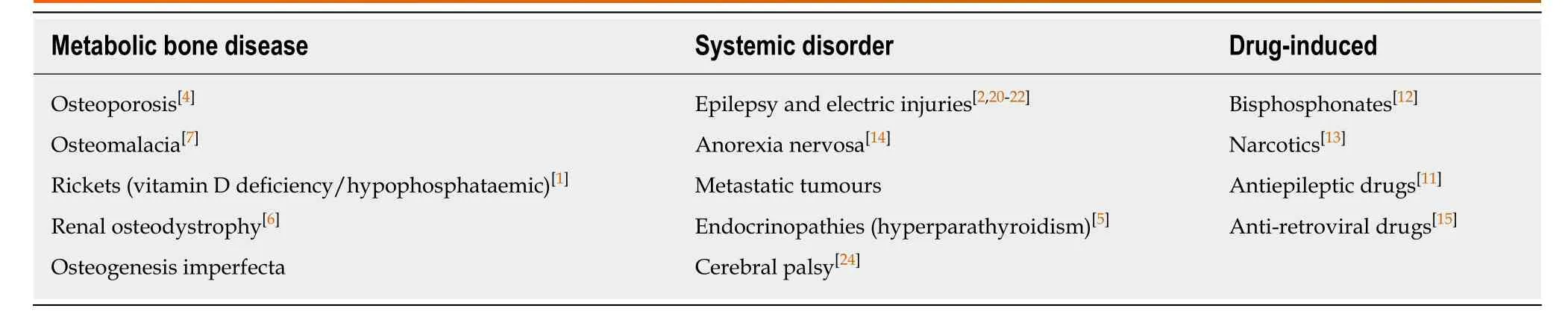
Table1 Factors associated with simultaneous bilateral femoral neck fractures
