Feasibility and safety of robotic PCI in China: first in man experience in Asia
2019-06-12KeFeiDOUChenXiSONGChaoWeiMUWeiXianYANGChengGangZHULeiFENGJueCHENLeiSONGYuNINGBoXU
Ke-Fei DOU*, Chen-Xi SONG*, Chao-Wei MU, Wei-Xian YANG, Cheng-Gang ZHU, Lei FENG, Jue CHEN, Lei SONG, Yu NING, Bo XU
Feasibility and safety of robotic PCI in China: first in man experience in Asia
Ke-Fei DOU*, Chen-Xi SONG*, Chao-Wei MU, Wei-Xian YANG, Cheng-Gang ZHU, Lei FENG, Jue CHEN, Lei SONG, Yu NING, Bo XU#
State Key Laboratory of Cardiovascular Disease, Department of Cardiology, Cardiovascular Institute, Fuwai Hospital and National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing, China
To evaluate the feasibility and safety of a second generation robotic percutaneous coronary intervention (R-PCI) system in China.Robotic PCI has been shown to be an effective method for conducting coronary interventions. It has further benefits of more accurate lesion measurement, improved stent deployment, reduced incidence of geographic miss and reduction of operator radiation exposure.This single center evaluation enrolled 10 consecutive patients who had been selected for PCI. Clinical success was defined as residual stenosis < 30% and no in-hospital major adverse cardiovascular events. Learning curve effect was assessed by comparing efficiency metrics of early. later cases.Eleven lesions were treated all successfully without manual interruption or MACE events. Most lesions (63%) were ACC/AHA class B2 and C. Mean procedure time was 57.7 ± 26.4 min, however two procedures were part of live demonstrations. Excluding the two live cases, the mean procedure time was 51.8 ± 23.7 min. Procedural efficiency tended to improve from early cases to later cases based on PCI time (48.3 ± 32.925.5 ± 13.0 min,0.27), fluoroscopy time (20.3 ± 8.212.5 ± 4.6 min,0.16), contrast volume (145.0 ± 28.9102.5 ± 17.1 mL,0.05) and Air Kerma dose (1932 ± 9781007 ± 70 mGy,0.31).Second generation robotic PCI was safe, effective and there were trends toward improvements in procedural efficiency during this early experience in China.
2019; 16: 401405. doi:10.11909/j.issn.1671-5411.2019.05.004
Angioplasty; Percutaneous coronary intervention; Robotic assist
1 Introduction
The use of robotics for performing coronary and peripheral vascular procedures has been shown to be safe and effective and their use is becoming more widespread.[1–3]Reported benefits of robotic percutaneous coronary intervention (R-PCI) over standard manual PCI (M-PCI) procedures include improved lesion measurement,[4]more accurate stent placement reducing geographic miss,[5]and reduction in radiation exposure for operating physicians.[1]The previously published data on R-PCI were based on experiences with the first generation CorPath 200 (Corindus Vascular Robotics, Waltham, MA) System. As with any new technology, there are incremental improvements based on collective experience and user feedback. This led to the de-velopment of a second-generation device, GRX, which incorporates a 3rdjoystick for active control of the guide catheter; modifying the robotic arm to provide additional reach for access, e.g., left radial; and an improved monitor to provide better resolution. We provide the first report of the clinical use of the GRX system and R-PCI in Asia. The objectives of the present study are to evaluate the feasibility and safety of R-PCI, and describe the early learning curve.
2 Methods
This study was conducted as a single-center first in human evaluation of a second generation R-PCI system, the CorPath GRX System (Corindus Vascular Robotics, Waltham, MA) in patients undergoing PCI. The study was approved by Institutional Review Board Central Committee at Fuwai Hospital and all patients were provided written informed consent prior to PCI procedure.
2.1 Patients
There were no formal inclusion/exclusion criteria for study participation. We enrolled ten patients who were scheduled to undergo PCI procedures.
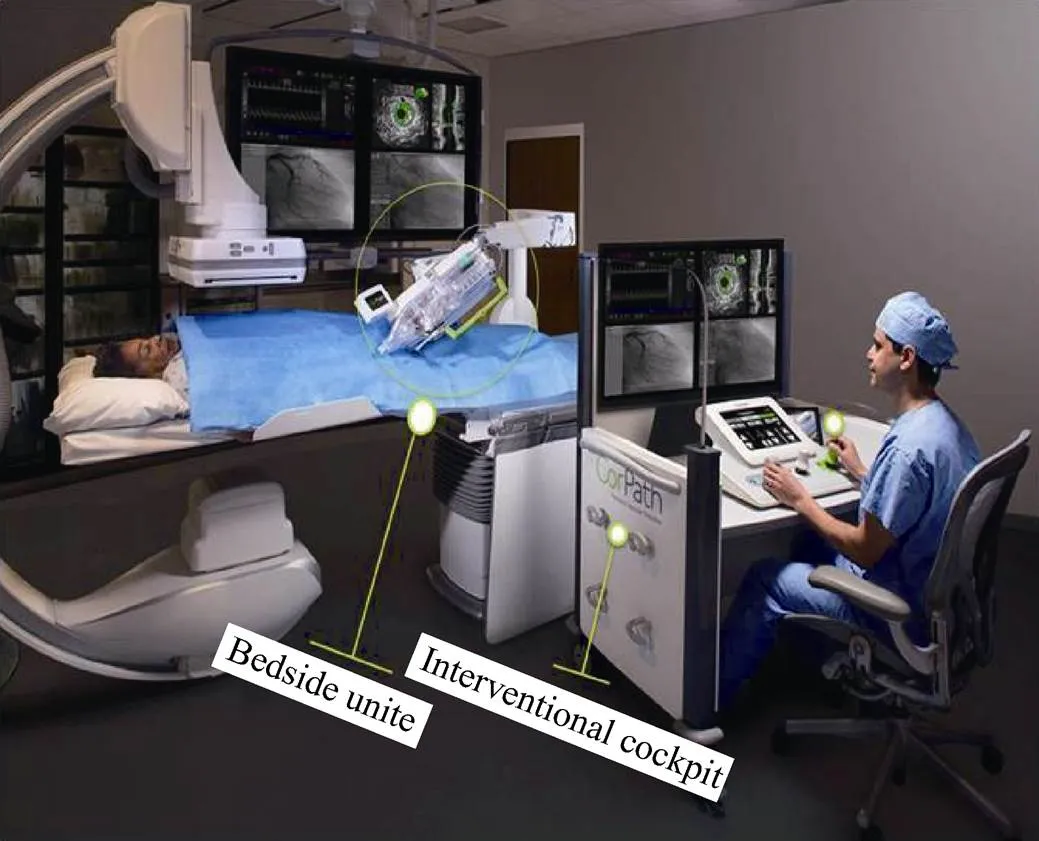
Figure 1. CorPath GRX robotic system components.
2.2 Procedures
Robotic PCI was conducted by two operators using the CorPath GRX System from March 15, 2017 to April 26, 2017 (Figure 1). All devices used in conjunction with R-PCI were commercially available devices and were used per physician preference. The general features of R-PCI have been previously described in detail.[1]Briefly, the GRX System consists of a bedrail mounted robotic drive and sterile cassette. The cassette can be loaded with commercially available PCI devices including 0.014” guidewires, rapid exchange balloons and stent delivery systems. Operators conduct the procedure from a seated position in radiation- shielded interventional cockpit. Within the cockpit is the console consisting of three joysticks and a touchscreen (Figure 2), which are used to manipulate the intravascular devices as well as video displays for monitoring fluoroscopy, electrocardiography, and hemodynamics. Operator manipulations to the joysticks and touchscreen are translated to the sterile cassette via a communication cable to control the guidewire and rapid exchange catheters (Figure 3).
2.3 Data collected and statistical analysis
Data collected included patient demographic and medical history, lesion characteristics, procedure characteristics and clinical success. Description of lesion characteristics included percent stenosis assessed visually; grading severity using the American College of Cardiology/American Heart Association (ACC/AHA) lesion classification.[6]Procedure characteristics included reporting of radiation exposure by use of a bedside monitor. Clinical success was defined as residual stenosis < 30% and no in-hospital major adverse cardiovascular events (MACE). Data presented as descriptive statistics (frequency and percentage for categorical variables and number of observations, mean, and standard deviation for continuous variables) were used to present results. We further evaluated whether there was a learning curve effect by evaluating the procedural efficiency of earlylater cases. For this evaluation we used unpaired- and chi-squared tests for continuous and categorical variables, respectively.
3 Results
Table 1 summarizes patient and lesion characteristics. Ten consecutive patients with 11 lesions were enrolled. The patients were primarily males, 9/10 (90%) and the mean age was 66.6 ± 5.7 years. The treated lesions included 6/11 (54.5%) in the left coronary artery and 5/11 (45.5%) in the right coronary artery. The majority (7/11; 63.6%) of the treated lesions were graded class B2 and C by the ACC/AHA classification system.
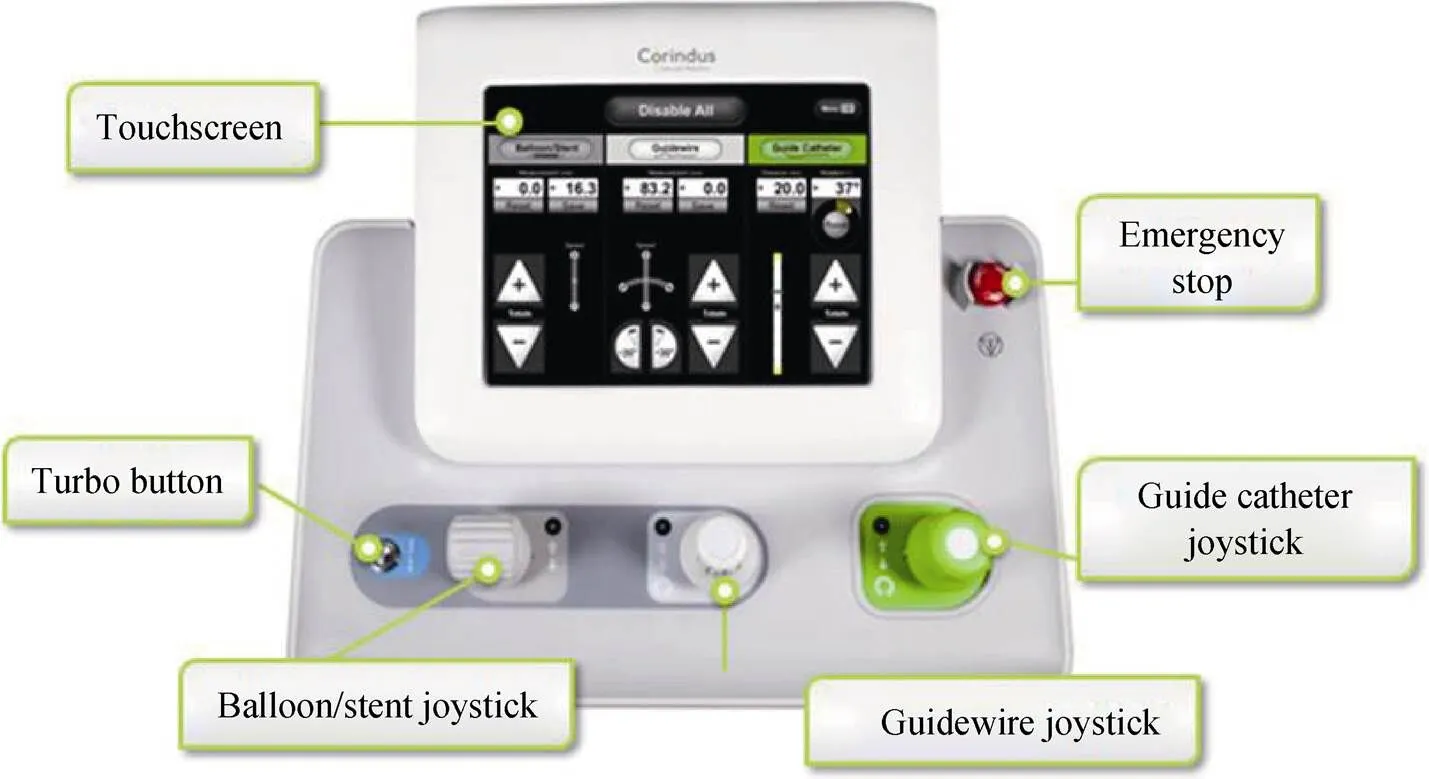
Figure 2. Control console components.
Figure 3. Extended reach and robotic drive.
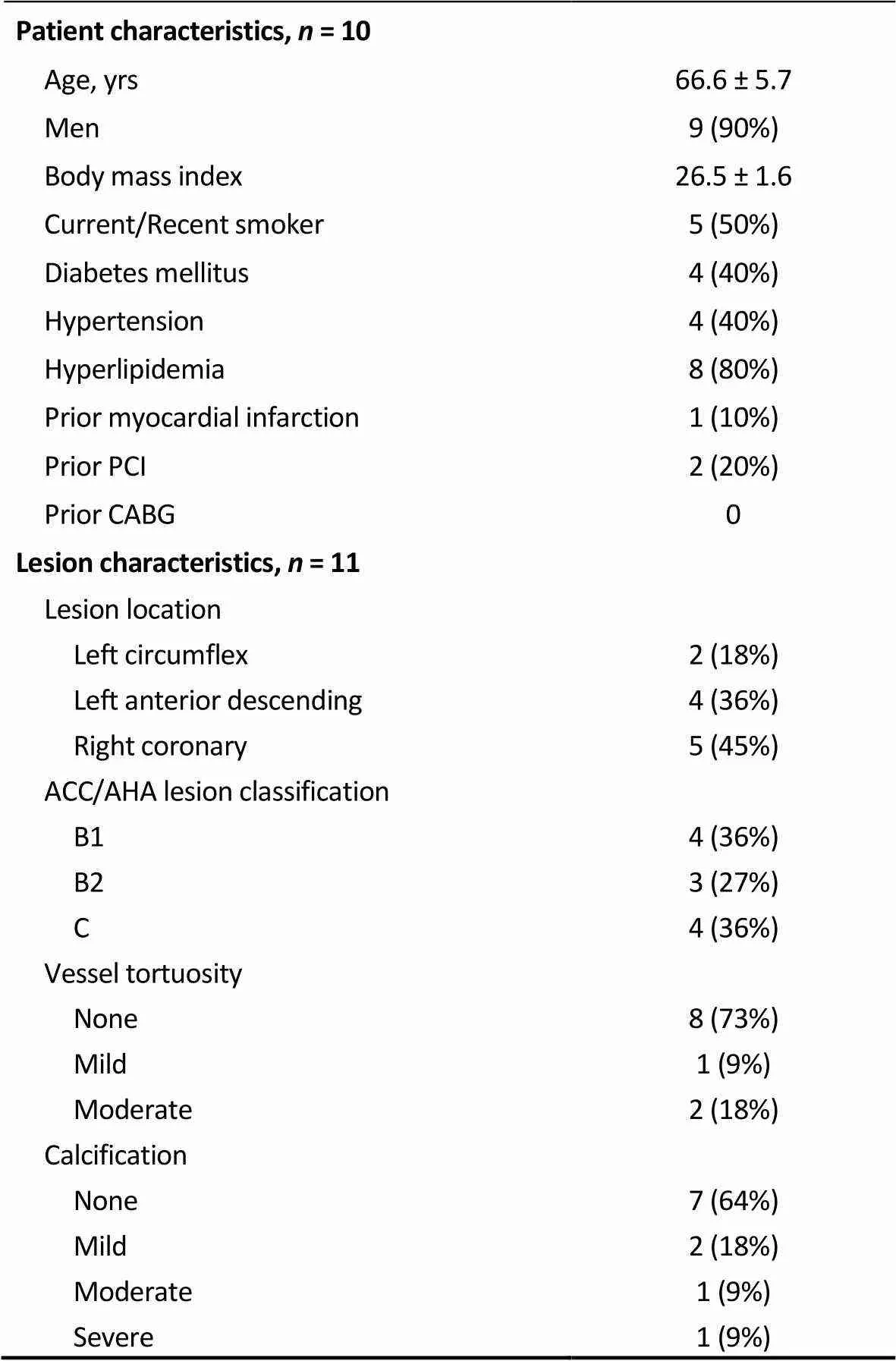
Table 1. Patient and lesion characteristics.
Results expressed as(%) or mean ± SD. CABG: coronary artery bypass grafting; PCI: percutaneous coronary intervention.
Procedural characteristics are described in Table 2. All procedures were performed via right radial artery access. The mean pre- and post-procedure percent stenosis were 84.5% ± 5.7% and 1.8% ± 6.0%, respectively. There were no MACE events, and all cases achieved the criteria for clinical success without conversion to manual operation. The mean PCI and fluoroscopy times were 44.3 ± 29.7 and 18.2 ± 8.0 min, respectively. Two cases (numbers 5 and 10) were conducted as part of live demonstrations at international conferences where delays were incurred due to conference scheduling. Excluding the live demonstration cases, the mean PCI time was 36.9 ± 26.1 min.

Table 2. Procedure characteristics.
All patients (= 10), excluding live cases (= 8). Results expressed as mean ± SD unless other indicated.
Learning curve effect analysis of early (patients 1–4)later (patients 6–9) cases, excluding the live cases, is summarized in Table 3. Procedural efficiency measures including PCI time (48.3 ± 32.925.5 ± 13.0 min;0.27 should be same as the data in Table 3), fluoroscopy time (20.3 ± 8.212.5 ± 4.6 min;0.16), contrast volume (145.0 ± 28.9102.5 ± 17.1 mL;0.05) and radiation exposure (1932 ± 9781007 ± 70 mGy*cm2;0.31) were numerically lower in the later compared to earlier cases.
There were no safety issues associated with device use and no patients experienced in-hospital major cardiac adverse events.
4 Discussion
The current study reports the first use of the next generation device, the CorPath GRX System in Asia and demonstrates safety and efficacy of this system.

Table 3. Lesion and procedure characteristics: early vs. late cases.
Early cases = case numbers 1–4; late cases = case numbers 6–9 (excludes live cases). Results expressed as mean ± SD or. PCI: percutaneous coronary intervention.
Previous studies have demonstrated the feasibility and safety of first-generation robotic system to treat complex coronary artery disease.[7]However, approximately 1 in 5 patients with complex coronary artery disease required manual conversion or partial manual assistance, and the predominant reason for this was due to inadequate robotic guide-catheter control. To decrease the rate of manual assistance or manual conversion, several improvements have been made, resulting in the second-generation robotic system. Compared with the first-generation CorPath 200 system, CorPath GRX added a third joystick for robotic manipulation of the guide catheter, and guide-catheter disengagement can be corrected robotically. In addition, CorPath GRX system has active rather than passive guide-catheter control, which further provides support for device manipulation. The cassette arm has also been improved to provide additional reach for arterial access. Taken together, all these improvements are made with the intension to further eliminate conversions to M-PCI.
To our knowledge, the use of CorPath GRX System in Asia has not been reported and this is the first in-human report of second-generation robotic system in Asia. Although small, in this early series we made three key observations. First, all ten cases, which were performed consecutively and included 11 lesions were performed successfully without MACE or manual assistance, which confirms that implementation of a robotic program can be accomplished in a safe and uniform manner by physicians experienced in manual PCI procedures. Our results are consistent with those of Smitson,,[8]who reported their experience on 40 patients in the United States treated with the same device and demonstrated the safety and efficiency of CorPath GRX System.Further, the manufacturer provided a detailed training program in the device use including a didactic review of the operator’s manual, hands-on use of the system with a model, and a post-training quiz to demonstrate proficiency. Therefore, prior to our first patient use, we were well-versed in the feature and capabilities of the robotic system. Still, there were learning curve issues, as trends toward improved procedural efficiency were demonstrated with continued use of the device.
Of note, in our experience, there were no conversions to M-PCI in our patient cohort. Conversion to manual procedures can be of particular concern because of increased procedure time leading to increased exposure to radiation and contrast. In a recent report of the previous generation device, CorPath 200, 20/108 (18.5%) procedures required planned or unplanned manual assistance or conversion to manual procedures.[8]We propose the improvements in second-generation system contribute to the reduced conversions to M-PCI.
Other than learning curve issues associated with the use of a new technology, we used the R-PCI system in the same manner that we would perform M-PCI. This includes the preferential use of radial access for all cases and the use of common guidewires, catheters and stent delivery systems. The mean overall procedure time of 57.7 ± 26.4 min, would be considered high when compared to contemporary M-PCI, but these results were inflated by two cases presented as part of international meetings. The range of procedure times for the other eight cases was 18-96 min, with the first case requiring 96 min. All other cases required 42 min or less, which is in line with procedure time reported for experienced users of the R-PCI system which was reported at 42.2 ± 16.4 min.[9]Further, although not statistically significant, there was a trend toward reduction of both procedure time, fluoroscopy time and radiation exposure with the continued use of the device indicating a learning curve toward increased comfort with its use. Our experience is similar to the reported learning curve experience in the PRECISE trial where there was a significant reduction in both procedure time and fluoroscopy time from the first three cases to the later cases.[10]
Additionally, we showed a near significant 42 mL reduction in the use of contrast volume in the later cases when compared to the early cases. Although widely used, contrast agent is not benign and can lead to the development of an iatrogenic complication, contrast-induced acute kidney injury (CI-AKI). The occurrence of CI-AKI is associated with increased patient morbidity, mortality, and health care costs.[11]Patients with pre-existing co-morbidities including renal disease, heart failure, diabetes, and > 75 years have been shown to be particularly susceptible to developing CI- AKI.[12]The only modifiable risk factor for reducing the incidence of CI-AKI is the utilization of decreased volumes of contrast.[12,13]If this trend toward reduced contrast volume use can be verified in a larger population, it could have significant impacts on patient outcomes.
4.1 Limitations
This study was a single center evaluation of a small number of patients. Although the only inclusion criterion for the study was that patients were scheduled to undergo PCI procedures, the small sample size limits the generalizability of the results. In addition, although there were no conversions to manual in our cohort, a larger sample will be required to ascertain as to whether the use of the GRX system improves this outcome when compared to the earlier device. Finally, although our results showed the first four cases were treated successfully and safe with the new robotic system, it should be noted that more cases are required in future study to further demonstrate the new system can be learned by most interventional cardiologists.
4.2 Conclusion
The first use of the second generation robotic PCI was safe and effective as all lesions were successfully treated with no conversion to manual operations. We show trends toward improvements in procedural efficiency during this early experience in China.
1 Weisz G, Metzger DC, Caputo RP,. Safety and feasibility of robotic percutaneous coronary intervention.2013; 61: 1596–1600.
2 Smilowitz NR, Moses JW, Sosa FA,. Robotic-enhanced PCI compared to the traditional manual approach.2014; 26: 318–321.
3 Mahmud E, Schmid F, Kalmar P,. Feasibility and Safety of Robotic Peripheral Vascular Interventions: Results of the RAPID Trial.2016; 9: 2058–2064.
4 Campbell PT, Kruse KR, Kroll CR,. The impact of precise robotic lesion length measurement on stent length selection: ramifications for stent savings.2015; 16: 348–350.
5 Bezerra HG, Mehanna E, Vetrovec GW,. Longitudinal Geographic Miss ( LGM ) in Robotic Assisted Versus Manual Percutaneous Coronary Interventions.2015; 28: 449–455.
6 Ellis SG, Vandormael MG, Cowley MJ,. Coronary morphologic and clinical determinants of procedural outcome with angioplasty for multivessel coronary disease. Implications for patient selection. Multivessel Angioplasty Prognosis Study Group.1990; 82: 1193–1202.
7 Mahmud E, Naghi J, Ang L,. Demonstration of the safety and feasibility of robotically assisted percutaneous coronary intervention in complex coronary lesions: results of the CORA- PCI study (Complex Robotically Assisted Percutaneous Coronary Intervention).2017; 10: 1320–1327.
8 Smitson CC, Ang L, Pourdjabbar A,. Safety and feasibility of a novel, second-generation robotic-assisted system for percutaneous coronary intervention: first-in-human report.2018; 30: 152–156.
9 Harrison J, Ang L, Naghi J,. Robotically-assisted percutaneous coronary intervention: Reasons for partial manual assistance or manual conversion.2018; 19: 526–531.
10 Weisz G, Smilowitz NR, Metzger DC,. The association between experience and proficiency with robotic-enhanced coronary intervention—insights from the PRECISE multi- center study.2014; 16: 37–40.
11 McCullough PA, Choi JP, Feghali GA,. Contrast-induced acute kidney injury.2016; 68: 1465–1473.
12 Mehran R, Aymong ED, Nikolsky E,. A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: Development and initial validation.2004; 44: 1393–1399.
13 Gurm H, Seth M, Mehran R,. Impact of contrast dose reduction on incidence of acute kidney injury (AKI) among patients undergoing PCI: a modeling study.2016; 28: 142–146.
Correspondence to: Bo XU, MBBS, Department of Cardiology, Fuwai Hospital, 167 Beilishi Road, Beijing 100037, China. E-mail: bxu@citmd.com
January 14, 2019
February 25, 2019
March 10, 2019
May 28, 2019
*The first two authors contributed equally to the article.
杂志排行
Journal of Geriatric Cardiology的其它文章
- Clinical significance of diabetes on symptom and patient delay among patients with acute myocardial infarction—an analysis from China Acute Myocardial Infarction (CAMI) registry
- Protective effect of Danhong injection in patients with acute myocardial infarction at a high risk of no-reflow during primary percutaneous coronary intervention
- Heart failure with preserved ejection fraction in the elderly: pathophysiology, diagnostic and therapeutic approach
- The Harvard method of Tau calculation is incorrect
- Conduction disorder and primary cardiac tumor: a fatal case of multiple lipomas of the right atrium
- Cryoballoon ablation on an elder paroxysmal atrial fibrillation patient implanted with double chamber pacemaker: a case report
