Management of pain in peripheral vascular disease with Jalauka Avacharana followed by Manjishtadi Kshara Basti-a case series
2019-09-03HerambPundalikHattikarGururajaTantry
Heramb Pundalik Hattikar,Gururaja D Tantry*
1Department of PG studies in Shalya Tantra, Muniyal Institute of Ayurveda Medical Sciences, Manipal, Karnataka,India.
Abstract Peripheral vascular disease with increasing prevalence rate is one among many conditions where a dependable cure is still elusive. Peripheral arterial disease (PAD), of which is a common form that results from atherosclerosis of arteries leading to reduced blood flow to the extremities. Commonly affecting the lower extremity, PAD presents with pain during ambulation, which is known as “intermittent claudication” which later manifests into “rest pain”.Due to the cry of the dying nerves, the pain is so severe that even common analgesics fail to relieve it. It is observed that the pathogenesis and clinical manifestation of PAD has striking similarities with “gambhira vatarakta” which is characterised by burning sensation, severe pain, excessive sweating, thirst, suppuration and tenderness. Keeping this view in mind the patients diagnosed with vatarakta were selected for jalauka avacharana(Leech therapy) followed by manjishtadi kshara basti (Decoction enema prepared by adding several drugs). This protocol showed remarkable results in relieving pain and ultimately vyadhi upashaya.
Keywords: Peripheral Vascular Disease, Intermittent claudication, Rest Pain, Vatarakta, Jalauka Avacharana,Manjishtadi Kshara Basti.
Introduction
Peripheral arterial disease (PAD) is a common form of peripheral vascular disease, where in atherosclerosis results in narrowing of an artery leading to reduced blood flow to the extremity. The risk factors for the development of peripheral arterial atherosclerosis are diabetes mellitus, hyperlipidaemia, hypertension, and cigarette smoking [1]. Especially, smoking is linked with PAD, although the mechanisms are still obscure.Also people who have a family history of atherosclerosis, obese and physically inactive, are associated with PAD. Each of these factors contributes not only to the development of occlusive peripheral arterial disease but also worsens the disease. The patients may present with intermittent claudication and the symptoms caused by critical limb ischemia,including rest pain, a pain in the soles of the feet,particularly when the feet are elevated,such as when in bed, tissue loss, consisting of arterial insufficiency ulcers, that heal slowly or not at all, and gangrene. In Ayurveda the disease can be correlated withvataraktacaused due toavarana.The vitiation ofvataandraktaleading to obstruction in the flow ofvataand subsequentlyraktaproduces clinical symptoms that start fromhastaandpada[2].These shows similarity in the symptomatology with PAD. As the treatment approach is concerned despite of availability of various treatment modalities on medical and surgical grounds,a dependable cure is still elusive. These many options does not with stand to the complexity, generalization and rapid progression inherent to the disease. In its most severe form, critical limb ischemia, patients are often treated with lower extremity amputation. But studies have shown that the risk of contralateral lower limb amputation and death after initial lower limb amputation is very high [3]. Considering the above challenges, the main treatment goal targeted to alleviate pain and primarily to save the limb; a treatment strategy was adopted in treating cases of PAD -withjalauka avacharan(leech therapy) andmanjishtadi kshara basti(decoction enema) and wound management. In this paper, four cases, which were reported to out patient department (OPD) and diagnosed as PAD in different stages of the disease progression, were managed with this protocol and will be discussed as follows.
Case history
Case 1
A 45-year-old male, fisherman by occupation reported to OPD with the complaints of blackish discoloration in the right leg and pain in calf region on walking present since one year. The patient had an amputated left leg wearing prosthesis (Figure 1). On history taking, patient was hypertensive with a history of below knee amputation done in 2015 as he had an attack of acute limb ischemia. Personal history revealed chronic smoking since 25 years. Clinically,vitals found to be normal, peripheral pulses feeble.Arterial Doppler study of right leg showed diffuse atherosclerotic changes in the popliteal artery,proximal and mid posterior tibial artery -having low monophasic wave forms. The patient was admitted to indoor patient department (IPD) for further management. Blood investigation showed random blood sugar(RBS)-96mg/dl.
Case 2
A 48 year old male, attender in jewellery shop by occupation reported to OPD with the complaints of non-healing ulcer above the ankle of left leg associated with excruciating pain. Having foul smell and pus discharge from the wound. The patient was apparently normal before one year developed bilateral pain in both legs. One month back a reddish -black spot was seen which further developed into a wound. He was under modern treatment.Twice debridement was done.But failed to heal. Patient was hypertensive and diabetic with the history of habitual smoking and drinking alcohol occasionally. Clinically, the patient had an increased body temperature. Presence of non-healing ulcer over medial (Figure 2A) and lateral malleolus (Figure 2B) of size approximately 10x7cm and 5x5 cm respectively.Punched out edges, with foul smelling pus discharge and slough. Arterial doppler study revealed diffuse narrowing of the anterior &posterior tibial arteries with decrease flow distally.The patient was admitted to IPD for further management.Blood investigation conducted at our hospital showed fasting blood sugar (FBS) - 128 mg/dl, postprandial blood sugar (PPBS) -153mg/dl, serum creatinine-6mg/dl,Haemoglobin(Hb)-9.4 gm%.
Case 3
A 74 year old male, hotel businessman by occupation came to casualty with the chief complaint of excruciating pain in right leg especially the foot.Associated with a non-healing ulcer of an amputated 4th toe (Figure 3).The patient had a history of gangrene of 4th toe for which he underwent toe amputation in a city hospital but the disease progressed and was further advised to undergo below knee amputation. On history taking patient was found to be hypertensive and diabetic since 20years and also a chronic smoker. On examination, he had an increased body temperature. Locally the ulcer was non-healing embedded with slough. Arterial Doppler study had shown Right- anterior tibial artery with focal area of stenosis-tibio-peroneal trunk 50%. posterior tibial artery 70% stenosis. For further management was admitted to IPD. Blood investigations showed FBS-122mg/dl,PPBS-186 mg/dl.
Case 4
A 70 year old male, a hotel serviceman and farmer by occupation reported to the hospital with chief complaint of excruciating pain in right leg.The patient had pain in right lower limb since 3 years which gradually increased and was specifically severe after walking a short distance. Later patient developed blackish discoloration of right little toe. He had the same history with the left leg for which his left lower limb was amputated as it manifested into gangrene.He also had a history of smoking and was a known case of hypertension and diabetes mellitus. Clinically the right little toe showed progression of gangrenous changes and decreased temperature locally (Figure 4).The patient was admitted to IPD for further management.Blood investigations were done which showed RBS-138 mg/dl,PPBS-138mg/dl,serum uric acid-1.3

Figure 1 Ischemic changes in contralateral limb in case 1

Figure 2 Medial malleolus ulcer in case 2

Figure 3 Amputated toe with non-healing ulcer in case 3

Figure 4 Gangrenous changes of little toe in case 4
Therapeutic intervention
Vataraktabeing a systemic disease, the management was planned on lines ofVatarakta chikitsaaimed at controlling the vitiatedVata,Pittaand to normalise theRaktadusti.
Oral Medications
The underlying pathophysiology for disease manifestation isavaranjanyawhich is due the vitiation ofvataandrakta. Thus Oral medicines were selected which are indicated inVataraktadisease.Guduchiis the drug of choice as explained in the classical texts.Gugguluis one extraordinary drug that possessesAnabhishyandhi, Snigdha, andSroto Shuhdhikarak. So Tablet Kaishoraguggulu[4] was selected.Manifestation of gangrene was present,TabletGandhaka rasayana[5] was added as it israktaprasadakahelpful to inhibit disease progression,promote wound healing and to control infection. As this is anavaranacondition, with predisposing factor as madhumeha;Rasayanadrugs were preferred, Tab.Shivagutika/Tab. Chandraprabha Vati[4] was added(Table 1).
Panchakarma therapy
According to classics,shodhanatherapy is one of the means of management ofavaranajanya vyadhis. Asvataraktais anavaranajanya vyadhi,bastiis efficacious in the management.Sushrutahas indicatedbastiinadhakatyasthita -vata dushta vranahavingatyartha vedana[6]. Kshara Basti[7] which is mentioned byChakradattaandManjishthadi Kwatha[8] which is mentioned bySharanghdhar SamhitaBased on these viewsmanjishthadi kshara bastiwas considered for the treatment.The patients were advised for treatment ofyoga basti karma.ForYoga Basti-Manjishthadi Kshara NiruhaandMatra Basti(Anuvasana) with Dhanvantara taila[9] were given alternatively for 8 days. In whichManjishthadi Niruhawas given 540ml on empty stomach in the morning andMatra BastiwithDhanvantara Tailaabout 60 ml was given in afternoon after meals.
The Yoga Basti
The course and the ingredients ofYoga Bastiare shown in Table 2 and Table 3.
Ulcer management
Jalauka avacharan(Leech therapy) has been indicated for both types ofVata-raktawhere pain, burning and redness found as perCharaka chikitsa[10]. As the patients had developed non healing ulcer- to remove slough and facilitate wound healing, it was indicated.Followed by daily dressing withEshwari mula kashaya.Eshwari(Aristolochia indica) is a medicine used in folklore practice in managememnt of snake bite poisoning,thelepaofmulais applied at the site of bite.Considering the disease having similar features of haemotoxicity and neaurotooxicity,it was used.
Observation and Results
Assessment Criteria
Pain
The main characteristic feature of peripheral arterial disease is pain.In initial stage the patient presents with claudication. This exercise-induced pain further manifests into pain at rest which is a sign of critical limb ischemia. The grading was done on the basis of‘Visual Analogue Scale’(VAS). Scale of 0 to 10, with 10 indicating most severe pain.
Claudication Distance
Patients with intermittent claudication have limited exercise and walking capacity.The most common estimation of walking capacity impairment is the relative claudication distance (distance until pain occurs).The patient was asked to walk on a flat surface and the distance was measured in metres.
Palpation of Periperal Pulses
Peripheral pulses are compared with the opposite side and the presence of any thrill is noted.Femoral,popliteal, posterior tibial,and dorsalis pedis pulses are assessed.The femoral pulses are palpated half way between the anterior superior iliac spine and pubic symphysis on each side. The popliteal artery lies between the heads of gastrocnemius and the pulse is assessed with the knee slightly flexed using the index,second and third fingers to push the popliteal artery against the tibia. The posterior tibial pulse is palpated just behind the medial malleolus and dorsalis pedis pulse over the navicular bone lateral to the extensor hallucis longus tendon (dorsum of foot). Pulses recorded as present,weak or absent.
Discoloration of the limb
The affected limb and its fellow side is put by side and the color is compared. Since both the limbs may be simultaneously affected, it is necessary to compare with the clinician’s own skin. When the gangrene is threatening, there is often marked pallor of the limb. It was noted and recorded as discoloration present or absent.
Wound
Multiple occlusive lesions of the limb arteries,coupled with functional and structural change in the microcirculation,are responsible for inadequate tissue perfusion, leading to the formation of skin ulcers andnecrosis. In the study the patients with non-healing ulcer underwent local ulcer treatment.Hence the assessement of the overall treatment of PAD was done on the basis of wound healing.Healed or non-healing.
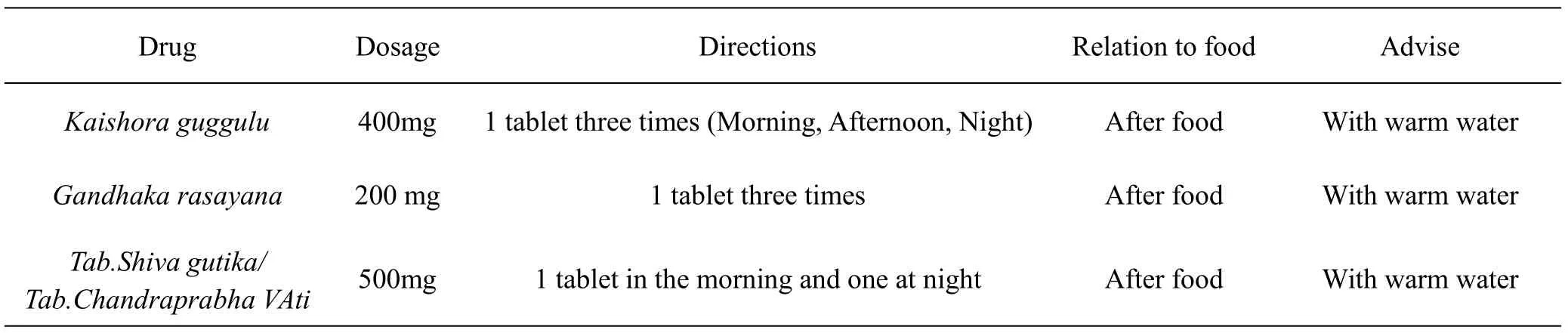
Table 1 The oral medications of these PAD patients
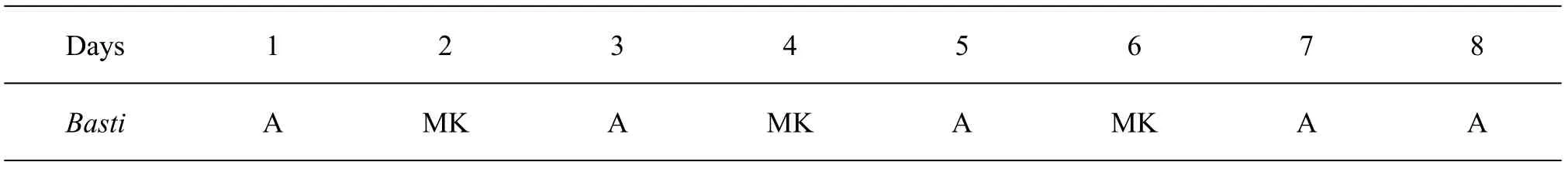
Table 2 The course of Yoga Basti
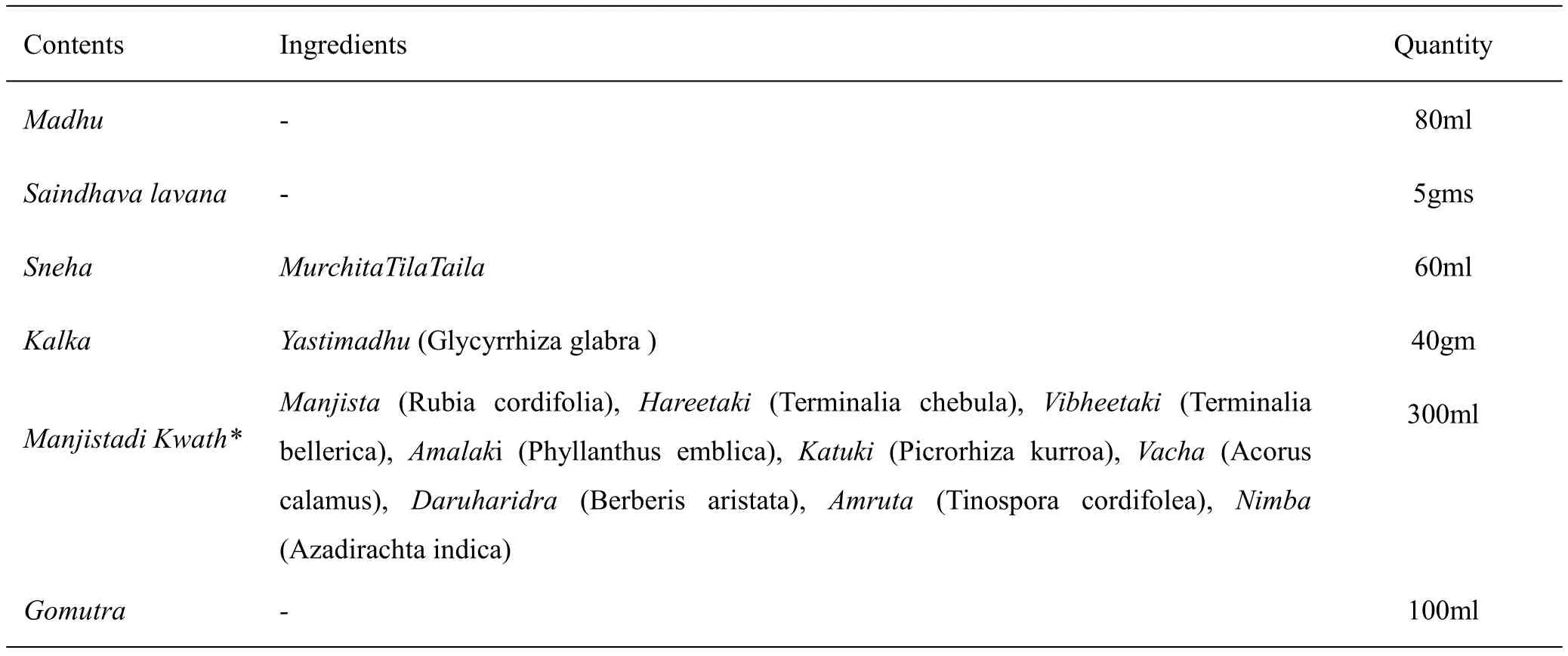
Table 3 The ingredients of Manjishthadi Kshara Basti
Buerger's Test
The patient is made to lie in supine position and the affected leg is raised vertically upwards,a marked pallor develops in 2-3 minutes (normally slight change of colour occurs). Lowering the leg below the horizontal causes marked cyanotic congestion. The angle of circulatory efficiency is the angle at which a reddish hue returns when the raised and blanched leg is gently lowered below the horizontal.
Results
Response to Treatment
In all the four cases, patients responded well to the treatment(Table 4).
Case 1
With the administration ofbastithe intensity of pain started reducing.At the end ofbasti karmathe patient improved with claudication distance and could walk longer distance. He was advised to come for follow up on every 15th day. The patient was asked to continue with oral medications for 3 months.At the end of three months patient had no pain on walking. The discoloration improved to a moderate level. The treatment protocol showed significant result in alleviating pain ultimately in saving the affected contralateral limb.(Figure 5)
Case 2
Patient responded well to the treatment,pain in the feet gradually started reducing with the administration ofbasti.In case of ulcer,unhealthy gangrenous tissue was debrided andjalauka avcharanwas done.Post-jalauka avacharanfurther reduced the pain.Dressing was done on daily basis. After completion ofbastikarma, the patient was advised to continue with oral medications and daily dressing. At the end of 15th day the ulcer showed signs of healing with presence granulation tissue.The same treatment was followed for 3 months.At the end of 3rd month the ulcer completely healed.There was complete reduction in rest pain. The claudication distance increased and he could walk 1 km without rest. And blood report showed serum creatinine-2.1 mg/dl.(Figure 6)
Case 3
With due course of treatment patient significantly improved. Administration ofbastishowed remarkable results. Rest pain started reducing on 10th day itself.Unhealthy gangrenous tissue was debrided and application ofjalaukawas done followed with daily dressing withkashaya.At the end of completion of thebasti karmapain in feet & discoloration improved.After 15days of treatment, ulcer began to show signs of healing with development of reddish granulation tissue at periphery. Dressing was continued on daily basis. The patient was advised to continue with oral medications for 3 months.At the end of 2nd month the ulcer completely healed.(Figure 7)
Case 4
After the completion ofbastikarma, pain significantly reduced.Jalauka avcharandone at the site of discoloration i.e at the little toe reduced signs of gangrene formation. On 15th day of follow up, patient had no rest pain with increased claudication distance.The patient was asked to continue with oral medications for three months.(Figure 8)
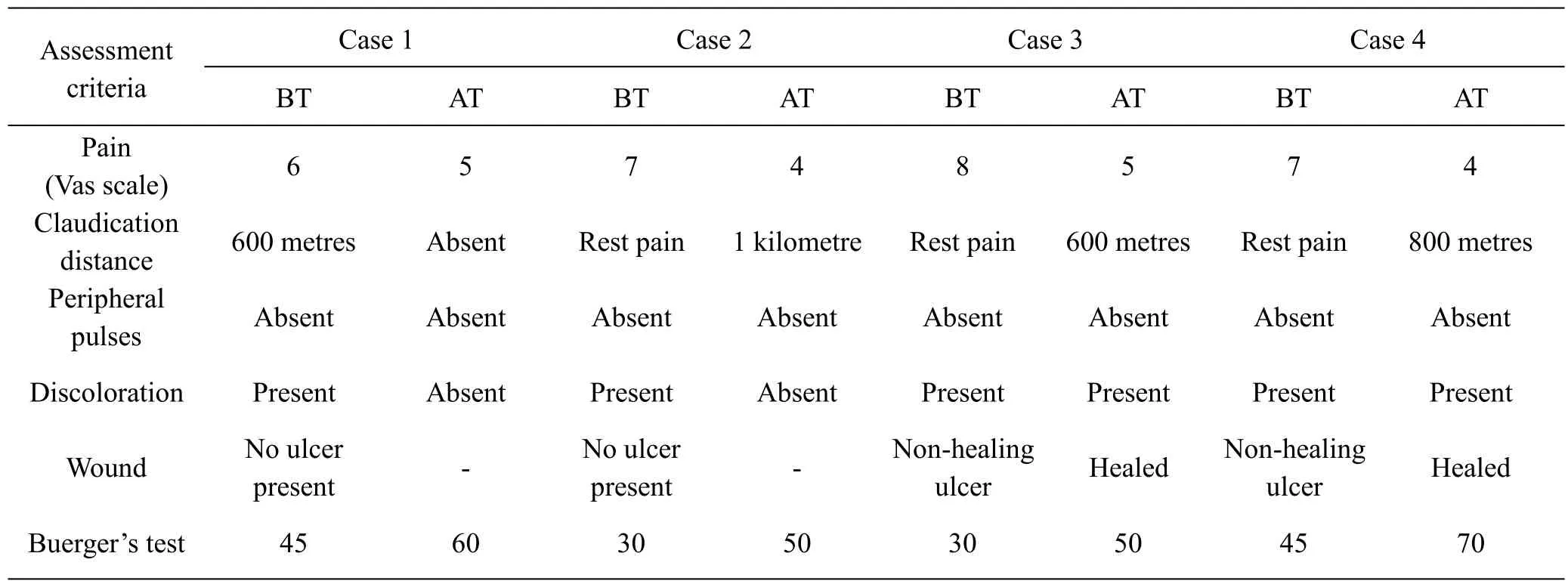
Table 4 Response to treatment

Figure 5 Response to treatment in case 1
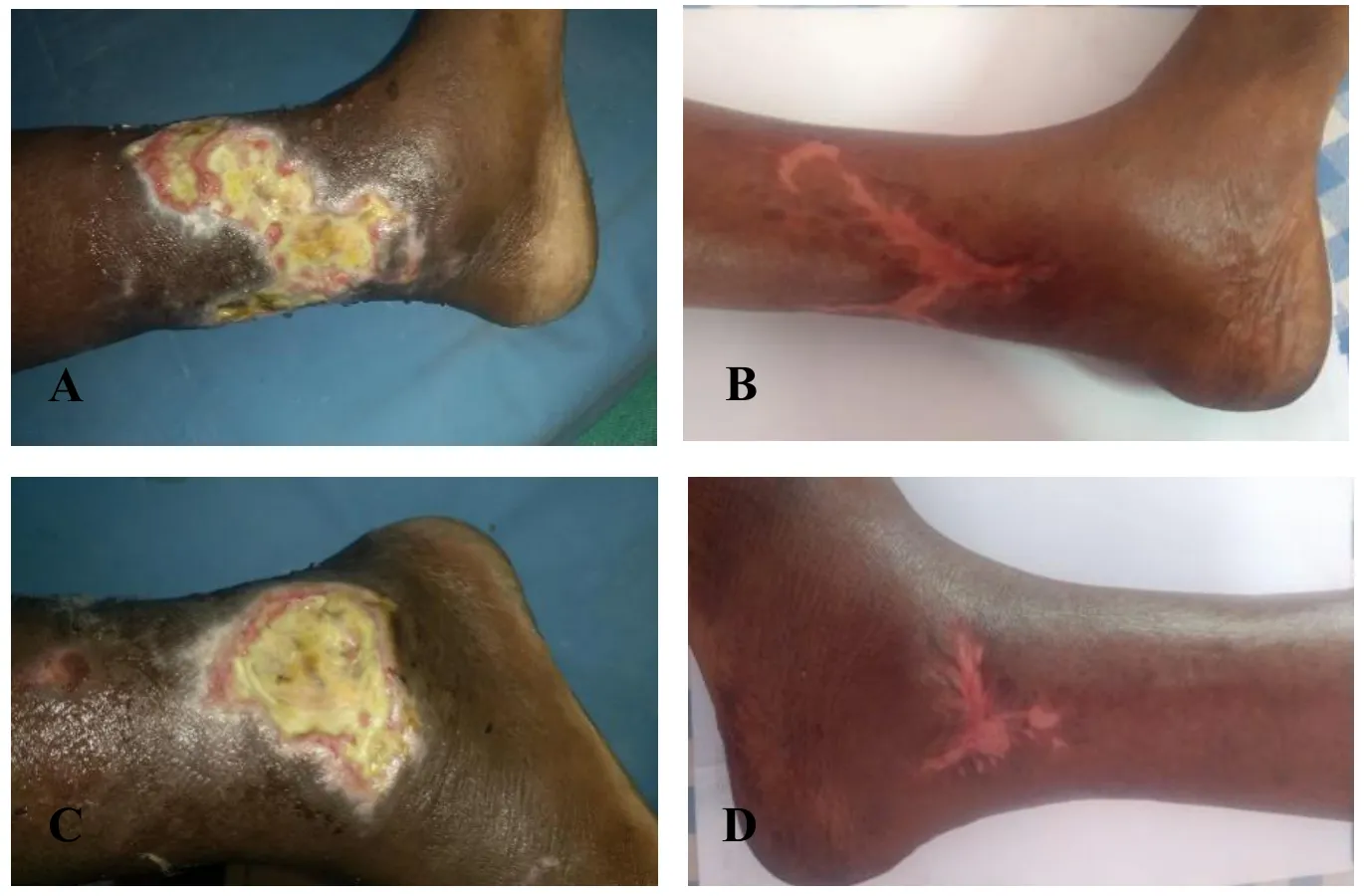
Figure 6 Response to treatment in case 2
Discussion
InAyurveda,Vataraktais explained as a disease manifested because ofavaranapathology. The scenario ofVataraktaoccurred owing to the margavarana pathology, which can very well be correlated with atherosclerotic peripheral arterial disease. In the above cases, having the predisposing factor as diabetes mellitus withnidana sevanaof smoking (tobacco), eating salty food (ushna-tikshna)lead totridosha dushtiandrakta dushtias tobacco isvisha dravya. Sincesira(arteries)isupadhatuofraktalead to pathology ofvatarakta. The resultant obstruction in the flow of bothvataandraktaat the peripheral vessels of lower limb manifested in leg pain,discoloration, burning sensation, ulceration and eventually gangrene.
In such casesSamprapti vighatana(chikitsa) can be achieved by relievingavaranaand correcting the vitiatedvataandrakta.Guduchiis the drug of choice in the management ofVatarakta.GuduchipossessTikta rasa,Madhura vipakaandUshna veerya. It isVatahara,Rakta prasadaka, shleshma rakta vibandaghnakrut, Rasayanawhich is indicated inVata-rakta avaranacondition [11]. Studies on Tinospora cordifolia have shown that it is having anti-inflammatory,anti-oxidant and immunomodulatory action [12].Gugguluis one extraordinary drug that possessesAnabhishyandhi,Snigdha, andSroto Shuhdhikarak[13]. Thuskaishor gugguluhas shown expected results.Tab.Gandhaka rasayanais havingyogavahi guna. Gandhakaas main ingredient and manybhavana dravyasit israktaprasadaka,pittaghna,dahashamakaandrasayana. Considering the predisposing factor as diabetis mellitus in all the cases, Tab.Chandraprabha vati/Tab.Shivagutikawas chosen as theshilajituis drug indicated inmadhumeha.The peculiarity ofshilajituis it doeslekhana karmawithout doingapatarpana.Charakhas indicated use of it in raktaja vyadhis [14].Previous studies have shownmanjishtadi kshara bastito be significantly effective in reducing leg pain, claudication and inhibited further manifestation of gangrene by reversing the pathology.Manjishtaand other drugs in theMahamanjistadi KashayaandManjishtadi Niruha bastihaveraktaprasadakaproperty and indicated inRaktadusticonditions. The main drugmanjishtais also known with synonym“vikasa”as it causesvikasa(vasodilation) insira[15]. Added to it Rubiadin [16]present inManjishtahas antioxidant property.Gomutra arkaacts as debriding agent.Dhanvantara tailaexplained inastang hridayam is said to besarva vata vikarajita[17] hence thematra bastiwas administered with it since the pain is the main symptom of the disease.
In case of PAD disease and ulcer management,Jalauka avacharanhas proved effective [18]. Leech possesses various metabolically active substances in its saliva. It has hirudin, the anticoagulant and an anesthetic also. Bdellinsis is another compound that acts as an anti-inflammatory agent by inhibiting trypsin as well as plasmin. It also inhibits the action of the acrosin. Another anti-inflammatory agent is the eglins.The saliva also contains a vasodilator agent, and they are the histamine-like substances, the acetylcholine, and the carboxypeptidase A inhibitors.All these act to widen the vessels, thus, causing inflow of blood to the site [19]. In folklore practiceEshwari mula kashayais used forlepaat the site of snake bite as an anti- poisonous drug.As it is known that Snakes are neurotoxic and hemotoxic-similarly incase of PAD the pathology is related to arterial circulation and nerves. Understanding the mode of action in snake poisoning it has been used in PAD.Dhavanand dressing withksahayafacilitated wound healing with formation of new granulation tissue.
Conclusion
Knowledge of pathogenesis and Complications of a disease according to Ayurveda and Modern science is necessary for proper planning of the treatment. In modern the approach of PAD with acute limb ischemia is amputation but the risk of contralateral limb amputation and death after initial lower limb amputation is proved to be high. In an attempt to treat PAD cases with four different disease progressions purely on the principles of ayurveda whereJalauka avacharanfollowed byManjishthadi Kshara Bastiwas used showed significant results. With the success,it can concluded that the pain presented as intermittent claudication or rest pain and end stage gangrene where surgical intervention is required can be effectively managed and affected limb(s) can be saved byyuktikrutaoral medications.jalaukavacharan&Manjishthadi Kshara Basti.
Abbreviations
PAD, peripheral arterial disease; OPD, out patient department; IPD, indoor patient department; RBS,random blood sugar; FBS, fasting blood sugar; PPBS,postprandial blood sugar; Hb, Haemoglobin; VAS,Visual Analogue Scale.
Acknowledgments
None.
Competing interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
杂志排行
Clinical Research Communications的其它文章
- Design and application of a new multifunctional uniform for hemodialysis patients
- Analysis of drug use rules of Chinese medicine master Liu Shangyi to treat thyroid cancer
- A meta-analysis of Duhuo Jisheng decoction combined with non-operative therapy on lumbar disc herniation
- Research progress in pharmacological and clinical application of Jingui Shenqi pill