动脉僵硬度和骨保护素对稳定型冠状动脉疾病患者的预后评估
2019-10-18延喜悦黄永华
延喜悦 黄永华
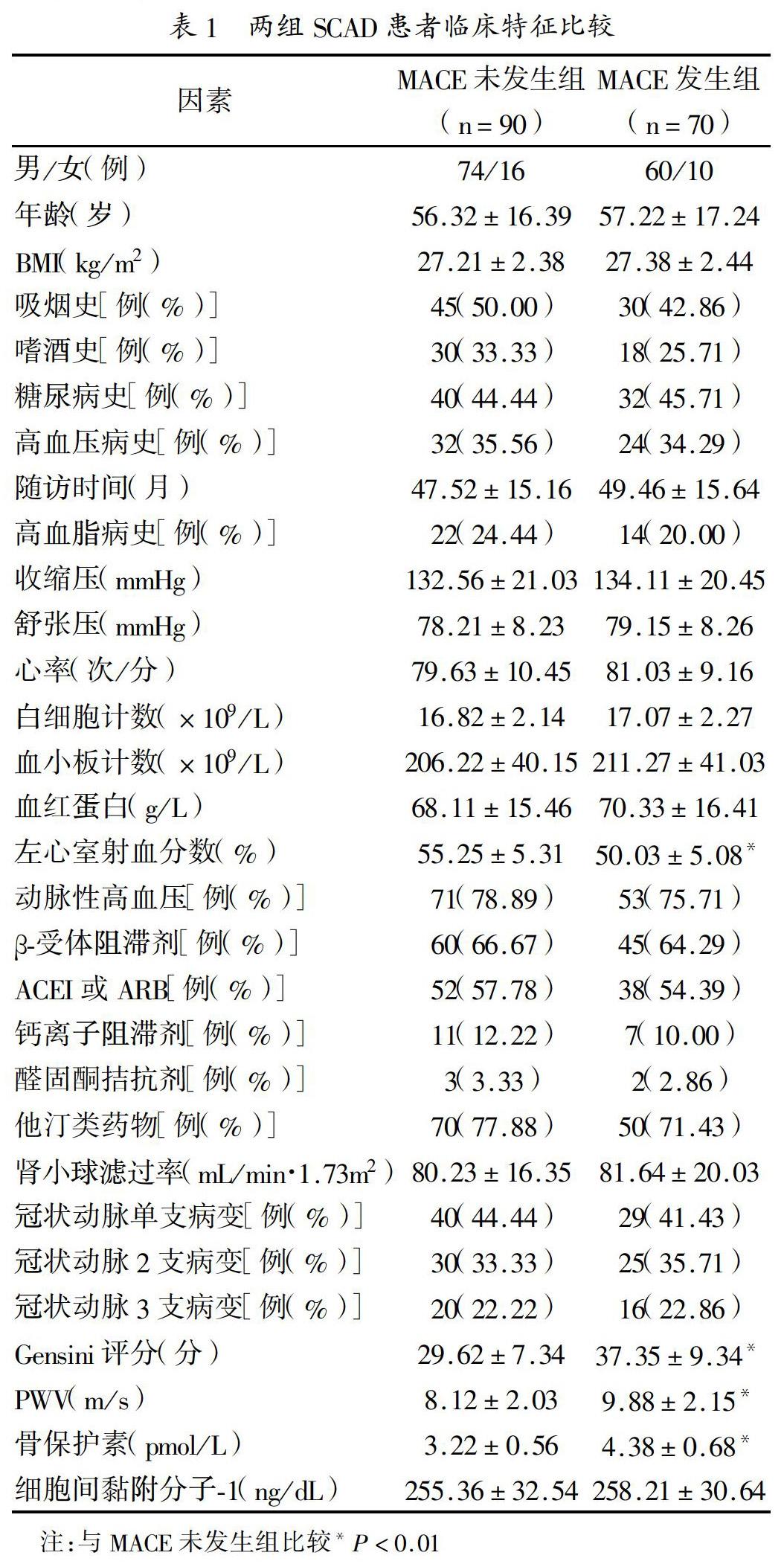
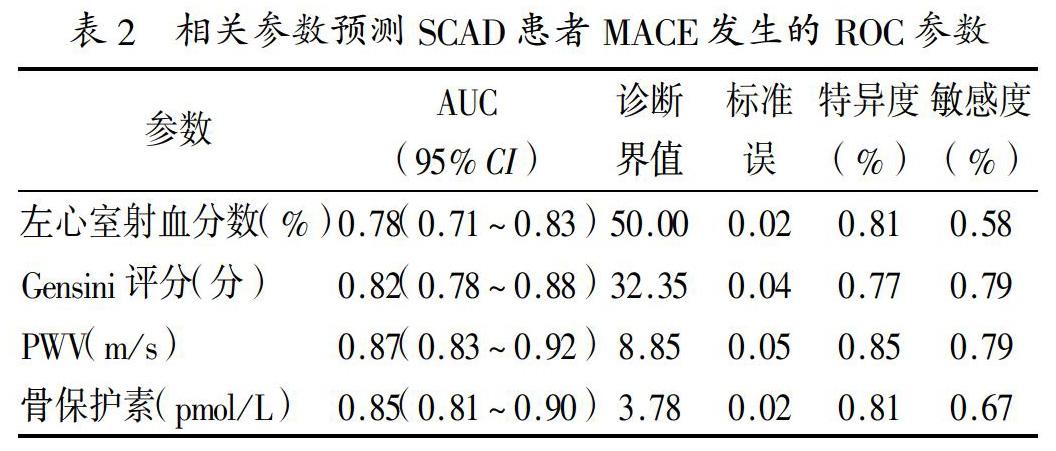
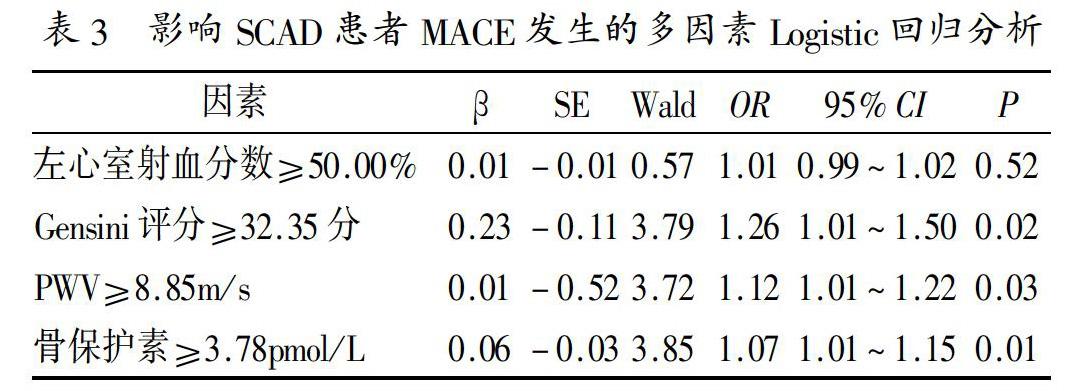
[摘 要] 目的 探討动脉僵硬度和骨保护素对稳定型冠状动脉疾病(stable coronary artery disease,SCAD)患者预后的预测价值。方法 回顾性选择在我院接受冠状动脉介入治疗的SCAD患者160例作为研究对象。根据随访期间有无主要不良心血管事件(major adverse cardiovascular events,MACE)发生分为MACE发生组(n=70)和MACE未发生组(n=90)。比较两组患者在临床特征方面的差异。通过绘制受试者工作特征曲线(receiver operating characteristic curve,ROC),筛选切点,计算曲线下面积评估不同参数预测SCAD患者MACE发生效力。应用多因素非条件Logistic回归分析影响SCAD患者MACE发生的危险性因素。结果 MACE未发生组左心室射血分数高于MACE发生组,Gensini评分、脉搏波速度(pulse wave velocity,PWV)、骨保护素水平低于MACE发生组,差异有统计学意义(均P<0.05)。左心室射血分数、Gensini评分、PWV、骨保护素预测SCAD患者MACE发生的诊断界值分别为50.00%、32.35分、8.85m/s、3.78pmol/L(均P<0.05)。多因素Logistic回归分析结果显示,Gensini评分≥32.35分、PWV≥8.85m/s、骨保护素≥3.78pmol/L增加SCAD患者MACE发生风险(OR=3.72~3.85,均P<0.05)。结论 Gensini评分、PWV、骨保护素水平与SCAD患者MACE发生密切相关。PWV和骨保护素水平偏高不利于SCAD患者预后。
[关键词] 动脉僵硬度;骨保护素;稳定型冠状动脉疾病;主要不良心血管事件
中图分类号:R541.4 文献标识码:A 文章编号:1009-816X(2019)04-0311-04
[Abstract] Objective To investigate the prognostic role of arterial stiffness and osteoprotegerin in patients with stable coronary artery disease (SCAD). Methods 160 patients with SCAD received coronary intervention therapy in our hospital were selected.The patients were divided into MACE group (n=70) and non-MACE group (n=90) according to whether MACE happened or not during the follow-up period. The differences in clinical characteristics between the two groups were compared. The ROC curve was drawn, the cut points were selected, the area under the curve was calculated, and the different parameters were used to predict the effectiveness of MACE in SCAD patients. Multivariate logistic regression analysis was used to analyze the risk factors of MACE in SCAD patients. Results The left ventricular ejection fraction in non-MACE group was higher than that in MACE group, while Gensini score, PWV, and osteoprotegerin were lower than those in MACE group, the difference were statistically significant (P<0.05). The diagnostic values of left ventricular ejection fraction, Gensini score, PWV and osteoprotegerin in predicting the occurrence of MACE in SCAD patients were 50.00%, 32.35points, 8.85m/s and 3.78pmol/L, respectively (P<0.05). The results of multiple factor logistic regression analysis showed that the Gensini score≥32.35 points, PWV≥8.85m/s, and osteoprotegerin≥3.78pmol/L increased the risk of MACE occur in SCAD patients (OR=3.72~3.85, P<0.05).Conclusions Gensini score, PWV and osteoprotegerin are closely related to MACE in SCAD patients. The high level of PWV and osteoprotegerin is bad for the prognosis of SCAD patients.
2.2 相关参数预测SCAD患者MACE发生的ROC参数的特异度和灵敏度:见表2。
2.3 SCAD患者MACE发生的多因素Logistic回归分析:以随访期间有无MACE发生为因变量(赋值:未发生=0,发生=1),以左心室射血分数、Gensini评分、PWV、骨保护素为自变量,构建Logistic回归模型。模型似然比检验,有统计学意义(均P<0.05)。多因素Logistic回归分析结果显示,Gensini评分≥32.35分、PWV≥8.85m/s、骨保护素≥3.78pmol/L会增加SCAD患者MACE发生风险(OR=3.72~3.85,均P<0.05),见表3。
3 讨论
根据欧洲心脏病学会《稳定性冠心病诊治指南》标准,急性冠状动脉综合征(ACS)稳定后无症状或症状稳定、稳定型心绞痛、痉挛导致的静息发作心绞痛均属于SCAD[9]。既往研究证实,SCAD的发病机制包括微血管功能障碍、心外膜冠状动脉狭窄、局灶性或弥漫性痉挛、既往急性缺血、冠状动脉粥样硬化、左心室功能不全等[11]。因此,寻找能预测SCAD患者MACE发生的危险性因素,对于提高患者生活质量至关重要。目前,SCAD患者常规的血清学、冠状动脉造影、心电图检测多为阴性,且缺乏相关预测SCAD患者MACE发生的特异性分子标志物及指标。
本研究160例SCAD患者中,MACE发生率为43.75%(70/160),高于既往研究结果。这或许是由于入组的患者临床病理资料差异导致。本研究发现,MACE未发生组与发生组在左心室射血分数、Gensini评分、PWV、骨保护素方面差异有统计学意义。上述指标或许与SCAD患者MACE发生密切相关。进一步多因素Logistic回归分析发现,Gensini评分≥32.35分、PWV≥8.85m/s、骨保护素≥3.78pmol/L会增加SCAD患者MACE发生风险。研究结果表明Gensini评分、PWV及骨保护素参与了SCAD患者冠状动脉介入治疗后MACE发生过程。Gensini评分可反映每支冠状动脉血管病变的狭窄程度,并能客观评估冠状动脉病变的进展情况[12]。本研究证实了Gensini评分是SCAD患者MACE发生的危险性因素。先前研究已经证实,骨保护素在骨代谢、恶性肿瘤、冠心病、糖尿病等疾病方面发挥重要作用[13,14]。骨保护素影响SCAD患者MACE发生的机制或许为:(1)骨保护素可通过抑制细胞毒性配体-肿瘤坏死因子相关凋亡诱导配体介导的血管细胞的凋亡影响SCAD患者血管系统;(2)SCAD患者MACE发生组中骨保护素水平升高,可能是对动脉粥样硬化进程的一种自我防御性代偿反应。PWV是一种反映SCAD患者动脉僵硬度的非侵入性手段,是评价血管结构及功能的重要指标。PWV升高预示动脉弹性减退,造成动脉所受的牵拉力增加、血管壁压力增大,可导致血管壁弹性成分断裂,进一步造成血管内膜损伤及动脉粥样硬化,当动脉粥样硬化发展到一定程度便可导致MACE发生[13]。本研究与Siasos等[15]研究结果一致,均明确骨保护素和PWV在预测SCAD患者预后中具有重要价值。相关机制研究还需后期进一步探讨。
本研究为回顾性研究,容易造成选择偏倚;且为单中心研究,样本量少,制约研究结论准确性;加之,患者发病及入院时间不一致,可能对PWV、骨保护素等临床指标的测定产生影响。但本文显示Gensini评分、PWV、骨保护素与SCAD患者MACE发生密切相关,PWV和骨保护素水平偏高不利于SCAD患者预后,应引起临床医师密切关注。
参考文献
[1]沈迎,张奇,沈卫峰.美国和欧洲稳定性冠心病诊治指南解读[J].中华心血管病杂志,2014,42(1):70-72.
[2]王朝晖.冠状动脉斑块与微血管病變—2013 ESC-SCAD指南的启示[J].临床心血管病杂志,2014,30(7):557-559.
[3]Adams H, Paratz E, Somaratne J, et al. Different patients, different outcomes: A case-control study of spontaneous coronary artery dissection versus acute coronary syndrome[J]. J Interv Cardiol,2018,31(1):41-47.
[4]Lin MJ, Chen CY, Lin HD, et al. Impact of diabetes and hypertension on cardiovascular outcomes in patients with coronary artery disease receiving percutaneous coronary intervention[J]. BMC Cardiovasc Disord,2017,17(1):12-21.
[5]Rusnak J, Fastner C, Behnes M, et al. Biomarkers in stable coronary artery disease[J]. Curr Pharm Biotechnol,2017,18(6):456-471.
[6]Mccarthy CP, Mcevoy JW, Januzzi JL. Biomarkers in stable coronary artery disease[J]. Am Heart J,2018,196(1):82-96.
[7]耿学峰,宋丽萍,朱宏旭,等.BaPWV联合超声心动图检测在冠心病心功能异常和心脏重构研究中的意义[J].中国医药导刊,2016,18(7):653-654.
[8]Nugroho J, Widorini W. Correlation between osteoprotegerin serum level and coronary calcification using coronary artery calcium score in patient with moderate-severe cardiovascular risk factor[J]. Int J Angiol,2017,26(4):234-237.
[9]Members TF, Montalescot G, Sechtem U, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the task force on the management of stable coronary artery disease of the european society of cardiology[J]. Eur Heart J,2013,34(38):2949-3003.
[10]金晶,秦慧娟.益氣活血化痰方联合小剂量阿托伐他汀对高危性COPD患者动脉僵硬度、血液黏度及预后的影响研究[J].重庆医学,2017,46(28):3943-3946.
[11]Rah S, Colquhoun DM, Marschner SL, et al. Persistent psychological distress and mortality in patients with stable coronary artery disease[J]. Heart,2017,103(23):1860-1866.
[12]Ueland T, Akerblom A, Ghukasyan T, et al. Osteoprotegerin is associated with major bleeding but not with cardiovascular outcomes in patients with acute coronary syndromes: insights from the PLATO (platelet inhibition and patient outcomes) trial[J]. J Am Heart Assoc,2018,7(2):e007009.
[13]Grzelka A, Naskret D, Araszkiewicz A, et al. Higher concentrations of osteoprotegerin in type 1 diabetic patients are related to retinopathy: results from the poznań prospective study[J]. Adv Clin Exp Med,2017,26(9):1343-1349.
[14]Ikonomidis I, Makavos G, Lekakis J. Arterial stiffness and coronary artery disease[J]. Curr Opin Cardiol,2015,30(4):422-431.
[15]Siasos G, Oikonomou E, Maniatis K, et al. Prognostic significance of arterial stiffness and osteoprotegerin in patients with stable coronary artery disease[J]. Eur J Clin Invest,2018,48(3):e12890.
