Termination of a partial hydatidiform mole and coexisting fetus:A case report
2019-04-18RuiQingZhangJiaRongZhangShuangDiLi
Rui-Qing Zhang,Jia-Rong Zhang,Shuang-Di Li
Rui-Qing Zhang,Jia-Rong Zhang,Shanghai General Hospital,School of Medicine,Shanghai Jiao Tong University,Shanghai 200120,China
Shuang-Di Li,Shanghai First Maternity and Infant Hospital,Shanghai 200120,China
Abstract
Key words:Partial hydatidiform mole and coexisting fetus;Caesarean section;Second trimester;Case report
INTRODUCTION
A partial hydatidiform mole and coexisting fetus(PHMCF),a rare phenomenon of the past,is showing an upward trend in frequency due to the increasing use of assisted reproductive technologies(ART).The reported incidence of complete hydatidiform mole and coexisting fetus,which is essentially a twin pregnancy,is 1 in 22000-100000 pregnancies[1].However,a PHMCF is a single pregnancy and the reported prevalence is 0.005%-0.01% of all pregnancies[2].The management of such pregnancies creates a dilemma for both the physician and the parents,particularly when the PHMCF occurs during the second trimester of pregnancy.Empirically,the pregnancy is allowed to proceed provided that severe maternal complications are controlled,and the fetal karyotype and development are normal[3].A small number of cases of PHMCF have been reported with certain couples choosing to continue the pregnancy until 28 wk of gestation and delivery was achievedviacaesarean section(CS)resulting in a number of healthy babies[4,5].Unfortunately,in most patients,serious complications can occur,posing significant challenges and difficult choices for both the obstetrician and the patients.For these patients,the main problem is to determine whether the pregnancy is sustainable,and if not,the best way to terminate the pregnancy.Herein,we report the case of a PHMCF patient with severe complications during the second trimester,whose pregnancy was considered unsustainable after careful evaluation and eventually terminated by CS.The timeline is shown in Figure 1.
CASE PRESENTATION
Chief complaints
A 38-year-old Chinese woman was found to have blood pressure instability at 21 wk of gestation and was admitted to our hospital for pre-eclampsia.
总之,汉魏六朝时期的死亡观受到庄子哲学、自然气化论和命定说的交叉影响,体现在遗令文中时常也是混杂在一起的。而且,遗令文中的死亡观也存在着一个故作达观和真正达观的问题,存在着抗俗与顺俗的问题(详下文),需要结合作者的具体情况和为文背景来仔细分辨和探索发现。故作达观者有时是为了排解死亡的恐惧,有时是为了矫时抗俗。真正达观者坦然面对死亡的来临,按照自己的本愿交代后事,但也有人兼顾时俗和儿孙,在本愿和俗情间求一调和,这在后事丧葬安排上十分明显的表现出来。
History of present illness
The patient became pregnant followingin vitrofertilization and embryo transplantation(IVF-ET).Three embryos were transferred into the uterus and only one embryo survived.In early pregnancy,the patient had recurrent episodes of fresh vaginal bleeding.On admission,the couple was informed of the high probability for a poor obstetrical outcome with complications;however,they wished to continue the pregnancy.
History of past illness
The patient(gravida 2,para 0)denied having had hypertension,diabetes and coronary heart disease.The patient denied having had hepatitis and tuberculosis.Moreover,the patient denied a history of food and drug allergy.
Personal and family history
The patient denied a history of drug abuse,smoking,and drinking.The patient denied a family history of genetic disease and cancer.
Physical examination upon admission
The patient’s blood pressure at admission was 160/87 mmHg,and heart rate was 115 bpm.Her temperature and pulse were normal.The fetal heart rate was 140 bpm.
Laboratory examinations

Figure 1 Timeline.
At 13 wk and 3 d,the measurement of serum β-human chorionic gonadotropin(β-HCG)rose to 271600 IU/L,and the result of the Down’s syndrome screening showed a low-risk status.At 21 wk and 4 d,her serum β-HCG level rose to 510427 IU/L,which was abnormally high for the corresponding gestational age.
Imaging examinations
An ultrasound sonographic examination at 55 d of gestational age revealed a single live intrauterine fetus of 7 wk and 4 d,and a blood clot beside it.At 10 wk and 3 d,an ultrasound examination revealed a single live intrauterine fetus of 10 wk and 3 d with a suspected partial hydatidiform mole.However,at 13 wk and 3 d of gestational age,vaginal bleeding disappeared and an ultrasound examination merely revealed a single live intrauterine fetus.At 21 wk and 3 d,a transvaginal sonographic examination revealed a single live intrauterine fetus of 21 wk and 4 d.The left part of the placenta was composed of multiple cystic areas,measuring 126 mm × 42 mm ×114 mm(Figure 2).Two days later,enhanced magnetic resonance imaging revealed a single live intrauterine fetus and abnormal intensified signals at the left part of the placenta with no clear demarcations between the myometrium and placental tissue(Figure 3).The chest computed tomography result was normal.
FINAL DIAGNOSIS
The histopathology was consistent with molar changes(Figure 4).
TREATMENT
A detailed counseling session was provided to discuss the risks of maternal complications,and the couple decided to terminate the pregnancy following careful consideration.CS was chosen because of the heavy vaginal bleeding and the high probability that a medical induction of labor may lead to an incomplete evacuation of the uterus.An infant with weak vital signs and a partially cystic placenta measuring 110 mm × 95 mm × 35 mm were delivered by CS.Thereafter,vesicular tissue,measuring 180 mm × 160 mm × 45 mm,was extracted and the uterus was completely evacuated(Figure 5).
OUTCOME AND FOLLOW-UP
The serum β-HCG levels of the patient decreased to 5258 IU/L after a week.Thepatient was discharged and her weekly follow-up of serum β-HCG levels showed an obvious downward trend.After 5 wk,her serum β-HCG levels decreased to the normal range and no evidence of persistent trophoblastic disease(PTD)or lung metastases was noticed at the 6-mo follow-up.

Figure 2 Transvaginal ultrasonographic images.
DISCUSSION
A PHMCF is always associated with complications such as fetal death,vaginal bleeding,early onset pre-eclampsia,hyperthyroidism,and a risk of gestational trophoblastic neoplasia.Consequently,an early diagnosis of PHMCF has been recommended in order to treat this disease.The diagnosis of PHMCF during the first trimester of pregnancy is mainly revealed by ultrasonographic examinations.Unfortunately,a misdiagnosis is not uncommon on the initial ultrasonography due to the reassuring presence of a fetal heartbeat and the misinterpretation of abnormal placental echoes such as those associated with hematomas[2].Moreover,partial molar pregnancies often present minor cystic changes of the placenta[6],which makes PHMCFs even more difficult to diagnosis.In our case,the ultrasound examination at 55 d revealed a single live intrauterine fetus with a blood clot beside it.At 13 wk of pregnancy,it merely revealed a single live intrauterine fetus.Magnetic resonance imaging can be a useful adjunct to ultrasound for visualizing the normal placental site,the relationship between the fetus and vesicles,and the extension of the disease to the myometrium and parametrium.However,its diagnostic effect in early pregnancy remains unclear[7].Although several PHMCF cases have been successfully diagnosed during the first trimester[8-11],the overall diagnosis rate is still low.Further investigations are required to find more ideal methods to diagnose PHMCF in the first trimester.
When we failed to diagnose PHMCF early and the pregnancy progressed to the second trimester,we considered two factors to determine whether the pregnancy was sustainable.First,severe maternal complications were controlled,and second,the fetal karyotype and development were normal,as stated above.However,even if the pregnancy is allowed to proceed,the overall live birth rate is very low,as listed in Table 1.In addition,a partial molar pregnancy with an embryo of a normal karyotype during the second trimester,may end up as a fetal demise in the third trimester which may be due to placental mosaicism or placental mesenchymal dysplasia[12,13].In our case,we could not acquire the fetal karyotype information because the patient refused to allow an amniocentesis since the fetus appeared normal on sonographic examination.Moreover,the onset of severe vaginal bleeding at 22 wk rendered the pregnancy unsustainable.
Several methods have been reported to terminate PHMCFs during the second trimester.Suction curettage is a safe way to terminate hydatidiform moles[14].However,a mid-term pregnancy with a relatively large fetus precludes the use of suction curettage.Medical termination(using rivanol or misoprostol)is not recommended for molar evacuations since these methods increase maternal complications,including blood loss,incomplete evacuation[15],and the development of PTD due to increased intrauterine pressure[16].Dilatation and evacuation have been recommended by the Evidence-based Practice Guidelines of the Royal College of Obstetricians and Gynecologists as a safe method for termination of pregnancies > 15wk.However,it should be performed by a skilled specialist,and its use in PHMCFs is still questionable.CS has also been reported for terminating PHMCFs.So far,no PTDs have been reported to develop after this procedure.However,the relatively low survival rate of the neonate and the presence of a uterine scar make the CS procedure a difficult choice for both physicians and patients.Hysterectomy is a viable management choice for women in an emergent situation not wishing to maintain fertility[17].Bearing in mind that PHMCF patients often are relatively young,this procedure can cause emotional distress and should be considered very carefully.Moreover,PTDs can still develop after a hysterectomy.

Figure 3 Magnetic resonance imaging scans.
To the best of our knowledge,12 PHMCF cases during the second trimester have previously been reported(Table 1).Three of these cases[15,18,19]of PHMCF were treated with medical termination;unfortunately,all of them resulted in PTDs and metastases.In contrast,two cases[20,21](and our case)were terminated using CSs and no PTDs or metastases developed.Therefore,these results led to the hypothesis that CS termination may be a safer therapeutic strategy during the second trimester with regard to the risk of developing PTDs.
A plausible relationship between gestational trophoblastic disease(GTD)and ART has been established[15].This may be because the clinical factors(advanced maternal age,poor oocyte quality and so on)that exist in IVF patients may also predispose them to GTDs.As PHMCF is a rare kind of GTD,it is imaginable that the PHMCF incidence increases along with the increase in the use of ART.Although no statistical analysis can be done due to the small case numbers,our literature review showed that,in addition to our case,three more cases(1/7)[4,15,19]of PHMCF developed following IVF-ET.This highlighted the possible link between IVF-ET and PHMCF.
A PHMCF during the second trimester poses a considerable challenge both for the patients and the doctors.Once the pregnancy is confirmed to be unsustainable,a suitable termination method should be carefully chosen.According to the knowledge gained from the current case and from the literature review,we can conclude that,compared to medical terminations and dilatation and evacuations,CS is a difficult choice,but may be ultimately safer with regard to the risk of developing PTDs or distant metastases.
CONCLUSION
The CS termination of PHMCFs during the second trimester may be the safest method.

Table 1 Previously reported cases of PHMCF during the second trimester in the literature

Figure 4 Histopathology of the hydatidiform mole.
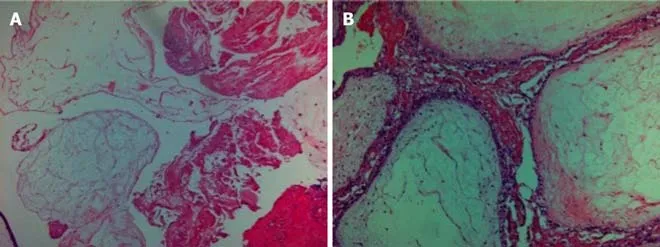
Figure 5 lmages of the gross specimen.
ACKNOWLEDGEMENTS
We thank the Department of Shanghai General Hospital,School of Medicine,Shanghai Jiao Tong University and our patient with her family for their extreme cooperation and support.
猜你喜欢
杂志排行
World Journal of Clinical Cases的其它文章
- Rh-incompatible hemolytic disease of the newborn in Hefei
- Ureteral Ewing’s sarcoma in an elderly woman:A case report
- Anaplastic lymphoma kinase-negative anaplastic large cell lymphoma masquerading as Behcet's disease:A case report and review of literature
- Synchronous quadruple primary malignancies of the cervix,endometrium,ovary,and stomach in a single patient:A case report and review of literature
- Sister Mary Joseph’s nodule in endometrial carcinoma:A case report
- Alternative technique to save ischemic bowel segment in management of neonatal short bowel syndrome:A case report
