Active uveitis induces transient refractive error changes
2019-10-12,2,5,6
,2,5,6
Abstract
•KEYWORDS:anterior uveitis; intermediate uveitis; posterior uveitis; pan-uveitis, refractive errors
INTRODUCTION
The overall annual incidence of uveitis is approximately 17-52 cases per 100, 000, with a prevalence of about 38-714 cases per 100, 000[1-4].Females and males are reported to be involved equally[5].Uveitis is the fifth most common cause of visual loss.It accounts for 5%-20% of legal blindness in developed countries and up to 25% in the developing world[6-8].Prolonged visual loss occurs in two-thirds of uveitis patients, with average patients meeting the criteria for legal blindness at some points in their follow-ups[9], however, such complication is not prevalent in anterior uveitis cases.
One of the less explored areas of research is the effect of active uveitis on the refractive status of the eye and relevant changes after uveitis management.Although uveitis can occur at any age, it predominantly affects patients between the ages of 20 to 59[10-11].Considering the high incidence among individuals at working age, refractive changes in uveitic patients might have an important socioeconomic impact.
There are few studies in the literature that evaluated refractive changes in uveitis.An increase has been reported in corneal astigmatism in Fuchs’heterochromic iridocyclitis[12-13].Additionally, myopic shift has been detected in active uveitis secondary to chronic juvenile arthritis[14].Another study demonstrated a hyperopic shift in refraction after several acute anterior uveitis attacks[15].
This study was designed due to the lack of sufficient information about refractive changes in eyes with active uveitis.In this report, the refractive status of active and quiescent phases was compared in uveitic cases with various underlying causes.The effects of age, sex, anatomical location, and severity of disease on refractive changes were also analyzed.
SUBJECTS AND METHODS
The current prospective cohort study was approved by the Ethics Committee of our institute.Institutional review board approval was also obtained.The study was performed in agreement with the ethical principles in the Declaration of Helsinki.Written informed consent was obtained from every enrolled subject.
Subjects referred to our uveitis clinic from June 2012 through July 2015 diagnosed with active uveitis who did not receive any treatment were included.Exclusion criteria were history of any anterior or posterior segment surgery in the involved eye, pregnancy, the presence of dry eye or any ocular surface diseases, posterior synechiae, pseudophakia, epiretinal membrane or cystoid macular edema confirmed with optical coherence tomography, hypotony or intraocular pressure more than 23 mmHg, refractive error ≥±6.00 diopters as well as any condition that prevented refractive error measurement.Cases who developed cataract during the period of study were also excluded due to its potential effect on refractive status.
All patients underwent complete ophthalmic evaluation including best-corrected visual acuity (BCVA)measurement, slit lamp examination, intraocular pressure(IOP)measurement by Goldmann tonometer, and fundus examination by 90 diopter noncontact lens and indirect ophthalmoscopy.The Standardized Uveitis Nomenclature (SUN)criteria were used to classify subjects according to the anatomical locations of inflammation as anterior, intermediate, posterior, and pan-uveitis[4].Subject demographics were also recorded during the recruitment phase.Systemic work-up including appropriate laboratory tests were performed at initial visit for detecting the cause of uveitis.
Affected eyes were installed with 3 drops of tropicamide 1% (Mydrax, Sina Darou, Tehran, Iran)and cyclopentolate 1% (Cyplegin 1% ophthalmic solution, Santen Pharmaceutical, Osaka, Japan)at 5-minute intervals.Cycloplegic refraction was performed 60min after the first installation using an autorefractometer (RM 8800, Topcon, Tokyo, Japan).The sphere, cylinder, and spherical equivalent (SE)were recorded for each eye.SE of refractive error was defined as sphere plus half of negative cylinder.Spherical component was defined as sphere of refractive error.Each refractive component was analyzed as an independent element of refractive error change.Keratometry was performed at the initial visit as well as at 3-month follow-up to ensure that there was no change in corneal curvature.
After initial examination, treatment started accordingly using topical, periocular, and systemic corticosteroids and/or cycloplegic drops as well as other indicated medications.All participants were followed-up for 3mo after primary cycloplegic refraction.The quiescent eyes at 3-month visit were considered for reevaluation of cycloplegic refraction.Quiescent eye was defined as absence of anterior chamber reaction in anterior uveitis and no more than grade one vitreous haze (based on Nussenblatt grading scale)in intermediate, posterior, and pan-uveitis cases.We excluded eyes in which uveitis activity was not quiescent at 3-month follow-up.
StatisticalAnalysisKolmogorov-Smirnov and Q-Q plots were used to evaluate normal data assumptions.To describe data, we used mean and standard deviation, range, frequency, and percentage.Wilcoxon singed-rank test was used to evaluate any changes within study groups.To compare groups, Chi-square test, Fisher’s exact test and Analysis of Variance (ANOVA)were used.Generalized Estimating Equation (GEE)was used to evaluate the simultaneous effect of age, sex, course of activity (acutevsrecurrent), severity, and anatomical disease classification on the change of refractive error.In addition, 95% confidence interval (CI)was calculated for the difference.All statistical analyses were performed by SPSS software (IBM Corp.Released 2013.IBM SPSS Statistics for Windows, Version 22.0.Armonk, NY: IBM Corp.).AP-value of less than 0.05 was considered statistically significant.
RESULTS
In total, 88 eyes from 66 subjects (22 with bilateral disease)fulfilling the inclusion/exclusion criteria were included in this study.The mean age of participants was 34±14 (median: 33; range: 6-65)years (Table 1).The mean IOP was 17±3 (median: 16; range 10-23)mmHg in the active phase and did not change significantly at the quiescent phase (mean: 16±2.4; median: 16; range 12-21)mmHg, (P=0.36).The affected eyes were diagnosed as follows: 46 eyes as anterior uveitis, 30 eyes as intermediate uveitis, 2 eyes as posterior uveitis, and 10 eyes as pan-uveitis.The anterior uveitis group was further divided into non-granulomatous (39 eyes)and granulomatous (7 eyes).Out of 30 eyes with intermediate uveitis, 20 had pars planitis.Both eyes in the posterior uveitis group had toxoplasmosis retinitis.In the pan-uveitis group, five had Behcet’s disease and five had Vogt-Koyanagi-Harada (VKH)disease.Of the 46 eyes in the anterior uveitis group, 25 (54.3%)eyes were in the first attack and 21 (45.7%)eyes in the recurrent phase.All of the involved eyes in the intermediate, posterior, and pan-uveitis groups were in a recurrent phase.
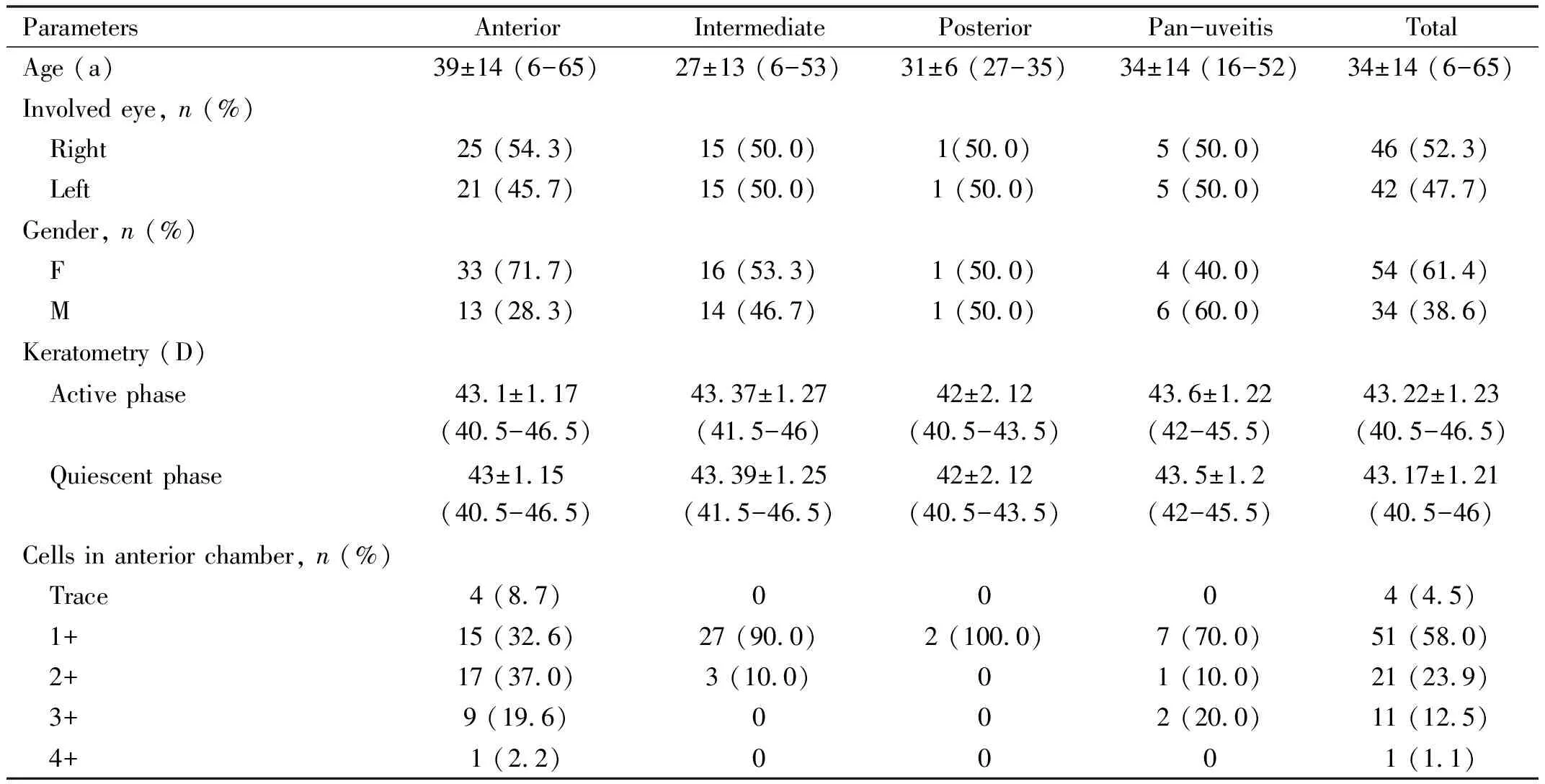
Table 1 Demographic characteristics of patients by type of uveitis Mean±SD (range)
Refractive errors in active and quiescent phases (at three-month follow-up)were evaluated and compared.Considering the mean spherical equivalent, there was a myopic shift in the anterior uveitis group when comparing active (-0.32±1.12 D)and quiescent (-0.09±1.21 D)phases; however, the difference was not statistically significant (Change: -0.23±0.99 D, 95%CI: -0.52 to 0.07,P=0.135).In the intermediate uveitis group however, mean spherical equivalent changes showed a significant hyperopic shift in the active phase (0.25±1.29 D)compared to the quiescent phase (-0.18±1.3 D)(Change: 0.43±0.94 D, 95%CI: 0.08-0.79,P=0.005).This significant hyperopic shift was noted in both subgroups of intermediate uveitis.In the posterior and pan-uveitis groups, we did not observe any statistically significant changes in spherical equivalent (P=0.317 and 0.096 respectively)(Table 2).
Similar findings were observed in the spherical component of the refractive errors.In the anterior uveitis group, a myopic shift (-0.25±0.77 D, 95%CI: -0.5-0)occurred in the active phase in the non-granulomatous subgroup and a hyperopic shift (0.25±0.72 D, 95%CI: -0.42 to 0.92)in the granulomatous one.However, only in the non-granulomatous subgroup did the difference reach a significant level (P=0.039).In the intermediate uveitis group on the other hand, a significant hyperopic shift (0.39±0.79 D, 95%CI: 0.09-0.69)was detected in the active phase compared to the quiescent phase (P=0.003).Statistically significant change was observed only in the subgroup of intermediate uveitis without signs of pars planitis (P=0.014).In the posterior and pan-uveitis groups, no significant change was detected in the spherical component of refractive error (P=0.18 and 0.288 respectively)(Table 3).
Regarding the astigmatism component of the refractive error, there were significant changes in the pan-uveitis group (Changes: -0.3±0.39, 95%CI: -0.58 to -0.02,P=0.043), while other uveitic groups did not show any significant changes (Table 4).
In a secondary analysis, the anterior uveitis group was further classified into four subgroups of acute anterior non-granulomatous uveitis (24 eyes), recurrent anterior non-granulomatous uveitis (15 eyes), acute anterior granulomatous uveitis (1 eye), and recurrent anterior granulomatous uveitis (6 eyes).The acute anterior non-granulomatous uveitis group exhibited a significant shift in the active phase in spherical (myopic shift of -0.64±0.54, 95%CI: -0.86 to -0.41,P=0.003)component (details not included in the tables).In the recurrent non-granulomatous uveitis group, spherical component also had significant change (hyperopic shift of 0.37±0.67 95%CI: 0.01-0.72,P=0.049).The recurrent anterior granulomatous uveitis group showed a significant change in cylindrical component in the active phase (-0.46±0.43, 95%CI: -0.91 to -0.01,P=0.041).

Table 2 Spherical equivalent of refractive error in active and quiescent phases based on uveitis type Mean±SD (range)

Table 3 Spherical component of refractive error in active and quiescent phases based on uveitis type Mean±SD (range)

Table 4 Cylindrical component of refractive error in active and quiescent phases based on uveitis type Mean±SD (range)
We explored the effect of age, sex, anatomical classification, acute or recurrent episodes of uveitis, and disease severity on refractive error changes.Univariate analysis showed that course of disease activity (acute versus recurrent)and anatomical location of uveitis had statistically significant effects on spherical equivalent changes (P<0.001 andP=0.008, respectively).Spherical equivalent changes in the acute episode were lower (about 0.86 D, 95%CI: 0.32-1.4)than those in the recurrent phase.Furthermore, in the anterior, intermediate and posterior uveitis groups, spherical equivalent changes were greater than those in the pan-uveitis group.In addition, multiple regression analysis by Generalized Estimating Equation (GEE)revealed that only course of disease activity (acute versus recurrent)and anatomical location of disease had statistically significant effects on spherical equivalent changes after adjusting for the above-mentioned factors (P=0.003 andP=0.004, respectively).Spherical equivalent changes were lower in the acute (about 0.99 D, 95%CI: 0.61-1.38)than those in the recurrent phase.
DISCUSSION
In the present study, we compared the refractive parameters between active and quiescent phases of uveitis with various etiologies in 88 eyes.Comparing the active and quiescent phases, a myopic shift occurred in the active anterior non-granulomatous uveitis group and a hyperopic shift occurred in the intermediate uveitis group.There was no significant change in the cylindrical component within anatomical groups.Furthermore, regression analysis showed that anatomical location of disease and recurrent episode of disease had a significant effect on spherical equivalent changes.
Several previous studies with limited numbers of subjects and on specific types of diseases evaluated refractive error changes in uveitic cases.While a myopic shift was detected in cases with juvenile idiopathic uveitis in one study[14], a hyperopic shift was demonstrated after multiple acute anterior uveitis attacks in another report[15].In two other papers, a higher cylindrical change was found due to corneal astigmatism in the eyes with Fuchs’heterochromic iridocyclitis compared to their sound eyes[12-13].In another study, severe inflammation of the sclera and choroid with ciliary body detachment and inflammatory supraciliary exudation resulting in acute myopia was reported[16].None of these studies, however, provided detailed information on refractive error changes and only compared active and quiescent phases in a number of eyes suffering from different types of uveitis with various etiologies.
The purpose of our study was to evaluate refractive error changes not related to significant anatomical pathologies.Given our exclusion criteria, we did not include uveitic eyes with very severe inflammation.Such inflammation might have resulted in significant refractive error changes because of cystoid macular edema, choroidal effusions, and exudative retinal detachments.This study included a large cohort of uveitic eyes with various anatomical location involvement and disease entities.
We demonstrated a myopic shift in our cases with active anterior uveitis.There are a few main mechanisms that can alter the refractive status of the eyes in the uveitic conditions: sclero-choroidal inflammation, corneal curvature or axial length changes, cataract formation induced by corticosteroid therapyand drug induced myopic shift.Linetal[17]found a higher myopia incidence among the patients with inflammatory diseases like diabetes mellitus (DM)type 1, uveitis and systemic lupus erythematosus (SLE)compared to the control group.DM type 1, uveitis and SLE resulted in a 1.57, 1.47 and 1.47-fold increase in the risk of myopia respectively, compared to the control group.They discovered that the level of interlukin-6, tumor necrosis factor α and some other inflammatory factors were upregulated in myopic eyes and downregulated following treatment with atropine.They demonstrated that cyclosporine A (an anti-inflammatory agent)can inhibit myopia progression in inflammatory conditions.Scleral or choroidal inflammation would induce ciliary body-lens-iris diaphragm displacement and myopic shift in uveitic eyes[16].Additionally, supraciliary exudation due to inflammation, can cause relaxation of zonular fibers and increased convexity of the crystalline lens, thus would induce myopia[16,23].Corneal curvature (as showed in this study)is not usually affected by active uveitis.Fledeliusetal[14]demonstrated that axial length changes in uveitic patients could alter the refractive error status of the eye.They theorized that the myopic shift noted in juvenile idiopathic uveitic eyes was related to progressive weakness of the scleral connective tissue in chronic inflammation resulting in axial length increment.This mechanism, generally resulting in a permanent shift of refraction, is not applicable to our study since refractive error changes were transient considering the active and quiescent phases.Side effects of drugs used to treat uveitis may result in myopia.Corticosteroid therapy may induce cataract, and sulfonamides compounds may induce myopic shift as an idiosyncratic reaction[18-20].The incidence of new-onset cataract among children with juvenile idiopathic arthritis related uveitis, treated with topical corticosteroid over 4y, has been reported to be elevated (0.04/eye-year)[18].Because our cases were followed for only 3mo, we did not observe detectable cataract formation.On the other hand, Posteletal[21]reported an idiosyncratic side effect of systemic sulfonamides that caused forward shift in the crystalline lens position and lens hydration, which in turn resulted in myopic shift.According to Panday and Rhee[22], the risk of such adverse reaction to sulfonamide would be approximately 3%.However, only two cases of toxoplasmosis in our present study received cotrimoxazole for treatment, and no adverse reaction was detected.The myopic refractive change in our cases with anterior uveitis might be explained by the mechanism in which ciliary body dysfunction due to inflammation leads to relaxation of the zonules and hence an increase in crystalline lens curvature.In contrast, a hyperopic shift was observed in cases with intermediate uveitis including pars planitis.This could be justified by zonular constriction due to the inflammation occurring in pars plicata circular fibers, leading to a decrease in lens curvature.Additionally, primary inflammatory systemic disease may alter the corneal curvature and some topical medications may affect tear film status, resulting in changes to the refractive status of the involved eye[24].However, we neither observed any cases of dry eye during the period of our study, nor significant changes in the keratometry values when comparing active and quiescent phases.While some other studies detected myopic shift in the active phase of VKH cases, we did not find any changes in refractive status in our VKH cases, which can be due to the small number of such cases in the pan-uveitis group[16,23].
Univariate and multivariate analysis showed that recurrent episodes of uveitis resulted in larger refractive shifts compared to the acute episode in our cohort of patients.It may be theorized that with each recurrent insult, the lens-iris-ciliary body complex does not recover its full anatomical integrity resulting in further refractive changes.
The main limitation of our study was the small number of cases, especially those with posterior uveitis and pan-uveitis that prevented us from detecting the possible role of active inflammation on refractive error changes in such patients.Comparing the refractive errors in the active phase of inflammation with the subsequent quiescent phase instead of with the preceding refractive errors could be another shortcoming in our study.As well, we did not measure the central corneal thickness, which might change due to anterior uveitis and might induce refractive error changes.To the best of our knowledge, however, this is the largest case series quantifying and analyzing refractive error changes in active uveitis.In addition, the diversity of the subject population allowed for varied statistical analyses to provide more information regarding refractive error changes in different uveitis entities.
In conclusion, the present study demonstrated that active uveitis induces a transient change in refraction and that the involved anatomical area determines the shift toward myopia or hyperopia.Given the results of this study, patients with active uveitis suffering from decreased vision due to refractive changes should be reassured that this problem may be temporary, and decisions for changing glasses should be postponed to the quiescent phase.
