Role of trace mineral in periodontal health: a review
2019-10-14AdiyaAponPraneetaKamble
Adiya Apon, Praneeta Kamble
Department of Periodontics, Nair Hospital Dental College, Mumbai, India
Abstract
Key words: nutrition; periodontitis; micronutrients; iron; zinc; selenium; copper; diabetes mellitus; anaemia; antioxidant; reference value
INTRODUCTION
Periodontitis is defined as “an inflammatory disease of the supporting tissues of the teeth caused by specific microorganisms or groups of specific microorganisms, resulting in progressive destruction of the periodontal ligament and alveolar bone with pocket formation, recession or both.”1Regarding the onset/progression of periodontal breakdown, a number of risk indicators/factors have been identified.These are characterised by genetic, environmental (e.g., stress, bacterial challenge) and lifestyle/behavioral (e.g., exercise, nutrition, smoking).2Risk factors are important in the development and propagation of periodontal disease and act predominantlyviamodification of the host response to bacterial challenge, resulting in less effective clearing of pathogenic species and inflammation resolution, which in turn increases host mediated tissue damage.The onset and progression of disease depend upon a delicate equilibrium between the microbial challenge and the host response.3
Nutrition has significant effects on the inflammatory processes as well on the cellular and humoralimmune mechanism.The interaction between nutritional status and the immune response to the bacterial challenge can be an underlying factor in the progression of periodontal disease.4Nutrients can be divided into six major classes,i.e., fats, carbohydrates, proteins, minerals, vitamins and water; these can be further subdivided into two broad categories, ‘macronutrients’ (fats, carbohydrates and proteins), which are required in large quantities from the diet providing a vital energy source and ‘micronutrients’(minerals, vitamins, trace elements, and amino-acids), which are essential co-factors required for functioning of many enzyme systems, such as DNA polymerase, RNA polymerase,superoxide dismutase, catalases, and alkaline phosphatase.4,5
Micronutrients are dietary compounds that do not provide energy but are required by living organisms and are essential for optimal health, proper growth, and metabolism.4,5
Micronutrients are required in milligram (mg) to microgram (μg) quantity and include vitamins and minerals.The major minerals are sodium (Na), potassium (K), calcium(Ca), magnesium (Mg), phosphorus (P) and sulfur (S).The trace minerals are: iron (Fe), zinc (Zn), iodine (I), selenium(Se), fluoride (F), copper (Cu), cobalt (Co), chromium (Cr),manganese (Mn) and molybdenum (Mo).Recommended daily allowance of micronutrient such as iron, copper, and zinc is less than 100 μg.4Depletion or lack of availability of these nutrients gives rise to malnutrition at either the macro or micronutrient level.Both are detrimental to periodontal health as well as to general health.
Micronutrient deficiencies can be provoked by6:
· Drugs (e.g., antacids, antibiotics, antihypertensives, chelating agents, corticosteroids, diuretics, laxatives, lipidlowering drugs, non-steroidal anti-inflammatory drugs, and cancer chemotherapeutics);
· Malabsorption or diarrhea;
· Lifestyle factors (e.g., diet, malnutrition, chronic alcohol or nicotine abuse, and consumption of fast foods or processed foods);
· Systemic disorders (e.g., diabetes mellitus, thyroid and parathyroid disorders, liver and kidney diseases, psoriasis,and atopic dermatitis);
· An increased requirement (e.g., during pregnancy, breastfeeding, growth, physical/mental stress, convalescence,exposure to heavy metals, and heavy sweating);
· Loss (e.g., following hemodialysis, nephrosis, surgery, or burns).
Micronutrients play a role in both health and disease.The vitality of the periodontal tissues in both health and disease depends on the adequate source of essential nutrients being available to the host.
This review aims to discuss the role of some important trace mineral micronutrients essential for periodontal health.
SEARCH STRATEGY AND SELECTION CRITERIA
The PubMed database was searched.Common keywords relating to periodontitis and micronutrients were derived from the literature.We restricted our search studies in English, relating to humans, published after January 1, 1980.Searches were run from January 1, 1980 to March 1, 2019.The full electronic searches are shown in Table 1.
ESSENTIAL TRACE MINERAL MICRONUTRIENTS FOR PERIODONTAL HEALTH
Iron
Fe is the most abundant essential trace element in the human body.The total content of Fe in the body is 3-5 g with most of it in the blood.About 4 g of Fe is present in the typical person:2.5 g in hemoglobin; 0.3 g in myoglobin and cytochromes;and about 1 g in Fe stores (ferritin).7The Recommended Daily Allowance for Fe varies with age.Its requirement is highest in women of reproductive age group which is 18 mg/d, while in middle-aged adults, it is about 8 mg/d.8Typical intake of Fe is about 10 mg/d, but only about 10% is absorbed.Fe is absorbed in the gut from diet in case of depletion and transported in the form of ferritin.Its reduced absorption results in Fe deficiency anaemia where the hemoglobin levels are< 12 g/dL for adult non-pregnant women and < 13 g/dL for adult men.9Furthermore, in Fe deficiency anemia, decreased serum Fe and ferritin levels and increased total Fe binding capacity are seen.This should be distinguished from anemia of chronic disease which is a cytokine-mediated anemia more prevalent in individuals with chronic inflammatory, infectious,or neoplastic disorders and characterized by hypoferremia with adequate reticuloendothelial Fe stores.10,11
Optimal levels of Fe are essential prerequisite for periodontal health and shift in either direction may be detrimental.The role of Fe in periodontal ligament and alveolar bone homeostasis and function was recently verified in an animal model.12The PDL cells have the ability to regulate Fe uptake by expressing the light and heavy chain subunits of heteromeric ferritin.12,13This further controls the cyto-differentiation of these cells into osteoblasts and mineralization, thereby affecting the bone density.12,13Fe is essential for both innate and adaptive immune responses.14Its deficiency weakens the cell-mediated immunity by reducing lymphocyte count, interferon-γ and interleukin-2 levels and functions of natural killer cells.The delayed type of hypersensitivity response mediated through CD4+lymphocytes is also disrupted.15,16It also results in reduced immunoglobulin E (IgE) production, high CD4+to CD8+T cell ratios, low numbers of CD28+cells and impaired CD8+T-cell function.17Furthermore, Fe plays an important role in oxidative burst,i.e., the release of reactive oxygen species (ROS) from macrophages and neutrophils.A shift in the levels of Fe may cause oxidative stress leading to periodontal destruction.This is mainly related to the conversion of hydrogen peroxide to ROS through Fenton reactions catalysed by free Fe.Subsequently,there is activation of matrix metalloproteinases, which degrade the extracellular matrix components.This further activates the nuclear factor-kappa B pathway stimulating the release of proinflammatory cytokines such as interleukin-1β, interleukin-6,interleukin-8 and tumor necrosis factor-α, which destroy the periodontal tissues and alveolar bone.
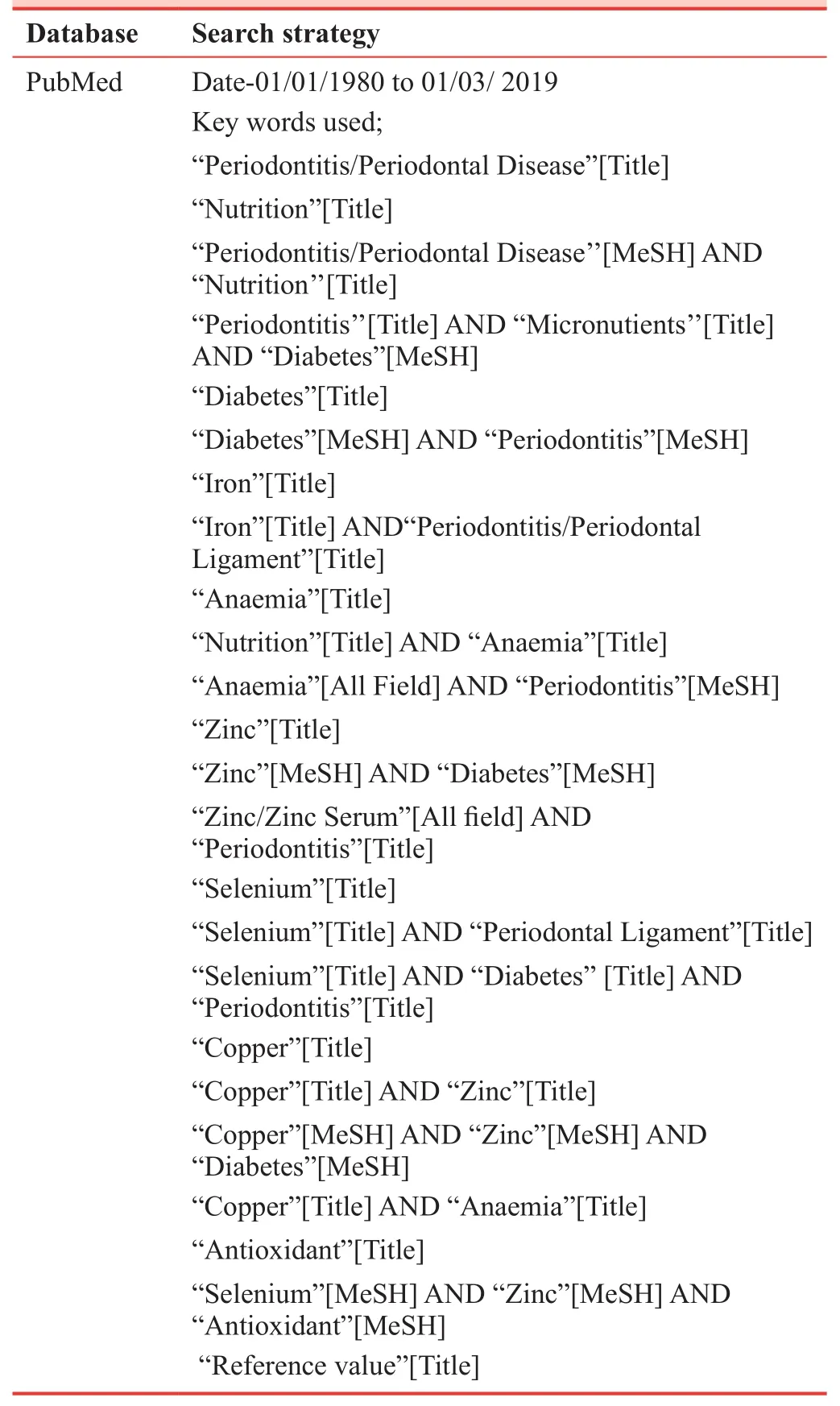
Table 1: Search strategy and selection criteria
Fe is required for the activation of enzymes such as inducible nitric oxide synthase, myeloperoxidase and NADPH oxidoreductase during bacterial phagocytosis.14,18,19Its deficiency may inhibit the activity of protective enzymes like myeloperoxidase, which are essential for the bactericidal activity of macrophages.20Additionally, it may reduce the levels of oxygen in the gingival tissues which further activates the inflammatory cascade.
Although the evidence for Fe deficiency directly causing chronic periodontitis is weak, the reverse association is com-paratively strong.20-23It has been suggested that inflammation due to chronic periodontitis results in increased levels of pro-inflammatory cytokines which suppresses erythropoiesis in bone marrow.23-25Patients with chronic periodontitis have a lower number of erythrocytes and a lower hemoglobin level than healthy controls.25A prospective study on a rural Japanese population26confirmed that, after adjusting for age,the progression of periodontal disease is associated with a decrease in erythrocyte counts.It was proposed that chronic periodontitis can lead to anemia of chronic disease, which may be explained by a depressed erythropoiesis resulting from the systemic effect of the pro-inflammatory cytokines in response to periodontal pathogens and their products.21,23,27In addition,improvement in hematological parameters up to 6 months following nonsurgical periodontal therapy of patients with chronic periodontitis was reported.21,23,27
Chakraborty et al.20reported that chronic periodontitis as well as Fe deficiency anemia in patients with and without periodontitis are associated with decreased salivary and serum superoxide dismutase levels compared to healthy controls.There was a significant, negative correlation between serum superoxide dismutase levels and all periodontal parameters.Patients with Fe deficiency anemia and comorbid chronic periodontitis exhibited a higher incidence of bleeding on probing,a higher percentage of sites with clinical attachment loss of ≥6 mm, as well as deeper periodontal pocket depths, compared with patients with chronic periodontitis only in this study.
It is documented that Fe affects glucose metabolism and it has been shown that free Fe concentrations in the patients with type 2 diabetes mellitus are higher than those of normal subjects, which could contribute to tissue damage that may potentially elevate the risk of type 2 diabetes mellitus.28,29
Thus, Fe is essential for immunological homeostasis.The general consensus is that both elevated and reduced levels are detrimental to the host immune responses, as well as susceptibility to infections.So, it is necessary to control its levels and needs tight regulation in order to guarantee the protective responses to the health.
Zinc
Zn is an essential trace element which is involved in a multitude of intracellular processes of more than 300 different enzymes, acting as an essential requirement for the successful growth of many internal organs, stabilizing cell membranes,and modulating membrane-bound enzymes and insulin action.29,30It plays an important role in immune function, wound healing, protein synthesis, DNA synthesis, and cell division.In addition, zinc is essential for intracellular binding of tyrosine kinase to the T-cell receptors, CD4 and CD8α, which are required for T-lymphocyte development and activation.In biological systems, zinc exists as Zn2+and is present in all tissues and fluids of the body.There is 2-4 g of Zn distributed throughout the human body.31Zn is stored in prostate, parts of the eye, brain, muscle, bones, kidney, and liver.The recommended dietary allowance of zinc is 8 mg for adult women and 11 mg for adult men.32
Zn is stored in liver cells by binding to the cytosolic proteins and accumulates in mitochondria and markedly increases succinate dehydrogenase activity in the organelle.Zn taken up by the liver binds to the subcellular organelles and affects the cellular metabolic system.This micronutrient participates both in the synthesis and actions of the hormones, which are intimately linked to bone metabolism.33In blood plasma, Zn is bounded and transported by albumin (60%) and transferrin(10%).34Since transferrin also transports Fe, excessive Fe can reduce zinc absorption, andvice versa.35
Zn is an integral component of antioxidant enzymes and its altered levels cause oxidative stress.Zn deficiency may cause oxidative damage to membranes, structural strains,altered function of specific receptors and nutrient absorption sites, altered activity of membrane-bound enzymes, altered function of permeability channels, altered function of carrier and transport proteins in the membrane.36Zn deficiency also affects the functioning of immune cells such as monocytes (all cells), natural killer cells (reduced cytotoxicity), neutrophils(reduced phagocytosis), T cells and lymphocytes (decreased apoptosis).Furthermore, it increases the secretion of proinflammatory cytokines.37
Optimal levels of Zn are imperative for growth and development of periodontal tissues.While the deficiency leads to reduced protection of sulpha-hydryl groups and increased production of ROS, excessive levels may act as pro-oxidant by eliciting decline in erythrocyte Cu-Zn superoxide dismutase.37This enzyme has been localized in the human periodontal ligament where it prevents free radical induced damage.38,39Therefore, its optimum levels are a prerequisite to maintain the tissues in a healthy state.Animal studies have revealed that dietary deficiency of Zn leads to poorer periodontal health.It alters the thickness and keratinization of oral mucosa which becomes more susceptible to infections.Furthermore,deeper periodontal pockets and thicker palatal tissues have been reported in Zn deficient rats.40,41Zn deficiency has also been shown to reduce osteoblastic activity, collagen and proteoglycan synthesis as well as alkaline phosphatase activity.Serum zinc levels and the severity of periodontal disease were evaluated in patients undergoing periodontal treatment, or in untreated patients, in Sweden by Frithiof et al.42Patients with decreased Zn levels showed increased alveolar bone resorption.This could be related to altered bone collagen metabolism with a significant reduction in collagen synthesis and turnover as well as reduced alkaline phosphatase activity.
Thomas et al.43compared serum Zn levels in a group of patients with diabetes and periodontitis, with those in a group of patients with periodontitis but without diabetes,and with group of systemically and periodontally healthy control subjects, all from South-West India.The Zn levels were significantly lower in periodontitis patients, with and without diabetes, than in healthy individuals.Zn absorption decreases in diabetic patients, which causes intercellular depletion.Hyperglycemia causes the increased urinary losses of Zn and decreased Zn levels in the body.The decreased levels of Zn affect adversely the ability of the islet cell to produce and secrete insulin.44This altered metabolism of Zn leads to some diabetic complications.45
Thus, adequate levels of Zn are imperative for both protective immune and bone regenerative processes, which would further prevent the progression of periodontitis.
Selenium
Se is a mineral antioxidant essential for the proper functioning of various organ systems.Its biological functions are mainly exerted through selenoproteins, which are a group of antioxidants involved in activation, proliferation and differentiation of cells of innate and adaptive immunity.46They prevent exacerbation of immune responses in chronic inflammation.Various selenoproteins are glutathione peroxidase, thioredoxin reductases, deiodinases and selenoproteins P, K and S.46Among them, the glutathione peroxidase system is most widely investigated.Se is present in the glutathione peroxidase system and helps to minimize oxidative damage to lipid membranes.The recommended daily allowance for Se is 55 μg for adult men and adult women.47
The glutathione peroxidase enzymes utilize Se at their active sites to detoxify ROS including hydrogen peroxide and phospholipid hydroperoxide.The redox balance at the cellular level regulates the selenoproteins, which indirectly modulate immune cell signalling and function.46Likewise, Se regulates the activity of transcription factors (i.e., nuclear factor-κB and activator protein-1) and associated gene expression.It even reduces the levels of tumor necrosis factor-α and cyclooxygenase-2 produced by macrophages in response to lipopolysaccharides and downregulates the expression of adhesion molecules (i.e., intercellular adhesion molecule-1 and vascular cell adhesion molecule-1).Besides, it helps in metabolism of arachidonic acid and eicosanoids.It reduces monocyte adhesion and migration through endothelial cells.This is mainly related to Se induced shedding of L-selectin.At cellular level,dietary Se influences the leukocytic functions such as adherence, migration, phagocytosis and cytokine secretion.46
The deficiency of Se may be related to poor dietary intake,presence of chronic diseases and ingestion of drugs that reduce its absorption and proper utilization.Some studies even suggest that alcohol intake may result in poor concentrations of Se.48
The beneficial effects of Se on periodontium are mainly due to its antioxidant effects.In vitroand animal studies showed that addition of Se to α-tocopherol accelerated the proliferation rate and wound healing process.This was related to the increased synthesis of basic fibroblastic growth factor and type I collagen from both gingival and periodontal ligament fibroblasts in the presence of Se.49,50Thomas et al.51evaluated the concentrations of glutathione, catalase, and Se in the serum of middle-aged patients with type 2 diabetes mellitus and healthy individuals, with and without periodontal disease.The levels of glutathione, catalase, and Se were found to be significantly lower in patients with diabetes and periodontitis compared with healthy controls.Se levels in healthy individuals with periodontitis were also decreased; however, this did not reach significance.A co-morbid impact of periodontitis with diabetes upon systemic micronutrient status was seen,probably because of oxidative stress.52
Thus, Se is a protective trace mineral micronutrient for the periodontium and its inclusion in the diet may be vital in “dietary regulation of inflammatory cascade.”53Se in the diet would further prevent the progression of destructive periodontal disease.
Copper
Cu is the third most abundant trace element with only 75-100 mg of total amount in the human body.54Cu is present in almost every tissue of the body and is stored chiefly in the liver along with the brain, heart, kidney, and muscles.55Cu is essential for immunity and combating the oxidative stress induced by reactive oxygen and nitrogen species.It acts as a co-enzyme for cytochrome-C and superoxide dismutase and is involved in electron transport of proteins.It is also required in association with Fe for the formation of hemoglobin and is stored bound to ceruloplasmin, a Cu dependent ferroxidase.Ceruloplasmin helps in oxidising Fe so that ferritin is utilized.Therefore, its deficiency may cause anemia.56The Recommended daily allowance for Cu is 900 μg.57
Cu plays an important role in cytochrome oxidase functions at the terminal end of the mitochondrial electron transport chain.The loss of this activity can contribute to the characteristic swelling and distortion of mitochondria, which can be observed in Cu deficiency, particularly in metabolically active pancreatic acinar cells, enterocytes, and hepatocytes.58Abnormal metabolism of Cu can affect the function of superoxide dismutase and results in decreased protection of cells from superoxide radical.59Hyperglycemia and hyperinsulinemia increase the production of free radicals and decrease the efficiency of antioxidant defense systems, which may lead to the complications of diabetes.60
Cu deficiency also has a negative influence on neutrophils,macrophages, Tcells and natural killer cells.There is impaired production of interleukin-2 and excessive production of proinflammatory cytokines, such as tumor necrosis factor-α,matrix metalloproteinase-2 and -9 which degrade the collagen and extracellular matrix components in periodontal ligament.43Thomas et al.51conducted a study in which elevation of serum Cu level is observed in periodontitis patients causing certain alterations in collagen metabolism.Cu is essential for proper connective tissue development and the elevation in serum Cu may reflect the changes in periodontal collagen metabolism.Sundaram et al.61demonstrated the levels of Cu in diabetes and non-diabetes patients with chronic periodontitis; Cu were elevated at baseline and were improved significantly 3 months following nonsurgical periodontal therapy, even in those participants with uncontrolled type 2 diabetes mellitus.A study by Manea and Nechifor62has shown that there exists a connection between salivary copper levels and periodontitis.
As Cu serves as a cofactor for metalloenzyme like superoxide dismutase, an essential antioxidant for chronic periodontitis, optimal levels of Cu are essential for preventing exacerbation of inflammatory pathways.43
RECOMMENDATIONS OF MICRONUTRITIONAL THERAPY FOR A HEALTHY PERIODONTIUM
Nutrition is the mainstay of good health and immune system,and micronutrient administration to overcome their deficiencies is justified.There are two options to achieve this objective:Firstly, dietary modification; and secondly, administration of supplements.It has been suggested that where dietary manipu-lation is difficult, fortified foods and supplements may be a more practical choice.However, the argument regarding the cost-benefit effects and use of multi-micronutrient additives still prevails.63Even though numerous studies have evaluated the relationship between micronutrients and periodontal disease, intervention studies utilizing trace minerals in humans are scarce.20,43,51A randomized, parallel clinical trial evaluated the influence of multivitamin tablets as an adjunct to periodontal therapy over a 60-day period and significant improvement in probing depths of subjects with chronic periodontitis was seen in subjects who received the experimental treatment.64
The trace mineral micronutrients, Zn, Fe, Se and Cu, have been deeply investigated for their role in immune function and resistance to infection.Evidence from preclinical and clinical trials suggests that although Fe is essential for immune function, its supplementation does not necessarily decrease morbidity and mortality.53This could be related to the complexity of mechanisms of Fe homeostasis.Alternatively, strong evidence exists for the use of Se and Zn as dietary modulators due to their antioxidant and anti-inflammatory actions.65They prevent periodontal destruction by reducing the levels of plasma oxidative stress markers and pro-inflammatory cytokines.Furthermore, their administration in conjunction with periodontal therapy accelerated wound healing and improved the clinical periodontal parameters.A study investigated the effect of antioxidant therapy on the progression of periodontal disease when used as a monotherapy and/or as an adjunct to non-surgical debridement.66About 6 mg of antioxidants was administered in three divided doses for 2 weeks in the form of soft gel containing lycopene 2000 μg, Zn 7.5 mg and Se 35 μg.The results showed significant improvement in the salivary antioxidant levels and its response to periodontal therapy.66
Even though some reliable evidence exists, caution should be practised when advising supplements, as risk for toxicity cannot be ruled out.Following guidelines may be helpful in determining the micronutrient requirements for oral and general health.67
(1) Dietary assessment of nutritional intake should be done by a dietician.This involves use of a questionnaire to explore the dietary intake over a period of time;
(2) Clinical assessment of nutritional status through changes in skin, nails, eyes, hair, mouth, neck, abdomen and extremities should be done;
(3) Screening tools like, the Malnutrition Universal Screening Tool, a five-step screening method, may be utilized to identify individuals who are malnourished or at risk of malnutrition.This tool scores the malnutrition risk as low, medium or high, which helps the workers to develop a strategic plan for improving the dietary intake of the subjects68;
(4) Anthropometric assessment, including weight, body mass index and arm circumference, may be used to calculate muscular circumference of the arm, which indicates the lean body mass.67Additionally, biometric impedance analysis to estimate total body water, extracellular water, fat-free mass and body cell mass helps in identification of malnourished individuals.These parameters may be utilized in building a formal diet plan for the subjects69;
(5) Biochemical tests should be done to confirm the levels of specific micronutrients; however, they should be correlated with clinical parameters.70The nutrients may be supplemented with the presence of specific indications;
(6) Administration of supplements should be further verified through the results of randomized controlled clinical trials in periodontitis subjects.
CONCLUSION
Trace elements are indispensable for the functioning of many physiologic and biochemical reactions.Many of them are metals and their exact role,i.e., patho-physiology of periodontal disease is less evident and debatable.It is one of the most difficult tasks to diagnose trace element de ficiencies nutritionally as well as clinically.So, the need of the hour is to consider the dietary intake of the patients and also the host in flammatory response for the better treatment outcome and for the general health of patients suffering from periodontal diseases.A formal assessment combined with minor dietary shifts may be sufficient to achieve optimal levels for periodontal health.Future controlled clinical trials are warranted to elucidate their exact role in chronic periodontitis.
Author contributions
Concept, design, definition of intellectual content, literature search,manuscript preparation, editing and review: AA, PK.Both authors approved the final mamuscript.
Conflicts of interest
None declared.
Financial support
None.
Copyright license agreement
The Copyright License Agreement has been signed by both authors before publication.
Plagiarism check
Checked twice by iThenticate.
Peer review
Externally peer reviewed.
Open access statement
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
杂志排行
Clinical Trials in Degenerative Diseases的其它文章
- Clinical progress of cell therapy in treating age-related macular degeneration
- Hemodynamic responses of patients with stable coronary artery disease to a comedy film: study protocol for a randomized controlled trial
- Tanreqing injection with ambroxol hydrochloride for heart failure and pulmonary infection in senile degenerative heart disease: a randomized controlled trial
- Relationship between low vitamin D status and extra-skeletal diseases: a systematic review on effects of prophylaxis with vitamin D
- CTDD call for papers
