Hydrogen gas therapy induced shrinkage of metastatic gallbladder cancer: A case report
2019-08-14JiBingChenZhongBaoPanDuanMingDuWeiQianYangYangMaFengMuKeChengXu
Ji-Bing Chen,Zhong-Bao Pan,Duan-Ming Du,Wei Qian,Yang-Yang Ma,Feng Mu,Ke-Cheng Xu
Abstract
Key words: Hydrogen gas; Metastatic gallbladder cancer; Case report
INTRODUCTION
Gallbladder cancer (GBC) is the sixth most common gastrointestinal cancer and the sixth highest cause of cancer-related deaths in China[1].Despite improvements in the diagnosis and treatment of GBC,the majority of the patients are usually confirmed as having metastatic GBC (mGBC)[2,3].Due to the high incidence of lymph node or distant metastasis,the 5-year overall survival (OS) rate for GBC is only 5%[3,4].In mGBC patients who are not candidates for surgery,the National Comprehensive Cancer Network (NCCN) guidelines reco-mmend the use of biliary drainage,chemotherapy,clinical trials,and the best supportive care available.At present,there are few alternative options,and new and more effective methods are urgently required.
In patients with cancer,the treatment strategy,outcome,and prognosis are strongly dependent on immune status.CD8+T cells become exhausted by persistent stimulation by tumor antigens,resulting in cessation of proliferation,cytokine production,and immune function[5,6].The preventive and therapeutic effects of hydrogen in various diseases,including cancer,have been investigated in several studies[7-9].Hydrogen was recently reported to stimulate peroxisome proliferatoractivated receptor γ coactivator 1α[10],which enhances mitochondrial function[11]and thus,may rescue exhausted CD8+T cells.In an advanced study of the effects of inhaled hydrogen gas in 55 patients with stage IV colorectal cancer[12],Akagiet al[12]identified accumulation of terminal programmed cell death 1 (PD1)+CD8+T cells as a significant index for poor prognosis,with reduction in terminal PD1+CD8+T cells and accumulation of terminal PD1-CD8+T cells following hydrogen gas treatment found to be significantly associated with improved progression-free survival and OS.
Here,we present the case of a 72-year old Chinese woman with stage IIIA GBC who was treated with irreversible electroporation (IRE) and oral tegafur (a fluoropyrimidine derivative) chemotherapy.Primary recurrence and liver metastases were identified 9 mo later.Obvious shrinkage of the patient’s recurrent and metastatic lesions was observed with continuous application of a hydrogen oxygen nebulizer,and a clinically objective response lasting for more than 4 mo was achieved.The patient remained disease-free at the time of writing this report.
CASE PRESENTATION
Chief complaints
We present the case of a 72-year-old female GBC patient,who was admitted to our hospital due to chest tightness in September 2018.
History of present illness
After examination,GBC was found to recurin situ,invading the duodenal descending part and causing intestinal fistula and hepatic colon adhesion.In addition,multiple metastases of the liver,lymph node metastasis around the head of the pancreas,severe anemia requiring weekly blood transfusion,and symptoms of heart failure were noted.
History of past illness
In December 2017,the 72-year old Chinese patient underwent IRE following diagnosis as GBC (T3N1M0 stage IIIA) based on computed tomography (CT) imaging and pathological findings of GBC (8.0 cm × 3.9 cm) with multiple hilar lymph node invasion (max 4.7 cm × 3.6 cm).She had elevated levels of a variety of serum tumor markers,including CA19-9 (2556 U/mL) and CEA (607.6 ng/mL).
Personal and family history
After IRE ablation of the gallbladder and hilar lymph nodes,oral tegafur (20 mg bid)chemotherapy was administered for 9 mo.CT re-examination in April 2018 showed liquefactive necrosis at the ablation site.During the treatment period,the patient received intermittent red blood cell (RBC) infusions as supportive care for repeated episodes of anemia.
Physical examination upon admission
Accompanied by a progressive increase in pain in the upper right abdomen,a large area of adhesion between the gallbladder and the descending and horizontal segments of the duodenum was found in addition to compression of the inferior vena cava (October 6,2018).
Laboratory examinations
She had elevated levels of a variety of serum tumor markers,including CA19-9 (88.18 U/mL),AFP (14.11 IU/mL),and CEA (39.68 ng/mL) in September,2018.
Imaging examinations
After 2 wk of blood transfusions and anti-infective treatment,CT examination again revealed a bladder tumor (6.3 cm × 4.9 cm),with an adjacent descending duodenal fistula,multiple spotted high-density lesions in the liver parenchyma,and dilatation and gas accumulation in the intrahepatic and extrahepatic bile ducts.Enlarged lymph nodes (2.7 cm × 2.1 cm) were visible around the pancreatic head.
FINAL DIAGNOSIS
Metastatic GBC,severe anemia,infection,and gallbladder-duodenal fistula.
TREATMENT
Hydrogen gas treatment
The hydrogen oxygen nebulizer (AMS-H-01,Asclepius Meditec,Shanghai,China)generates 3 L/min hydrogen gas by water electrolysis.As measured by gas chromatography,the gas generated consisted of 67% hydrogen and 33% oxygen.Using a special mask,the patient continued to inhale hydrogen for 3-6 h a day at rest,with no interruption even after the obvious relief of symptoms.
Best supportive care
Due to the long-term difficulty in reversing the anemia in the early stage of hydrogen inhalation therapy,the patient received weekly (1-2) blood infusions,and her RBC and hemoglobin levels were tested regularly.Daily anti-infection treatment was administered for the gallbladder-duodenal fistula,and white blood cell counts were measured regularly.After 1 mo of hydrogen aspiration therapy,the patient presented with intestinal obstruction,which was treated by gastrointestinal decompression and intravenous nutrition.Analgesics and sedatives were prescribed for pain and insomnia,respectively.
Therapeutic procedure
Due to the lack of currently available conventional treatments combined with the patient’s poor condition requiring continuous supportive care,hydrogen gas monotherapy was started on October 24,2018 (Table 1).At the time of writing this report,the patient still continues to receive daily hydrogen therapy.
Adverse events
According to the Common Terminology Criteria for Adverse Events version 3.0(National Cancer Institute,Bethesda,MD,United States),adverse events were classified and graded every week for at least 2 mo after the treatment was started[13].Liver function was evaluated based on the levels of alanine transaminase,aspartatetransaminase,total bilirubin,and gamma-glutamyl transpeptidase on multiple occasions during hydrogen treatment.Bone marrow hematopoietic function was evaluated based on peripheral blood erythrocyte counts and hemoglobin levels.Inflammation caused by infection was assessed based on white blood cell counts.

Table 1 Clinical details and therapeutic procedure
Curative evaluation
The curative effects of the treatment were evaluated according to several aspects of the patient’s general condition.Since patients cannot eat normally,serum total protein and albumin levels were monitored after intravenous nutrition.Due to visceral adhesion,intestinal fistula and obstruction,degrees of pain and relief in the upper abdomen were recorded continuously.Absolute lymphocyte counts and serum tumor markers were measured to reflect changes in immune function and tumor activity.
CT imaging changes
Changes in CT tumor imaging were monitored to evaluate the curative effect of hydrogen gas therapy.According to the RECIST 1.1 guidelines[14],therapeutic effects are categorized as a complete response (CR),characterized as disappearance of tumor detection in all target lesions; partial response (PR),total reduction in the diameter of the target lesions ≥ 30%; stable disease (SD),tumor regression failing to reach PR or progressive disease (PD); or PD,defined as total progression of the tumor diameter ≥20%.
OUTCOME AND FOLLOW-UP
Hydrogen gas inhalation was started on October 24,2018.Within 1 mo of treatment,the patient’s condition was relatively stable,and her blood indexes,infection status,and degree of pain gradually improved.Subsequently,intestinal obstruction occurred at the adhesion site between the gallbladder and duodenum; this was relieved after 1 mo of gastrointestinal decompression and intravenous nutrition.The patient insisted on regular hydrogen therapy throughout the course of this treatment.
Adverse events
The most common adverse reactions recorded included drowsiness or agitation,and no other adverse events were observed.The patient’s transaminase levels remained normal throughout the treatment.Occasionally her bilirubin levels exceeded the reference range,but returned to normal after short-term use of hepatoprotective drugs.Despite regular blood transfusions,there was little change in the patient’s red blood cell counts and hemoglobin levels during the two weeks before hydrogen treatment was initiated.Both indexes continued to increase after hydrogen therapy and blood transfusions,and both reached the lower limit of the reference range after 2.5 mo of treatment (Figure 1A).The frequency of transfusions was decreased gradually after hydrogen therapy and stopped completely after 2 mo of treatment.
Within 1 mo prior to treatment,the patient had a high inflammatory response to infection and a high white blood cell count (22.1 × 109/L).After anti-infection treatment,the white blood cell count was restored to the upper limit of the reference range (9.8 × 109/L),with no further reduction.After 1.5 mo of hydrogen treatment(with no further anti-infection treatment),the leukocyte count decreased to 4.7 ×109/L (Figure 1C left).
Curative evaluation
Serum total protein levels returned to normal shortly after the start of hydrogen therapy and continued to rise.Because of the intestinal obstruction,the patient received intravenous nutrition for 1-2 mo after treatment.Within 2 wk of the removal of the gastric tube,the patient returned to a normal diet and the total protein remained at the upper limit of the reference range.Serum albumin levels returned to normal after 2 mo of hydrogen therapy and continued to rise (Figure 1B).
Prior to hydrogen therapy,extensive adhesion and compression of gallbladder tumors caused severe pain in the upper abdomen that required daily pain medication;this was stopped when the pain gradually diminished after 2 wk of hydrogen treatment.Subsequent pain-induced administration of analgesics was not necessary,even during ileus.
T and NK cells are the major populations of lymphocytes that mediate anti-tumor immunity; therefore,the total number of lymphocytes is positively correlated with the immune function of patients.Before tumor recurrence and metastasis,the total number of lymphocytes continued to rise (1.2 × 109/L),indicating an increase in immune function.However,the total number of lymphocytes declined rapidly with tumor progression,to significantly below the reference range (0.8-4 × 109/L),reaching a minimum (0.7 × 109/L) during intestinal obstruction (1.5 mo after hydrogen therapy).The lymphocyte numbers then rebounded,reaching 1 × 109/L after 2.5 mo of hydrogen treatment (Figure 1C right).
Before the detection of tumor recurrence (September 20,2018),all three tumor markers were significantly higher than the reference range,but all showed a slight decline,which may be related to the compensation of immune function before treatment failure.After identification of tumor recurrence and metastasis,all three markers began to increase rapidly.This was consistent with the rapid growth of the tumor,which caused obstruction.After 1.5 mo of hydrogen therapy,the levels of all three markers began to decrease rapidly,falling into the reference ranges after 2.5 mo(Figure 2).
CT imaging changes
Before hydrogen gas treatment,the sum of the tumor diameters was 12.2 cm; 1 mo after treatment,the sum was 13.1 cm (37% increase,PD); and 2.5 mo after treatment,the sum was 7.5 cm (6% increase,SD) (Figure 3 and Table 2).At the end of February 2019,no tumor recurrence was detected (very similar to the CT examination at 2.5 mo;images not shown).To date,the patient appears completely well (Karnofsky score 100) and has resumed a normal diet and exercise.
DISCUSSION
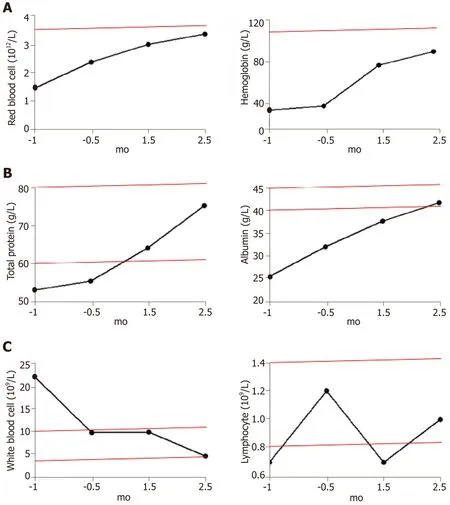
Figure 1 Blood parameters of patients before and after hydrogen treatment.
In GBC patients who are not candidates for surgery,the NCCN guidelines recommend the use of chemotherapy and best supportive care.Due to the large size of tumor in this patient (stage IIIA),the gallbladder function was completely lost with widespread adhesions to the hilum of the liver.Therefore,it was necessary to choose an ablation method that causes minimal damage to the extrahepatic bile duct system in reducing the tumor size.IRE is a novel ablation technology that utilizes short pulses of high voltage electrical energy to induce tissue necrosis.This technique has many advantages,including short ablation time,preservation of the internal structure of vital organs,and lack of the heat/cold-sink effect[15].We have previously verified the safety and efficacy of gallbladder ablation in a rabbit model[16].Although not yet included in the NCCN guidelines,IRE has the potential to be a superior alternative to other ablation techniques for the removal of tumors situated near the gallbladder[17-19].
IRE,combined with oral chemotherapy,effectively controlled the tumors in the gallbladder and the hilar part of the liver,and re-examination after 3 mo of treatment showed that the tumor was basically necrotic.However,for this patient with advanced GBC,palliative treatment could only delay the disease,with continued slow progression of the tumor.In the re-examination after 9 mo of treatment,recurrence of the gallbladder tumor,duodenum fistula,liver metastases,and lymph node metastases around the head of pancreas as well as severe anemia were detected,which indicated that the disease had entered a stage of rapid and life-threatening progression in a short period of time.Best supportive care was the only option at this timepoint,although in general,it is not possible to reverse the progression of such tumors.
Molecular hydrogen,or H2,can selectively neutralize hydroxyl radicals,but not other reactive oxygen species (ROS)[20].Hydrogen has been used to treat various states associated with oxidative stress,including trauma[21],neurodegenerative disease[22],inflammatory disease[23],metabolic syndrome[24],adverse reactions to chemotherapy[25],and radiation injury[26].In addition to the apparent improvement in the immune system[12],there is much evidence that hydrogen directly kills different types of tumors,including cutaneous squamous cell carcinoma[27],leukemia[28],tongue cancer[29,30],and colon cancer[8].Since there has been no report on the upper limit of hydrogen use,this therapy might be a very safe method.

Figure 2 Changes in tumor markers before and after hydrogen treatment.
At the same time as the delivery of optimal supportive care,the patient was enrolled in this clinical study (24 October 2018) with the intention of improving clinical symptoms.One month after the start of hydrogen therapy,the disease continued to progress,and the levels of tumor markers (including CA19-9,AFP,and CEA) continued to rise,although the patient’s general status and blood indexes(including total protein,albumin,multiple blood cells count,hemoglobin content,etc.)showed continuous improvement,so the patient persisted with the hydrogen treatment.Gradually,the levels of multiple tumor markers began to decline,and multiple hematological indicators continued to improve.The patient underwent gastric tube removal on December 24,and gradually began eating semi-liquid food,with significant improvement in spirit,appetite,and sleep.Subsequent CT examination also confirmed relief of the obstruction,with significant shrinkage of tumors at multiple sites.The reason for the patient’s extraordinary recovery,apart from symptomatic treatment,is probably because the persistence of hydrogen therapy; this therapy not only mediates rapid improvement in the physical condition of the patient,but also significantly reduces tumor marker levels,increases lymphocyte counts,and even induces tumor shrinkage.
At present,there is only a temporal connection between hydrogen and improvement of this patient’s cancer.The proposed mechanism underlying the anticancer properties of hydrogen may involve:(1) Elimination of the high levels of ROS produced by cancer cells,thus inhibiting the proliferation,invasion,and migration of cancer cells[31]; (2) Downregulation of inflammatory factors,elimination of chronic inflammation,and modification of the microenvironment[32]; (3) Protection of mitochondria,which maintains energy generation and help correct hypoxia,thereby transforming the cardiovascular,endocrine,and nervous systems[11]; and (4)Restoration of the function of exhausted cytotoxic T cells,and enhancement of systemic anti-cancer effects[33].The detailed mechanism remains to be fully elucidated in further follow-up studies,and indications for advanced cancer therapy require verification in studies with greater numbers of patients.

Table 2 Tumor sizes before and after hydrogen gas treatment
CONCLUSION
This is the first report on the rehabilitation of an advanced GBC patient with a critical general condition,whose disease has gradually improved and has survived for more than 4 mo.

Figure 3 Computed tomography imaging findings at different time points before and after hydrogen treatment.
杂志排行
World Journal of Clinical Cases的其它文章
- Bone alterations in inflammatory bowel diseases
- Extrahepatic hepcidin production: The intriguing outcomes of recent years
- Neoadjuvant endocrine therapy: A potential strategy for ER-positive breast cancer
- Vestigial like family member 3 is a novel prognostic biomarker for gastric cancer
- HER2 heterogeneity is a poor prognosticator for HER2-positive gastric cancer
- Changes in corneal endothelial cell density in patients with primary open-angle glaucoma
