ALK-positive anaplastic large cell lymphoma presenting multiple lymphomatous polyposis: A case report and literature review
2019-08-14MakotoSaitoKohIzumiyamaReikiOgasawaraAkioMoriTakeshiKondoMasanoriTanakaMasanobuMoriokaKenchoMiyashitaMishieTanino
Makoto Saito,Koh Izumiyama,Reiki Ogasawara,Akio Mori,Takeshi Kondo,Masanori Tanaka,Masanobu Morioka,Kencho Miyashita,Mishie Tanino
Abstract
Key words: Anaplastic large-cell lymphoma; Anaplastic lymphoma kinase; Multiple lymphomatous polyposis; T-cell lymphoma; Gastrointestinal involvement
INTRODUCTION
Anaplastic large cell lymphoma (ALCL) was first described in 1985 by Steinet al[1].According to the 4thedition (2008) of the WHO classification[2],primary systemic ALCL can be divided into two distinct categories:anaplastic lymphoma kinasepositive (ALK+) and ALK-negative.Majority of ALK+ ALCL contain a t(2;5)chromosomal translocation.The t(2;5) translocation fuses a distal part of theALKgene on chromosome 2p23 with the promoter and a proximal domain of the nucleophosmin (NPM1) gene on chromosome 5q35[3].The most common extranodal sites of ALK+ ALCL are the skin,bone and soft tissue.ALK+ ALCL cases involving the gut are rare[2].
Multiple lymphomatous polyposis (MLP) is thought to be a representative form of gastrointestinal lesion in mantle cell lymphoma (MCL)[2,4,5].Here,we report an extremely rare case of ALK+ ALCL with gastroduodenal involvement presenting as MLP.
CASE PRESENTATION
Chief complaints
A 43-year-old Japanese man suffering from fever,night sweats,general fatigue and weight loss complained of a mass in the left inguinal area.The patient did not complain of gastrointestinal symptoms.
History of present illness
The patient was admitted to a local hospital.Computed tomography (CT) scan demonstrated multiple lymph node lesions continuing to the mesentery and paraaortic/left common iliac artery/left inguinal region (Figure 1).Scattered nodular lesions were found in both lung fields (Figure 1).Following needle biopsy of the left inguinal lesion,malignant lymphoma was suspected,and the patient was transferred to our department.
History of past illness
He had no chronic illness.
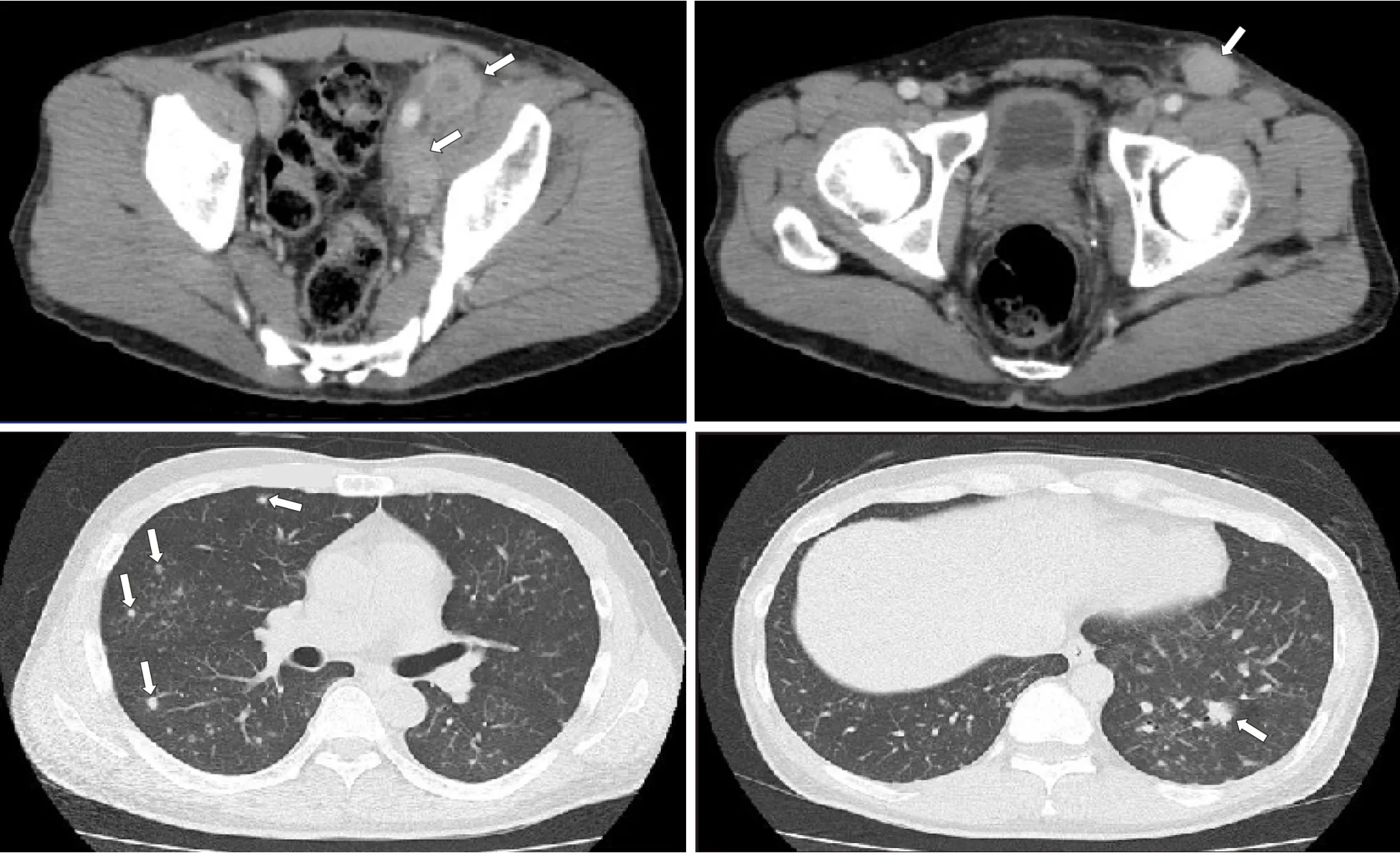
Figure 1 Computed tomography images.
Physical examination upon admission
Left inguinal lymph nodes were significantly swollen.
Laboratory examinations
WBC and CRP showed markedly high values,and elevated platelet count,liver dysfunction,and hypoalbuminemia were also observed.In addition,the level of soluble interleukin-2 receptor (normal range:121-613 U/mL),which was severely elevated according to the measurement of the previous hospital,had further increased over approximately one week (7120 → 12500 U/mL) (Table 1).
Imaging examinations
As measured by positron emission tomography (PET)/CT scan,the mean standardized uptake value was 18.1 in the abdomen - pelvis/inguinal nodes and 3.5 in the lung fields and the mediastinal nodes (Figure 2).
Esophagogastroduodenoscopy findings:In the descending portion of the duodenum,multiple polypoid lesions of 2-3 mm in diameter were observed (Figure 3A).Various large and small polypoid lesions were observed in the antrum of the stomach (Figure 3B and Figure 3C).These lesions are consistent with MLP continuously extending from the antrum of the stomach to the descending portion of the duodenum.Mucosal folds in the corpus of the stomach were slightly thickened,and its surface had changed to a white tone (Figure 3D).
The biopsies of both gastric and duodenal lesions proved the invasion of lymphoma cells,as below mentioned.These lesions could not be detected by PET/CT scan.Colonoscopy and bone marrow aspiration showed no involvement of lymphoma lesions.
Pathological examinations
Left inguinal lymph nodes were examined by open biopsy.Medium to large-sized abnormal lymphoid cells were observed to be invasively proliferating.CD25,CD30,T-cell intracellular antigen-1,and ALK tested positive by immunostaining.Meanwhile,CD3,CD20 and the Epstein-Barr encoding regionin situhybridization tested negative.Based on the histopathology,ALK+ ALCL was diagnosed.In the gastric and duodenal biopsy samples,abnormal lymphoid cells with irregular nuclei grew diffusely (Figure 4A),and mitotic figures were observed in high numbers(Figure 4B).Immunohistochemically,CD30 tested strongly positive (Figure 4C),ALK(monoclonal antibody,ALK1) tested positive in nuclear and cytoplasmic pattern(Figure 4D),and the Ki-67 proliferative (MIB1) index was > 80% (not shown).

Table 1 Results of laboratory examinations on admission
FINAL DIAGNOSIS
ALK+ ALCL that involved multiple lymph node lesions in the abdomen -pelvis/inguinal region and mediastinum,also both lung fields and the gastroduodenal lesions (Stage IV).
TREATMENT
We treated this patient with six cycles of CHOEP chemotherapy (Cyclophosphamide 750 mg/m2,Doxorubicin 50 mg/m2,Vincristine 1.4 mg/m2,Etoposide 100 mg/m2x 3 d,and Prednisone 50 mg/m2x 5 d) every three weeks.After administration of two cycles,the lymphoma lesions including lung field nodules shrank remarkably and disappeared at CT examination.
OUTCOME AND FOLLOW-UP
At the conclusion of treatment,there was complete remission.Numerous white scars were found in the stomach,endoscopically consistent with a remission image of lymphoma (Figure 3E).He is followed-up as outpatient with no treatment.There was no evidence of recurrence for more than 1 year and 10 mo since the end of the final treatment.
DISCUSSION
ALCL is a clinically,morphologically,and immunophenotypically heterogeneous Tcell lymphoma.Depending on the presence or absence of ALK expression,ALK+ALCL was classified as a biologically homogeneous disease unit independent of ALKnegative ALCL in the 4th edition (2008) of the WHO classification[2].ALK+ ALCL is more prevalent in children and young adults,and the ALK fusion protein is associated with a good prognosis[6].In contrast,ALK-negative ALCL has a poor prognosis similar to peripheral T-cell lymphoma,not otherwise specified,and angioimmunoblastic T-cell lymphoma[7].ALK staining pattern is nuclear and cytoplasmic in cases of t(2;5)/NPM-ALK translocation,and membranous or diffuse/granular cytoplasmic in the remaining cases with a variant translocation involving at 2p23[2,8].ALK staining in our patient showed a nuclear and cytoplasmic pattern.G-banded karyotype of the lymph node lesions showed complex chromosomal abnormalities with +2,der(2;21)(q10;q10),+7,however,translocation at 2p23 could not be confirmed.ALK+ ALCL frequently involves both lymph nodes and extranodal sites.The most commonly involved extranodal sites include the skin,bone,soft tissue,liver and lungs as we reported here[2].

Figure 2 Positron emission tomography/computed tomography (longitudinal) image.
Because gastrointestinal T-cell lymphomas are rare,little is known about the clinicopathological characteristics of primary gastrointestinal T-cell lymphomas.Kimet al[9]investigated the endoscopic differences between B- and T-cell lymphomas and observed that B-cell lymphomas presented more often as fungating (54% of cases),while T-cell lymphomas were frequently ulcerative (47%),and only 13% showing a fungating pattern.Regardless of ALK expression,primary gastrointestinal ALCL is rarer[10].According to a recent review on gastrointestinal ALCL,the rate of ALK expression among gastrointestinal ALCL was low at 24%[11].As far as we can determine,ALK+ ALCL of the gut has been reported in only eleven cases[11-20].The clinical features are summarized in Table 2 for a total of 12 gastrointestinal ALK+ALCL cases,including our patient.Of these,four cases were reported to involve the esophagus[12-15],all showing fungating tumors.Of the remaining cases,two involved the stomach[11,16],one involved the duodenum[17],one involved both the stomach and duodenum[18],and three involved the small intestine (jejunum/ileum)[11,19,20].Only three of these last seven cases showed macroscopic findings by resection or endoscopy; the morphology showed a mass formation pattern,such as a submucosal or bulky tumor.Although the number of cases is very small,gastrointestinal ALK+ALCL often seems to involve the esophagus,in which lymphomas rarely develop,and frequently exhibits a fungating growth pattern similar to that of B-cell lymphomas.
The term ‘‘MLP’’ was introduced in 1961 by Cornes to describe malignant lymphoma that presented as multiple polypoid tumors,from 2 mm to several centimeters,affecting long segments of the gastrointestinal tract[21].Histopathologically,these polyps originate from the mantle zone of the lymphoid follicle of the mucosa-associated lymphoid tissue (MALT)[22].Therefore,the most frequent lymphoma presenting with MLP is MCL[4,5],and it also develops in other Bcell lymphomas,such as MALT lymphoma and follicular lymphoma[23].Furthermore,T-cell lymphomas seldom show this feature (11%)[24].Several cases of adult T-cell leukemia/lymphoma presenting with MLP have been reported in Japan,which is an endemic area of human T-cell lymphotropic virus type 1 infection[25,26].To the best of our knowledge,including ALK-negative,our case is the first observation of ALCL presenting with MLP.However,in contrast to what has been seen in MCL,the MLP presented in this case with,irregular sized-polyps arranged irregularly.In addition,no MLP lesion was found in the large intestine,which is frequently involved in MCL[27].In our case,MLP lesions could not be detected with PET/CT scans.As we previously reported in a case of MCL[28],it appears that MLP lesions do not infiltrate the deep layer and instead maintain involvement with the surface layer of the gastrointestinal mucosa,even in the case of ALCL.The characteristic endoscopic findings of MCL are not only MLP,but also thickening of gastric mucosal folds has been reported[5].In our case,thickened folds of the stomach were also seen,and the endoscopic features were thought to be similar to those of MCL.
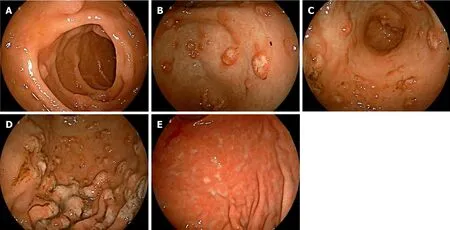
Figure 3 Esophagogastroduodenoscopy findings.
CONCLUSION
We reported a case of gastroduodenal ALK+ ALCL presenting with MLP.Although there is a limit in considering the macroscopic/endoscopic features of gastrointestinal ALK+ ALCL patients through this very rare case,the morphological features of gastrointestinal ALK+ ALCL may be similar to those of B-cell lymphomas rather than T-cell lymphomas.It is necessary to further accumulate and study the gastrointestinal ALK+ ALCL patients.

Table 2 Clinical features of gastrointestinal anaplastic lymphoma kinase-positive anaplastic large cell lymphoma
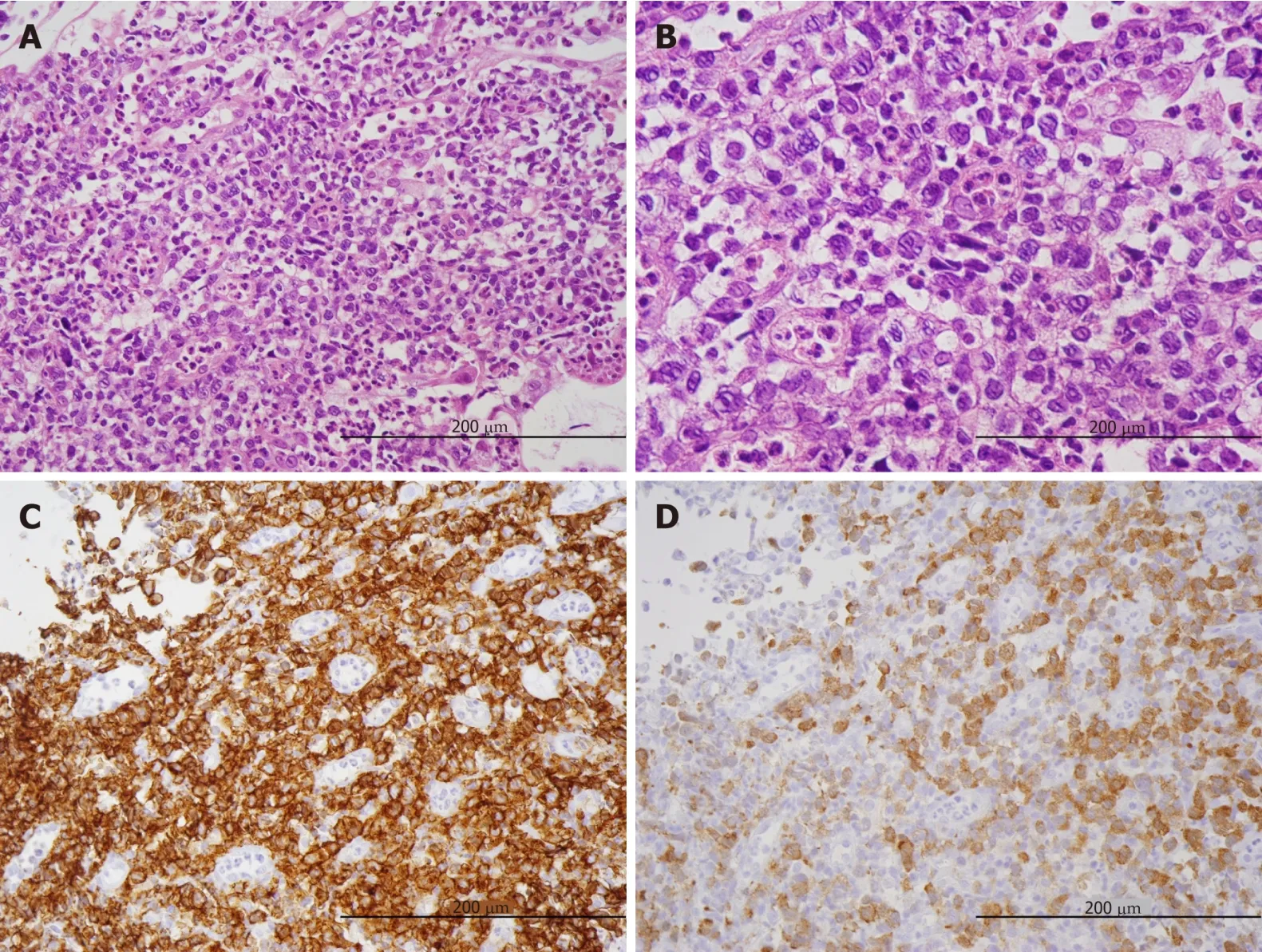
Figure 4 Histopathological findings in biopsy samples (x 200),Medium to large-sized abnormal lymphoid cells with irregular nuclei grew diffusely (A),and mitotic figures were observed in high numbers (B).
杂志排行
World Journal of Clinical Cases的其它文章
- Bone alterations in inflammatory bowel diseases
- Extrahepatic hepcidin production: The intriguing outcomes of recent years
- Neoadjuvant endocrine therapy: A potential strategy for ER-positive breast cancer
- Vestigial like family member 3 is a novel prognostic biomarker for gastric cancer
- HER2 heterogeneity is a poor prognosticator for HER2-positive gastric cancer
- Changes in corneal endothelial cell density in patients with primary open-angle glaucoma
