Comparative analysis of robotic vs laparoscopic radical hysterectomy for cervical cancer
2019-04-18LiChenLiPingLiuNaWenXiaoQiaoYuanGuangMeng
Li Chen,Li-Ping Liu,Na Wen,Xiao Qiao,Yuan-Guang Meng
Li Chen,Na Wen,Yuan-Guang Meng,Department of Obstetrics and Gynecology,Chinese PLA General Hospital,Beijing 100853,China
Li-Ping Liu,Department of Obstetrics and Gynecology,The First Central Hospital of Baoding,Baoding 071000,Hebei Province,China
Xiao Qiao,Medical Big Data Center,Chinese PLA General Hospital,Beijing 100853,China
Abstract
Key words:Cervical cancer;Robotic radical hysterectomy;Laparoscopy;Survival
INTRODUCTION
Cervical cancer is the most common gynecological malignancy,ranking first in female reproductive malignancies with more than 500000 new cases and 275000 deaths each year[1].In China,the incidence of cervical cancer varies across different regions.Women between 40 and 50 years old have higher incidence rates.The incidence in rural and mountain areas is higher than that in urban areas and on the plains[2-4].
Surgical resection with adequate lymphadenectomy is the main treatment for improving the survival rate of patients with cervical cancer.Traditionally,open radical hysterectomy(ORH)is considered the standard surgical procedure for the treatment of resectable cervical cancer.In 1992,Nezhatet al[5]first reported laparoscopic radical hysterectomy(LRH)for the treatment of cervical cancer.Since then,LRH has been reported with satisfactory surgical outcomes,compared with traditional open surgery[6].The latest guidelines from the National Comprehensive Cancer Network and the European Society of Gynecological Oncology suggest that open surgery and laparoscopic surgery(using traditional laparoscopic or robotic techniques)are the main surgical approaches for radical hysterectomy for patients with stage IA2-IIA cervical cancer[7-9].Robotic surgery has been increasingly used in abdominal surgery and has shown more beneficial effects[10-12].
In 2006,Sertet al[13]first published the results of robotic radical hysterectomy(RRH)with lymphadenectomy.To date,there have been relatively more studies of RRH for cervical cancer in foreign countries[14-19].Our center started to provide a service to perform RRH for cervical cancer relatively early in China,and it has also accumulated rich clinical experience.
This study was retrospectively performed to analyze the perioperative conditions,complications,and short-term and long-term effects in patients undergoing RRH and LRH in our center from February 2014 to December 2018,with an aim to comparetheir clinical efficacy,safety,and feasibility.
MATERIALS AND METHODS
The perioperative data of patients undergoing RRH and LRH were extracted and collected from the database of surgical treatments for cervical cancer(from February 2014 to December 2014)for statistical analysis.
Inclusion and exclusion criteria
The inclusion criteria included:(A)Patients with newly diagnosed cervical cancer[International Federation of Gynecology and Obstetrics(FIGO,2009)stage IA-IIB];(B)Patients with pathological diagnoses of squamous cell carcinoma,adenocarcinoma,or adenosquamous carcinoma;and(C)Patients with complete medical records who provided written informed consent for surgery.The exclusion criteria included:(A)Patients with uterine length greater than 12 cm;(B)Pregnant patients;(C)Patients with restrictions for creating a pneumoperitoneum;(D)Patients with clinical and radiological evidence showing lymph node and distant metastases;(E)Patients with histories of abdominal or pelvic chemoradiotherapy;(F)Patients without follow-up data available;and(G)Patients with histories of multiple primary malignancies.
Standardized regimen
The design of this study and the standardized regimen were approved by the Ethics Committee of the General Hospital of the People’s Liberation Army.After patient admission,the relevant examinations were completed;the patients were informed of the surgical risk and provided their written informed consent.The procedures were performed by surgical specialists and much the same team.
RRH for cervical cancer
After general anesthesia with tracheal intubation,the patient was placed in the lithotomy position with 30° elevation of the feet.The pneumoperitoneum pressure was maintained at 14 mm Hg.Preparation of the Da Vinci robotic surgical system is as follows.Two trocars were placed in the site 8 cm above the umbilicus and 30° to 45° to the right and at a site 8 cm above the umbilicus in the middle line,respectively.After creation of the pneumoperitoneum and camera placement,the trocar for the robotic arms was placed under camera guidance.The trocars were located at sites 7 to 8 cm lateral to the umbilicus and formed fan-shaped distribution with the trocar for the camera.Robotic arms 1 and 2 were attached to the trocars.The monopolar electrosurgical knife/shovel and bipolar forceps were placed.Another 2 ancillary trocars were placed.
LRH for cervical cancer
The pelvic and abdominal cavities were examined,and adhesions were lysed.The infundibulopelvic ligament and the round ligament on the right side were divided after high ligation.The anterior and posterior leaves of the broad ligament were opened gradually.The uterovesical fold was opened with scissors.The same procedure was performed on the left side for this step.The posterior peritoneum was opened to sequentially remove the bilateral common iliac lymph nodes,external iliac lymph nodes,deep inguinal lymph nodes,internal iliac lymph nodes,and obturator lymph nodes.The right uterine artery was divided to unroof the ureter and manage the sacrospinous ligament and cardinal ligament.The same procedure was performed on the left side for this step.The remaining parametrial tissues and the upper 1/3 of the vagina were resected.After specimen removal,the vaginal stump was closed with continuous sutures.The pelvic cavity was thoroughly evaluated.The pelvic cavity was irrigated,and hemostasis was performed if necessary.The drainage tube and urinary catheter were placed,and the procedure was completed.After the procedure,the patient’s pathological report was evaluated.Patients with lymph node metastasis,parametrial involvement,positive vaginal margins,lymphatic involvement,tumor invasion to deep interstitial regions,and large tumors(≥ 4 cm)underwent adjuvant therapy,such as radiotherapy and chemotherapy.
Statistical analysis
SPSS software(IBM statistics,version 22.0)was used for statistical analyses of the experimental data.The continuous parameters are expressed as the mean ± SD.The categorical variables are described as the positive rate(ratio).The pairedt-test and the chi-square test were used for the statistical analysis.P< 0.05 was considered to be statistically significant between the two groups.
RESULTS
Demographic data
A total of 558 cervical cancer patients who were admitted between February 2014 and December 2018 were included in this study.Of the patients,342 underwent LRH for cervical cancer,and 216 underwent RRH.The age of the patients was 47.49 ± 9.81 years old and 48.90 ± 9.65 years old in the LRH and RRH groups,respectively.The body mass index was 23.74 ± 2.96 kg/m2and 24.20 ± 3.37 kg/m2in the LRH and RRH groups,respectively(Table 1).
Stage IA1-IB1 patients accounted for 60.82% and 61.57% of all patients in the LRH and RRH groups,respectively.The stage IB2-IIA1 patients accounted for 36.55% and 35.65% of all patients in the LRH and RRH groups,respectively.Squamous cell carcinoma(92.40% and 90.74%)and adenocarcinoma(7.02% and 8.80%)were the main pathological types in the LRH and RRH groups,and there were two patients with adenosquamous carcinoma in the LRH group(P= 0.504).
Comparative parameter analysis related to the procedures and postoperative adjuvant therapy
In the comparison of the main parameters of the procedure,the operative time and estimated intraoperative blood loss were significantly less in the RRH group than in the LRH group(operative time:197.16 ± 57.76vs233.50 ± 59.76 min,P< 0.001;blood loss:163.09 ± 320.95vs233.50 ± 59.76 min,P< 0.001;Table 2).The number of dissected lymph nodes during surgery(23.51 ± 9.31vs25.09 ± 11.41,P= 0.748),length of postoperative hospital stay(12.28 ± 5.06vs10.87 ± 4.44,P= 0.772),and total length of hospital stay(18.57 ± 5.61vs17.19 ± 6.29,P= 0.777)were not statistically significantly different between the RRH and LRH groups.The proportion of blood transfusions in the RRH group(3.80%,8 cases)was significantly less than that in the LRH group(11.57%,39 cases)(P< 0.001).
There was no statistically significant difference in the intra-operative injury rate(2.31%vs0.87%,P> 0.05)between the two groups.There were four cases of vascular injury and one case of bladder injury in the RRH group and three cases of vascular injury in the LRH group.
The postoperative radiotherapy rates were 47.22%(102 patients)and 50.29%(172 patients),respectively;the postoperative chemotherapy rates were 11.57%(25 patients)and 12.28%(42 patients)in the two groups.There was no significant difference in the postoperative radiotherapy or chemotherapy rates between the two groups(P= 0.268 andP= 0.457,respectively).
Comparative analysis of postoperative complications
The total complication rate was 9.65%(20 patients)in the RRH group and 17.59%(60 patients)in the LRH group(Table 3).The complication rate was significantly lower in the RRH group than in the LRH group.
Early postoperative complications(within 4 wk after surgery)were mainly infections and fever(body temperature ≥ 38.0 °C).The early infection rate and fever rate were significantly lower in the RRH group than in the LRH group(infection:1.46%vs3.70%,P= 0.007;fever:4.39%vs6.48%,P= 0.017).The infections mainly included wound infections(2 cases and 9 cases)and urinary tract infections(1 case and 3 cases).A case of lower extremity venous thrombosis occurred after surgery in the RRH group.A urethral fistula was reported in a patient in the RRH group,and intestinal obstruction was reported in two patients in the LRH group.
Long-term postoperative complications(after 4 wk postoperatively)were mainly associated with lymphatic drainage disorder after lymphadenectomy(Figure 1).The incidence of lower extremity edema was significantly lower in the RRH group than in the LRH group(3.8%vs4.63%,P= 0.036).There was no statistically significant difference in the incidence of inguinal lymphocysts(1.39%vs0.88%,P= 0.429).
Comparative analysis of postoperative follow-up results and survival curves
The follow-up periods were 30.07 ± 15.67 mo and 29.48 ± 15.07 mo in the RRH and LRH groups,respectively(Table 4).There was no significant difference in follow-up period(P= 0.658).The total recurrence rates were 15.7% and 12% in the RRH and LRH groups,respectively.The progression-free survival time was 28.91 ± 15.68 mo and 28.34 ± 15.13 mo in the RRH and LRH groups,respectively,and the difference in progression-free survival time was not statistically significant(P= 0.669).The overall survival(OS)rates were 92.13% and 94.45% in the RRH and LRH groups,respectively,and there was no significant difference between them(P= 0.292).The OS time was 29.87 ± 15.92 mo and 29.41 ± 15.14 mo in the RRH and LRH groups,respectively(P= 0.732).
The survival curves and the progression-free survival curves were not statisticallysignificantly different between the RRH and LRH groups(P= 0.407 andP= 0.28,respectively).
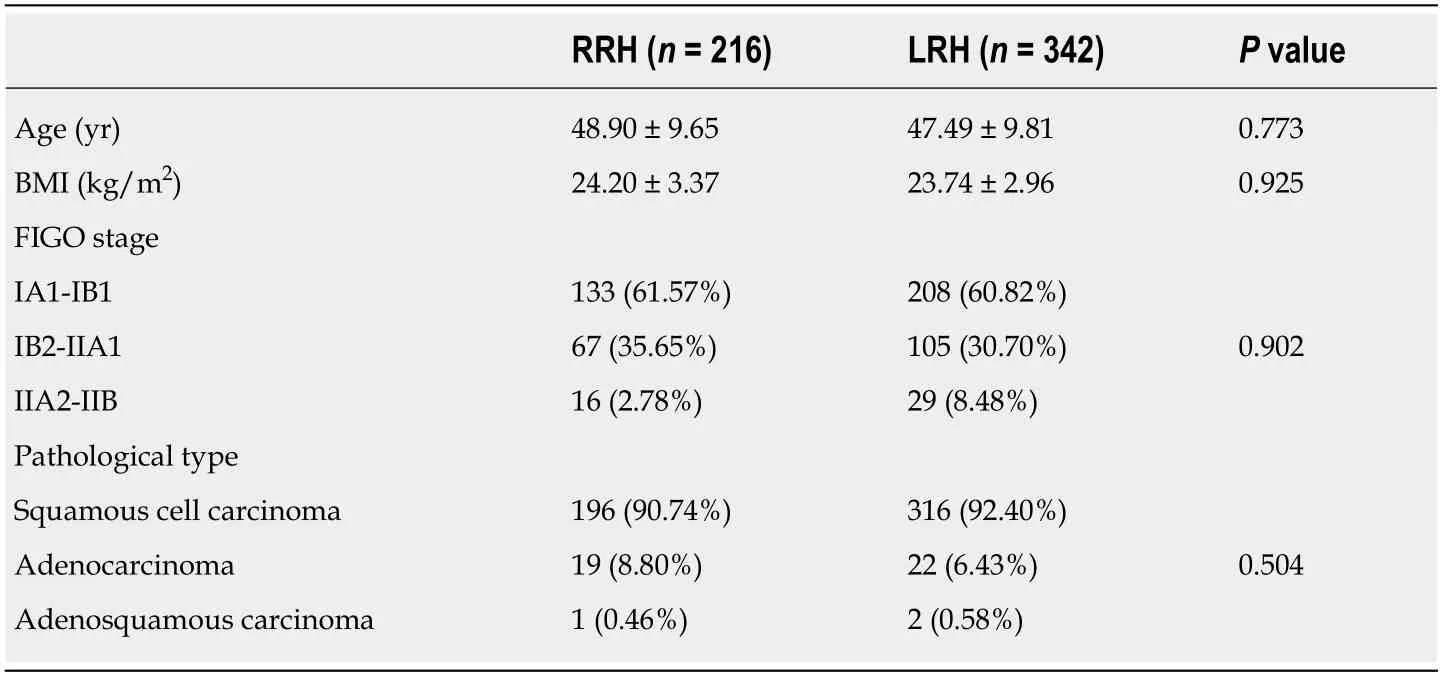
Table 1 Baseline demographic data of patients in the robotic radical hysterectomy and laparoscopic radical hysterectomy groups
DISCUSSION
According to statistics from the World Health Organization,more than 90% of new cases and deaths of patients with cervical cancer worldwide were reported in developing countries[7,20-23].To date,the treatments for cervical cancer include surgery,radiation therapy,and chemotherapy.
As one of the important approaches to cervical cancer treatment,surgical treatment has evolved from transabdominal surgery,transvaginal surgery,and laparoscopic surgery to robotic surgery.Compared with ORH,LRH has advantages including cosmetic incisions,less trauma,quick healing,a clear and accurately magnified surgical field,rapid recovery,and fewer complications[11,24,25].However,it has many shortcomings:The poor accuracy of the surgical field on two-dimensional imaging;the limited range of instrument flexibility,which is not conducive to fine surgical operations;and the long learning curve,which means that extensive practice is needed to master the procedure[26].The da Vinci robotic surgery system somewhat overcomes these shortcomings and has greater accuracy and stability for the operation.Thus,it has been widely used in the treatment of gynecological diseases[27-32].
A study by Boggesset al[33]compared the results of 51 patients undergoing RRH and 49 patients undergoing LRH and showed that type III pelvic lymphadenectomy is feasible during RRH and might be superior to that during LRH in patients with early cervical cancer.
The current study included more patients than the previous studies,including 216 patients undergoing RRH and 342 patients undergoing LRH.There were no differences in the basic characteristics between the two groups.However,the operative time and blood loss were significantly less in the RRH group than in the LRH group.
According to the literature,the incidences of urinary and vascular injuries were 3.3% and 6%,respectively,in patients undergoing open radical hysterectomy[34].In the current study,a patient in the RRH group experienced intraoperative urinary tract injury and a ureterovaginal fistula after surgery.The incidence of urinary injury was 0.46%.There were 4 and 3 cases of vascular injury in the RRH and LRH groups,respectively.The incidences were 1.85% and 0.87%,respectively.The incidence of intraoperative injury was significantly lower than that reported in the previous ORH study.
The main evaluation parameters of the surgical efficacy of malignant tumors are the recurrence rate and survival rate of patients after surgery.To date,there have been few reports about the recurrence rate and survival rate in patients undergoing RRH and LRH.Kawalet al[35]performed a follow-up in 109 patients undergoing RRH.The recurrence rate was 16.5%.The 2-year and 5-year OS rates were 96% and 89%,respectively.The 2-year and 5-year DFS rates were 88% and 72%,respectively.
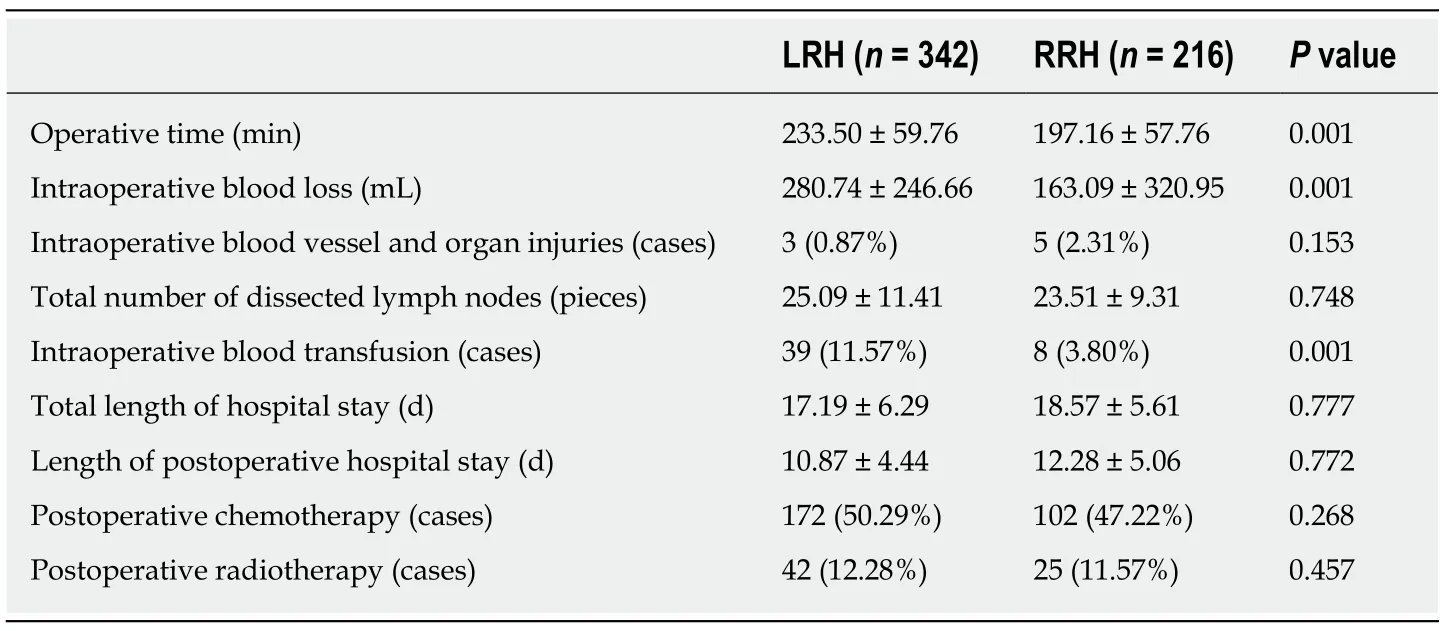
Table 2 Operative and postoperative adjuvant treatment parameters in the robotic radical hysterectomy and laparoscopic radical hysterectomy groups
With the publication of a large,prospective,multicenter randomized,controlled trial of minimally invasive(laparoscopic and robotic surgery)radical hysterectomy for cervical cancer and open radical hysterectomy for cervical cancer in New England Journal of Medicine in 2018,the postoperative efficacy of minimally invasive surgery has once again drawn widespread attention[36].The study showed that,compared with open surgery,minimally invasive surgery had a significantly higher recurrence rate and a poorer survival rate.It remains a problem widely acknowledged by the medical community whether minimally invasive surgery,especially laparoscopic surgery,can reduce residual tumors through technological innovations.
Corradoet al[17]demonstrated possible differences in perioperative outcomes and complications between mLRH and RRH in patients with early-stage cervical cancer.Their studies showed that the surgical efficiency of microlaparoscopic surgery is comparable to that of robotic surgery.Therefore,this result suggests room for improvement in the surgical accuracy of and reduced surgical trauma with laparoscopic techniques.
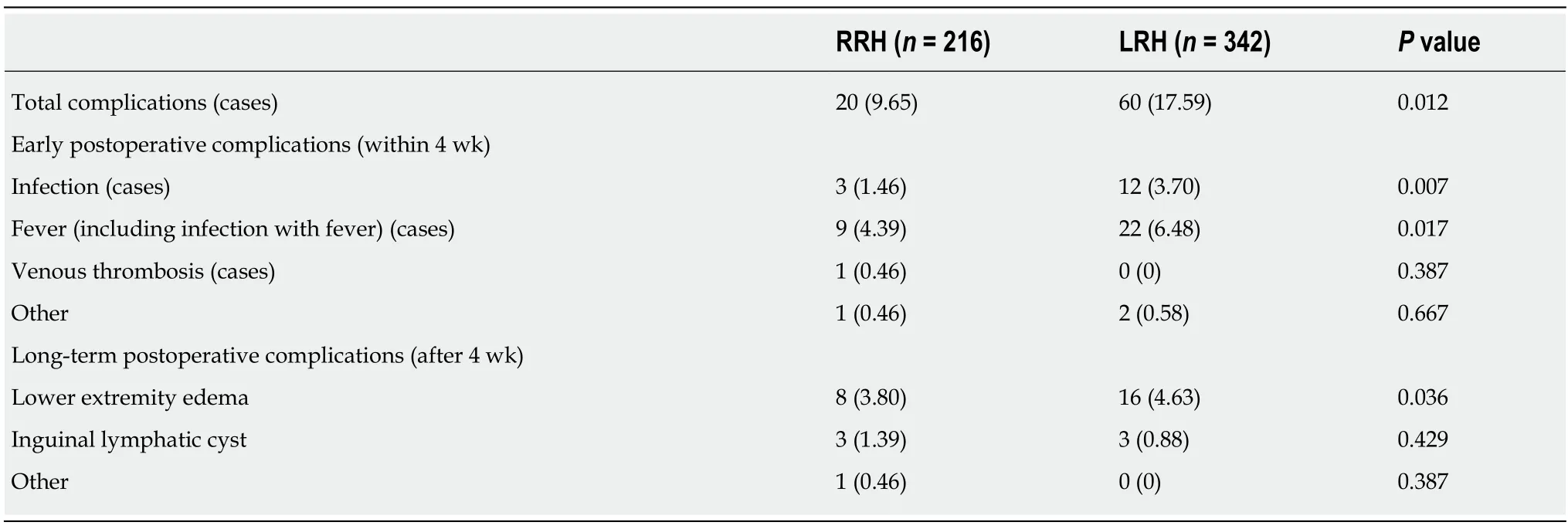
Table 3 Postoperative complications in the robotic radical hysterectomy and laparoscopic radical hysterectomy groups,n(%)
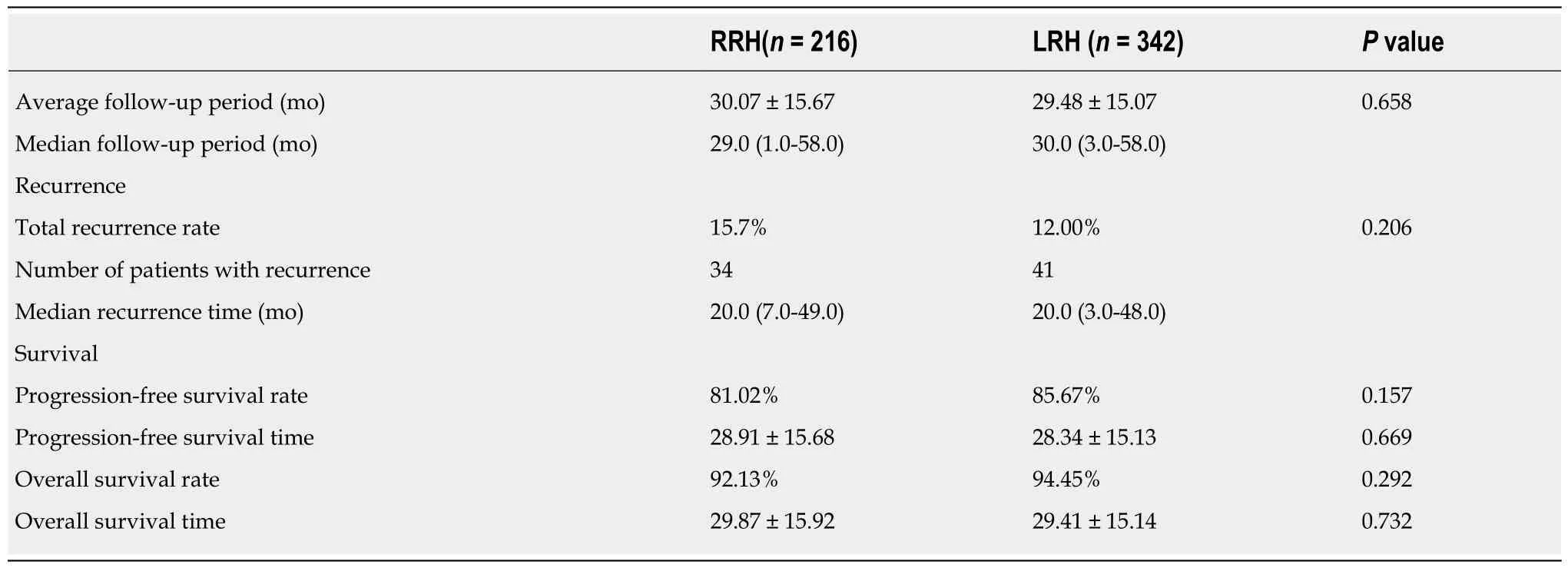
Table 4 Follow-up data in the robotic radical hysterectomy and laparoscopic radical hysterectomy groups
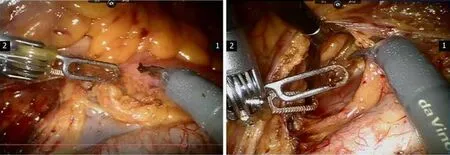
Figure 1 Pelvic lymphadenectomy during robot-assisted radical hysterectomy for cervical cancer.
ARTICLE HIGHLIGHTS
Research background
The da Vinci robotic surgery system somewhat overcomes the shortcomings of LRH and has greater accuracy and stability for the operation.Thus,it has been widely used in the treatment of gynecological diseases
Research motivation
This study was retrospectively performed to analyze the perioperative conditions,complications,and short-term and long-term effects in patients undergoing robotic radical hysterectomy(RRH)and laparoscopic radical hysterectomy(LRH)at our center from February 2014 to December 2018.
Research objectives
To analyze the perioperative conditions,complications,and short-term and long-term effects in patients undergoing RRH and LRH.
Research methods
The clinical efficacy,safety,and feasibility of RRH and LRH were analyzed and compared.
Research results
The complication rate was significantly lower in the RRH group than in the LRH group.There was no significant difference in follow-up period(P= 0.658).The total recurrence rates were 15.7% and 12% in the RRH and LRH groups,respectively.The progression-free survival time was 28.91 ± 15.68 mo and 28.34 ± 15.13 mo in the RRH and LRH groups,respectively(P= 0.669).The overall survival(OS)rates were 92.13% and 94.45% in the RRH and LRH groups,respectively(P= 0.292).The OS time was 29.87 ± 15.92 mo and 29.41 ± 15.14 mo in the RRH and LRH groups,respectively(P= 0.732).The survival curves and the progression-free survival curves were not statistically significantly different between the two groups.
Research conclusions
The operative time and blood loss were significantly less in the RRH group than in the LRH group.The two groups had similar complication rats,OS,and progression-free survival time.
Research perspectives
RRH can achieve similar long-term outcome to LRH with less operative time and less blood loss.
杂志排行
World Journal of Clinical Cases的其它文章
- Clinical use of low-dose aspirin for elders and sensitive subjects
- Distribution and drug resistance of pathogenic bacteria in emergency patients
- Feasibility of laparoscopic isolated caudate lobe resection for rare hepatic mesenchymal neoplasms
- Soft tissue release combined with joint-sparing osteotomy for treatment of cavovarus foot deformity in older children:Analysis of 21 cases
- Clinical characteristics of sentinel polyps and their correlation with proximal colon cancer:A retrospective observational study
- Longitudinal observation of intraocular pressure variations with acute altitude changes
