Laparoscopic ablative techniques
2019-09-09TommasoSilvestriBernardinodeConcilioGuglielmoZeccoliniAntonioCelia
Tommaso Silvestri,Bernardino de Concilio,Guglielmo Zeccolini,Antonio Celia
Urology Unit,“San Bassiano” Hospital,ULSS7 Pedemontana,Bassano del Grappa,VI 36061,Italy.
Abstract
Keywords: Laparoscopic kidney cryoablation,small renal masses,laparoscopic ablative techniques
INTRODUCTION
Although surgery remains the definitive recommended treatment of small renal masses (SRM),ablative techniques (AT) have emerged recently,particularly for tumors < 4 cm,and for those patients who cannot undergo surgery or with imperative indications of nephron sparing surgery (NSS).AT included:cryoablation (CA),radiofrequency ablation (RFA),microwave ablation,laser thermal ablation,and highintensity focused ultrasound.Historically CA and RFA have been introduced first worldwide,and recently longer-term outcomes for these techniques have become available[1-5].They can be performed either laparoscopically or percutaneously with good results in spite of higher reported recurrence and retreatment rates when compared to partial nephrectomy (PN)[6,7].
Historically laparoscopic cryoablation (LCA) has been the most popular approach for performing renal CA[8,9].Conversely,laparoscopic techniques for RFA have been used less in favor of percutaneous RFA,successfully performed under ultrasound,CT,or MRI guidance[10].
Anyway,over the years,also LCA have seen gradual decrease in utilization as image-guided techniques have improved greatly and currently American Urological Association (AUA) guidelines recommend also percutaneous cryoablation (PCA) as the best possible choice[11,12].
In this review,we focused on LCA in relation to its major diffusion and availability worldwide,particularly with SRMs with diameter > 3 cm in comparison to RFA ablation.
CRYOBIOLOGY AND AVAILABLE SYSTEMS
The principles of cryotherapy,including the mechanism of cell injury and cell death,have been well studied[13-15].The main mechanism of cryo-toxicity is the induction of coagulative necrosis in targeted areas.The key factors involved in freezing injury include direct mechanical shock,osmotic shock,and cellular hypoxia.Mechanism of action includes protein denaturation via dehydration,transfer of water from the intracellular space to the extracellular space,rupture of cell membranes from ice crystal expansion,a toxic concentration of cellular constituents,thermal shock from rapid super-cooling,slow thawing,vascular stasis,and increased apoptosis.The delayed or indirect destructive effects of cryotherapy continue primarily because of vasculature disruption,resulting in tissue hypoxia and vascular thrombosis[16].
Stephenson started the first cases of LCA in a canine model and the transition to the second and the third generation of cryoprobes have permitted the use of ultra-thin probes,leading to rapid diffusion of the technique[17].
Currently,the available cryogenic systems,that use pressurized argon gas as the source of freezing,are:the SeedNet® System,the Visual-ICE® System (Galil Medical Inc.,BTG,UK) and the CRYOcareTMSystem (Endocare Inc.,USA).These systems are used to create a conformal freezing pattern up to 25-17 gauge (2.4-1.47 mm) cryoprobe.
ADVANTAGES AND DISADVANTAGES OF LCA
Currently,considerations such as tumor location and complexity as well as patient morbidity must be made when selecting a modality and approach.With initial experience,LCA was utilized primarily for anteriorly and laterally located tumors,and PCA was the method of choice for posterior tumors[18].
The main advantages of LCA are[19]:(1) placement of probes under direct visualization; (2) real-time USguided placement of probes and monitoring of procedure (freezing and tissue viability); (3) easier treatment of anterior or hilar tumors; (4) major ability to displace colon or other organs or nearby structures whenever necessary for a safer ablation.
However,increasing experience during the last two decades has demonstrated that although technically challenging,also anterior tumors can be successfully treated via the percutaneous route,often with adjunctive displacement maneuvers[20].
Hence,the main disadvantages of LCA are[21]:(1) general anesthesia is required (it is not an outpatient procedure); (2) a higher rate of complication in comparison to PCA; (3) less rate of pain control and worst cosmetic in comparison to PCA; (4) higher cost rate in comparison to PCA.
PATIENT SELECTION AND INDICATION FOR LCA
The indications for LCA procedure are the same of all ablative techniques and limited to patients with contraindications to surgical extirpative therapy for comorbidities,advanced age,imperative indications for NSS or have a strong preference for nonsurgical management[1].
Currently,the 2017 AUA guidelines recommend consideration of ablation as an alternative to PN for cT1a renal lesions less than 3 cm in size[12].Otherwise,the European Association of Urology guidelines do not recommend an upper limit of diameter[1].Today there are data supporting CA for cT1b lesions,but in view of higher recurrence rate and complications should be reserved for patients with imperative indications[22].
The location of the mass is a major factor in determining if the mass should be ablated laparoscopically or percutaneously,but the most important factor is the surgeons' experience.
PROCEDURE AND TECHNIQUES
A transperitoneal approach is generally used for anterior and anteromedial tumors,whereas a retroperitoneal approach permits access to posterior and posterolateral tumors[23,24].
Effective cryosurgical tissue injury depends on:(1) excellent monitoring of the process; (2) fast cooling to a lethal temperature; (3) slow thawing; (4) repetition of the freeze-thaw cycle (2 times); (5) freeze cycle length of 8-10 min is commonplace in literature; (6) thaw cycle at least 5-8 min.
Critical factors of the procedure are:(1) placement of the cryoneedles; (2) reach and center a lethal temperature in the central part of the lesion with an ice ball margin of at least 5 mm to avoid a residual or an untreated tumor[25]; (3) iceball imaging as mentioned above.
Key factors to obtain specific success of LCA:(1) take your time to make a better exposure of the renal lesion:the real key is finding the better position for the cryoneedles; (2) triangle disposition of the cryoneedles by putting the different probes at least 10 mm of distance each other; (3) the using of hemostatic agents to prevent or treat bleeding; (4) high experience of the surgeon in NSS:in some rare case,it could be necessary to put sutures.
The number and size of the cryoprobes placed depends on the size and configuration of the mass.Generally,one probe is needed for each centimeter of tumor diameter to be treated.Recently,the use of multiple smaller probe has increased the variety and size of tumors that can be treated.When mobilization of the kidney is feasible,US probes are placed on the contralateral side of the kidney for visualization.Attention should be reserved for relative warming of the ablation zone by large central vessels:the thermal sink effect might be a limit to achieve the lethal temperature.
Laparoscopic cryoablation
Pneumoperitoneum and trocars placement
General anesthesia is required.The patient is placed in a standard flank position.Pneumoperitoneum is usually achieved in two ways:using the open Hasson technique or by placing a Veress needle in the umbilicus of the patient who have not had previous abdominal surgery or in the upper quadrant (left or right).Therefore,at least 3 trocars are placed as for laparoscopic nephrectomy.An extra 5 mm port is inserted as per requirement for suction or retraction.
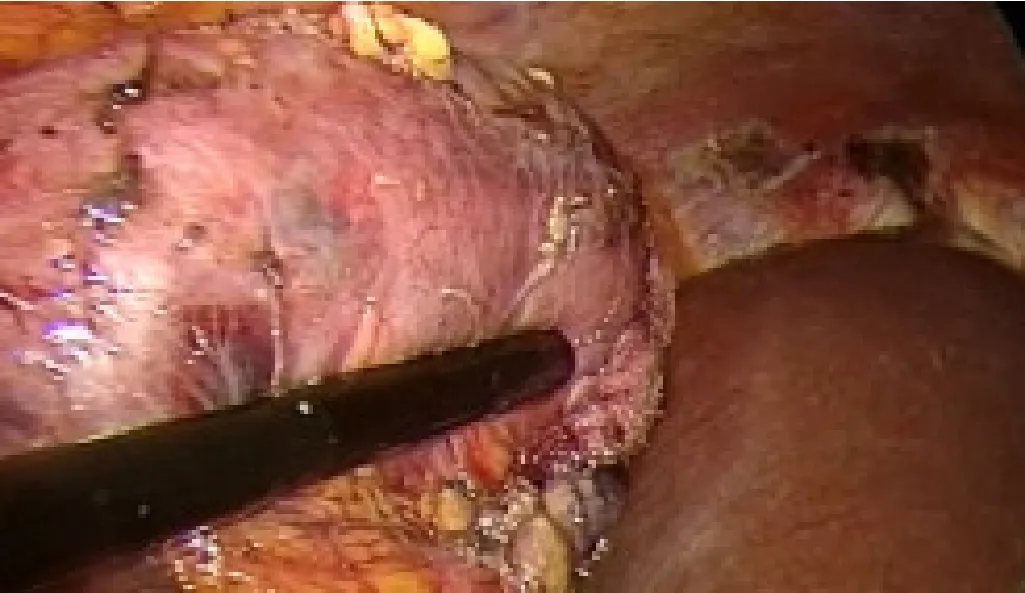
Figure 1.Ultrasound evaluation of the lesion

Figure 2.Under ultrasound evaluation a 1.5 cryoprobe is inserted into the mass
Renal dissection and US
Visceral rotation and reflection of the colon is performed,with a gently kidney mobilization and exposition.Generally,the fat overlying the lesion should be removed,and the tumor region should be carefully dissected.Intraoperative US is performed through the 12-mm trocar.The renal blood vessels are carefully dissected and secured using vessel-loop.Therefore,a Tru-Cut needle biopsy is performed.
Cryoprobes placement
Under US evaluation a 1.5-1.7 mm cryoprobe is inserted into the mass transabdominally through a skin puncture and placed into the lesion.The probe is anchored by freezing the tumor 1-2 mm from the probe [Figures 1 and 2].Generally,a triangulation of one or two additional probes around the first probe could be performed in relation to the size of the lesion.The “killing zone” temperature must be -20 °C or below.
CA cycles are performed as usual,monitored by the US [Figure 3].At the end of the second cycles the needles are gently removed [Figure 4] and hemostatic agents such as fibrin glue (FloSeal - Baxter,Illinois,USA) is then applied to the site.The Gerota's fascia is closed and a non-suction drain is put into the peritoneal cavity.All ports are closed in the usual fashion.
DISCUSSION

Figure 3.First freezing cycle
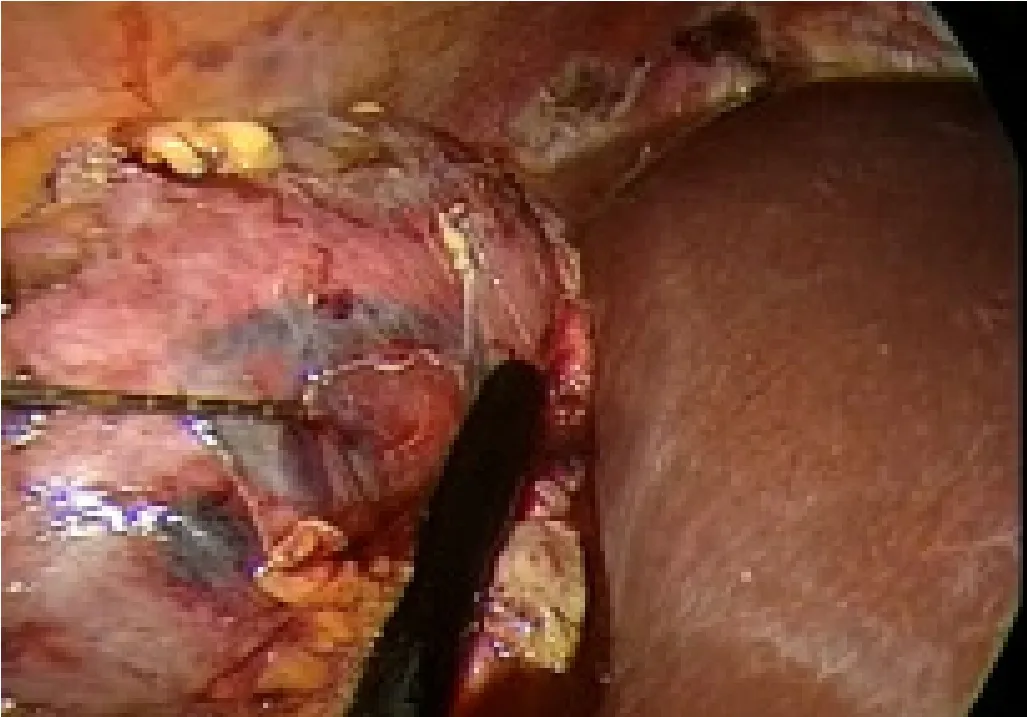
Figure 4.Under ultrasound evaluation the needle is carefully removed
CA and RFA could be an available treatment option for SRMs in selected patients.Quality of the available data and lack of level I evidence do not allow definitive conclusions regarding morbidity and oncological outcomes of CA and RFA.Generally,low-quality studies suggest a higher local recurrence rate for thermal ablation therapies compared to PN.Nevertheless,in currently comparative series no significant differences were reported for OS,CSS,or RFS between RFA and CA[1].Considering PN as a comparator,recently a meta-analysis reported similar complication rates and postoperative functional outcomes between RFA and PN[26].The local tumor recurrence rate was higher in the RFA group than in the PN group but there was no difference regarding the occurrence of distant metastasis.Although the majority of series are retrospective and with different follow-ups,recent studies with a long-term follow-up showed that no statistical difference was found in the 5-year OS,CCS,DFS,and local RFS of RCC patients between RFA treatment and PN treatment [Table 1][27].Johnsonet al.[28]presented data of SRMs with a diameter less than 3 cm with a median follow up of more than 6 years and a subgroup of patients with a minimum 10-year follow up with imaging.The 6-year disease-free recurrence rate of 89% is consistent with the prior published data.This data could suggest that for lesions less than 3 cm RFA oncologic outcomes were similar to efficacy rates of extirpative surgery[28].Regarding CA different studies compared open,laparoscopic or robotic PN with PCA or LCA [Table 2].Oncological outcomes were mixed,not all studies reported all outcomes listed,and some were small and included benign tumors.Globally no study showed an oncological benefit for cryoablation over PN.
Overall,studies comparing renal function before and after CA and PN suggest a degree of functional decline following CA similar to PN.However,in most cases,this is not clinically significant because baseline characteristics of lesions,function and the patient's comorbidities were different.No significant differencewas found between LCA and PCA in renal function outcomes in the two largest comparative studies published so far[29-31].
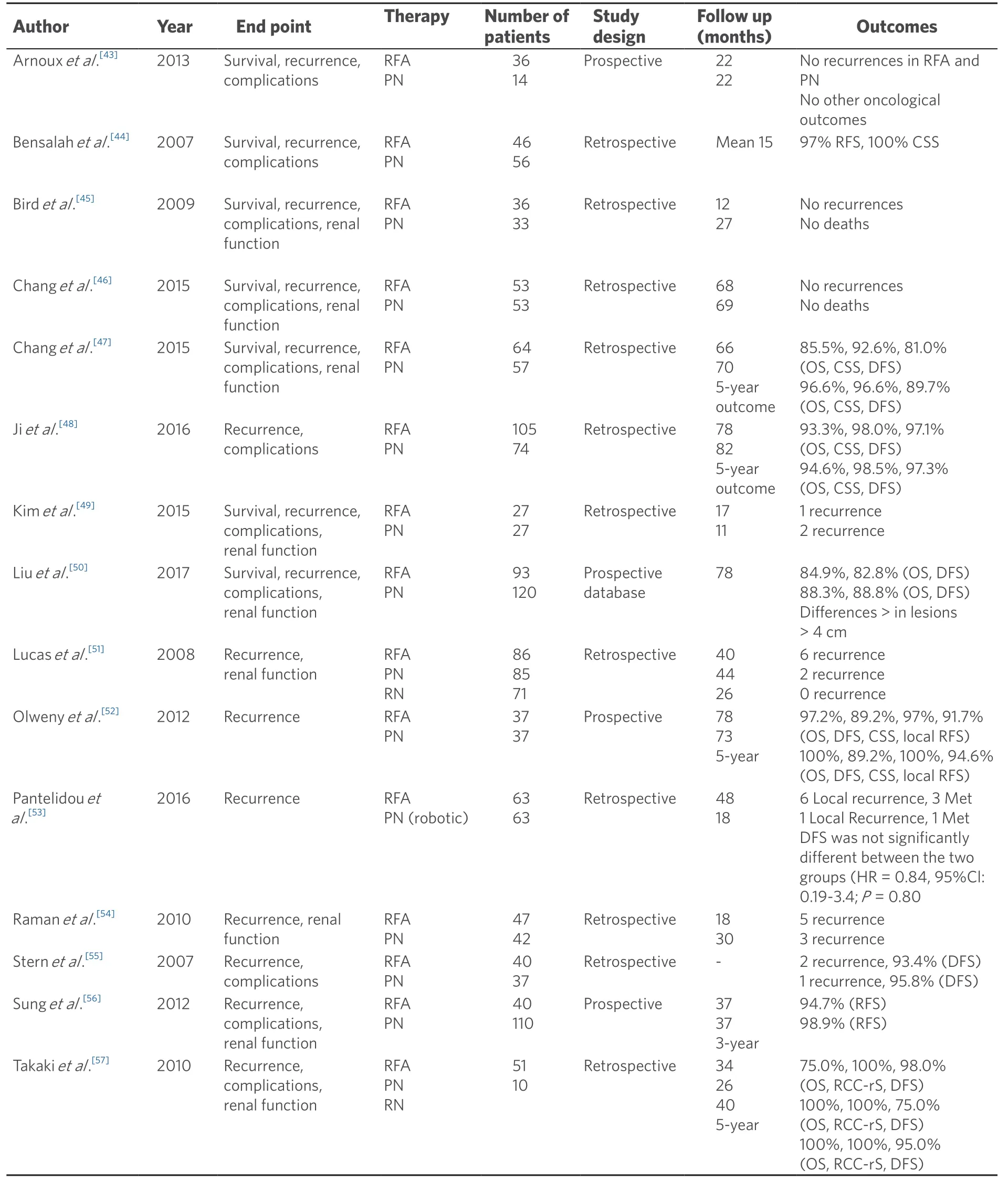
Table 1.Contemporary comparative series comparing radiofrequency with partial nephrectomy and/or radical nephrectomy with oncological outcomes
The reported overall rates of complications for CA procedures range from 7.8% to 20%[30].The overall published complication rates for PCA (7.8%-12.9%) were lower than the rates for LCA (15%-20%)[30,32].
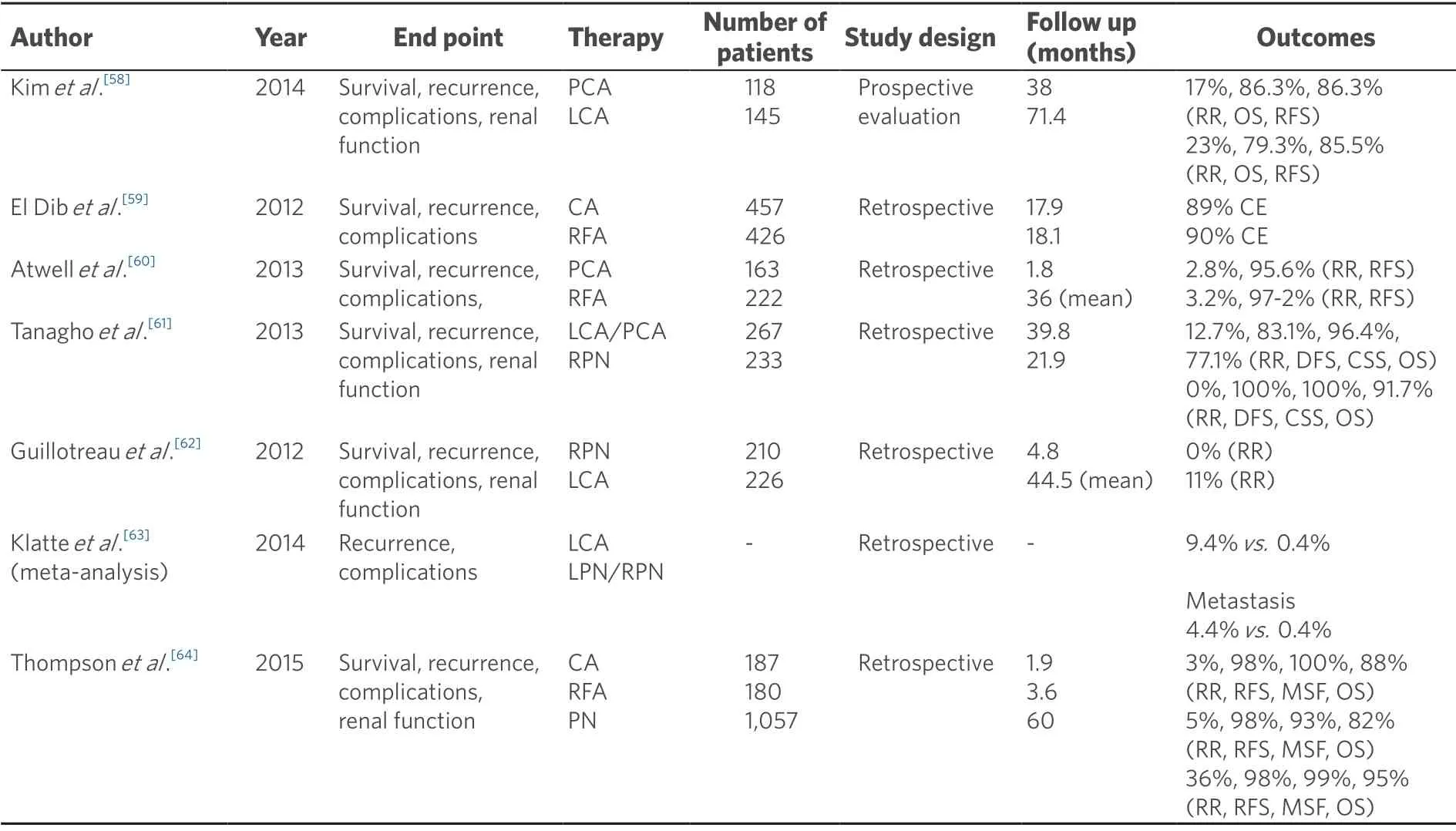
Table 2.Contemporary comparative series comparing cryoablation with different nephron sparing treatment options with oncological outcomes
RFA seems to be no different in Clavien complication rate in comparison to CA,however,Goelet al.[33]founded a lower rate of complication for CA compared with RFA,probably because the freezing-induced injury is less destructive than heat-induced one[33,34].Generally,the most common complications during the procedure or post-operative are bleeding and rupture of the iceball.
There is no consensus on the definition of recurrence after treatments for SRM and particularly after AT.Local recurrences mostly occur at the site of the primary treatment within the kidney.Conversely,extrarenal local recurrences are rare[35,36].Today,most analyses have shown lower specific cancer mortality for PN compared to non-surgical treatments.In general,local recurrence rates after CA are higher than after surgery (2%-11%vs.1%-2%)[37,38].
Ideally,histopathological confirmation and re-biopsy of previously treated lesions would improve data of recurrent or residual disease.Conversely,in the literature,the majority of reports relied on radiographic evidence of enhancement to define both residual and recurrent disease.PCA had a higher rate of residual disease/primary treatment failure in comparison to LCA:PCA residual disease seems to be more frequent and to occur earlier than LCA,even if the length of follow-up between groups is difference (approximately 14 months longer for LCA)[29].
Zargaret al.[30]found no significant difference in OS or RFS at 5 years between PCA and LCA.Conversely,in other studies seems that a lower rate of patients in the LCA group experienced a local recurrence as compared with the rate of PCA group[30].
Factors that might have contributed to the differences in residual and recurrent disease between PCA and LCA are the size of the lesion,the anatomical location,and the probe size and number (in LCA tendency to use wider probes).
To date,cost issues have not played a major role in driving decisions among treatment options.However,as health care expenses continue to rise,cost concerns are likely to play an ever-increasing role.Different studies have assessed cost,but their results differ based on some key postulated differences such as the period of observation,the definition of success and complication rates,different health-care systems,and also whether those with benign biopsies should be treated or followed up.
Changet al.[39]analyzed the cost-effectiveness of all NSS options for SRMs and concluded that for healthier younger patients (aged 65 years with a < 2 cm lesion or aged 75 years with a 3-4 cm lesion),immediate surgery represents the optimal NSS option with the best incremental cost-effectiveness ratio.Surveillance with possible delayed PCA was a cost-effective option for older patients or those with increased perioperative mortality risk.Observation represented the best strategy for patients who are poor surgical candidates and who had a life expectancy < 3 year.It is worth noting that laparoscopic AT was not cost effective in any scenario regardless of age,comorbidities,and tumor size[39].Bhanet al.[40],comparing RFA,CA,and observation for the treatment of SRMs,established that active surveillance with no initial biopsy and with subsequent PCA in case of disease progression was more cost-effective than immediate CA with or without biopsy and other observation options.They found that in terms of cost-effectiveness,all CA techniques were superior to RFA procedures owing to higher rates of retreatment for RFA[40].Reporting direct comparative costs of LCA and PCA,LCA was significantly more expensive than PCA (3.5 times on average)[41].However,these values need to be adjusted for patient and tumor characteristics to better gauge the cost incurred by each approach.Ideally,we have to consider also the cost of readmission,ongoing surveillance,and retreatment into the analysis.
Furthermore,Linket al.[42]analyzed the cost-effectiveness of different treatment options,particularly comparative analysis between PCA and laparoscopic treatment options.The PCA was 2.2-2.7 times less costly than the other options and resulted in a cost savings of $3625 to $5155 per case.For Open PN,Laparoscopic PN,and LCA,the operative time and hospitalization accounted for 69%-91% of the cost.The Laparoscopic PN and LCA were cost advantageous over PCA only when more than five cryoprobes were used during the percutaneous procedure[42].
CONCLUSION
AT seems to be a valid treatment option that could reduce complications and general impairment of classical surgical procedures.Finding the perfect candidate for AT is challenging due to the lack of objective criteria in the literature and of standardized techniques.Notably,the percutaneous approach seems to have lower complications rate than laparoscopic approach,especially in CA,and it can offer shorter hospital stay and faster recovery,which can be particularly appealing in an era of cost restriction in healthcare.Afterward,in the era of a multidisciplinary approach and tailored therapy,LCA could be a useful instrument to manage lesions for which PCA might have a failure or could be difficult and unfeasible.Hence,LCA should be collocated in a middle position for the management of SRM between PCA and NSS.Nevertheless,the application of this approach is dictated by the available technology and specific expertise of each center.
DECLARATIONS
Authors' contributions
Made contributions to conception and design of the study/review,performed data analysis and interpretation:Silvestri T,Celia A
Made substantial contributions to conception and design of the study/review,performed an entire revision of data analysis,re-interpretation and the revision for editors:Silvestri T
Performed data acquisition:de Concilio B,Zeccolini G
Availability of data and materials
Not applicable.
Financial support and sponsorship
None.
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Copyright
© The Author(s) 2019.
