Comorbidity of bipolar and anxiety disorders: An overview of trends in research
2019-03-21MamidipalliSaiSpoorthySubhoChakrabartiSandeepGrover
Mamidipalli Sai Spoorthy, Subho Chakrabarti, Sandeep Grover
Abstract Over the last three decades burgeoning research has shown that anxiety disorder comorbidity is not only highly prevalent in bipolar disorder (BD), but it also adversely impacts the course, outcome, and treatment of BD. The present review provides an overview of the current trends in research on comorbid anxiety and BDs based on prior reviews and meta-analyses (n = 103), epidemiological surveys, and large-scale clinical studies. The results reiterated the fact that at least half of those with BD are likely to develop an anxiety disorder in their lifetimes and a third of them will manifest an anxiety disorder at any point of time. All types of anxiety disorders were equally common in BD. However, there was a wide variation in rates across different sources, with most of this discrepancy being accounted for by methodological differences between reports. Comorbid anxiety disorders negatively impacted the presentation and course of BD. This unfavourable clinical profile led to poorer outcome and functioning and impeded treatment of BD. Despite the extensive body of research there was paucity of data on aetiology and treatment of anxiety disorder comorbidity in BD. Nevertheless,the substantial burden and unique characteristics of this comorbidity has important clinical and research implications.
Key words: Comorbidity; Bipolar disorder; Anxiety disorders; Correlates; Impact;Aetiology; Treatment
INTRODUCTION
Comorbidity is defined as the ‘presence of more than one disorder in a person in a defined period of time'[1]. Prior to the 1990s the focus was mostly on the link between anxiety disorders and unipolar depression, while substance-use disorders (SUDs)were the focus of research on comorbidity in bipolar disorder (BD). However,accumulated evidence over the last three decades has conclusively established that comorbidity with anxiety disorders is the rule rather than the exception among patients with BD[2-5]. In general, about a half to two thirds or even more of the patients with BD have a comorbid psychiatric condition. Anxiety disorders, SUDs, and behavioural disorders are the most common comorbid psychiatric disorders associated with BD. Very high lifetime and current rates of anxiety disorder comorbidity have been found in both epidemiological[5-9]and clinical studies of BD[5,6,8,10,11]. Additionally, multiple anxiety disorder comorbidity has been reported in a third of the patients with BD[12-16]. Despite differing widely across studies, rates of individual anxiety disorders comorbid with BD appear to be largely similar[11,17-20]. The presence of comorbid anxiety disorders in patients with BD has several adverse consequences including a negative impact on almost all aspects of the presentation and course of BD[10,15,21-23]. This unfavourable clinical profile leads to poorer outcome and functioning and impedes treatment of BD[16,17,20,24,25].
The increased awareness of the substantial burden of comorbid bipolar and anxiety disorders over the years has propelled research in this area[5,26]. Moreover, it gave rise to the hope that examination of anxiety disorder comorbidity in BD could provide clues to underlying etiopathogenetic mechanisms of BD[3,6,9]. Consequently, the existing literature now contains a sizeable body of research evidence on the subject[6,8,16,18]. However, there are several unresolved issues as well. This review intends to highlight both the well-known facts and the deficiencies in research concerning anxiety disorder comorbidity in BD. A major problem hampering research in this area has been the widely varying methodology of individual studies[20,26,27]. To obviate these methodological concerns to whatever extent possible, the current review is based on three of the relatively more reliable sources of evidence including prior reviews and meta-analyses, as well as epidemiological surveys and large-scale clinical studies of comorbid anxiety disorders and BD.
OBJECTIVES
The principal objective of this review was to provide an overview of the current trends in research on comorbidity of bipolar and anxiety disorders. The main areas examined included rates of anxiety disorder comorbidity in BD, its demographic and clinical correlates, the impact of such comorbidity on the course and outcome of BD,and research on management and aetiological mechanisms of comorbid anxiety and BDs.
LITERATURE SEARCH
A comprehensive literature search was undertaken using six English-language databases: MEDLINE, PubMed, PsycINFO, EMBASE, Cochrane, and Google to identify published articles on anxiety disorders comorbid with BD from inception until August 2018. Search terms included BD, or bipolar depression, or mania AND comorbid, or comorbidity AND anxiety, or generalized anxiety disorder (GAD), or panic disorder, or phobia, or phobic disorder, or social anxiety disorder, or obsessivecompulsive disorder (OCD), or post-traumatic stress disorder (PTSD). Reviews,editorials and original research articles were examined for their relevance to the subject. Reference lists of these articles were searched manually to locate other relevant reports.
SELECTION OF ARTICLES
All articles that provided information on prevalence, clinical features, aetiology, and treatment of anxiety disorder comorbidity in BD were chosen initially. However, for the purposes of the current review only three sources of evidence including earlier reviews (meta-analytic, systematic, and open), epidemiological investigations, and large-scale (usually multi-centric) clinical studies were included. Other original research articles were considered only when they provided additional information not present in these three principal sources.
DATA EXTRACTION AND SYNTHESIS
Data on different aspects of anxiety disorder comorbidity in BD were extracted from each source. Results were organized by identifying common patterns and trends so that logical conclusions could be drawn from the findings of the articles included.
EVIDENCE-BASE FOR THE CURRENT REVIEW
The electronic search yielded 1294 articles, 249 of which were reviews about anxiety disorder comorbidity in BD. Relevant reviews were extracted from this initial list of 249 articles. A manual search was also conducted to identify any other reviews on the topic. After excluding duplicate publications, 103 reviews on the subject were finally included. The final selection contained 14 meta-analytic reviews, 29 systematic reviews, and 60 open (non-systematic) reviews. Incidentally, the literature search also yielded over 350 relevant studies on comorbid bipolar and anxiety disorders.However, only a selected list of articles pertaining to epidemiological and large-scale clinical studies was included in this review.
OVERALL PREVALENCE OF ANXIETY DISORDERS IN BD
Data from meta-analytic and systematic reviews are included in Table 1, while Table 2 depicts the rates obtained as a part of non-systematic reviews. Prevalence rates from epidemiological studies are shown in Table 3 and from selected large-scale clinical studies in Table 4.
The first notable finding across all sources included in this review was the wide variation in prevalence rates between different reviews, epidemiological surveys, and clinical studies. The obvious reason for this discrepancy was differences in designs and methodologies of reviews and individual studies. However, despite these differences there appeared to be some consistency in the rates reported from different sources.
Reviews
Four meta-analyses of lifetime prevalence rates of anxiety disorders among adult patients with BD yielded very similar rates of 41% to 47% from both community and clinical populations[11,18-20]. Current rates of anxiety disorder comorbidity among adult patients ranged from 35% to 38% in two meta-analyses of epidemiological and clinical studies of BD[20,35]. Mean prevalence rates in children/adolescents were found to be 27% (range 15% to 43%) in one meta-analysis[29]and 44% in another[34], which was in keeping with the adult rates. There was a greater variation in rates (11% to 93%)derived from systematic reviews depending on the number and type of studies included in each review. Nevertheless, systematic reviews among adult patients have also reported lifetime anxiety comorbidity in about half and current comorbidity in about a third of those with BD. Incidentally, the systematic review with the largest number of studies (n = 167) has been conducted among those with child/adolescent BD[43]. The mean prevalence rate of any anxiety disorder in BD was found to be 54% in this review (range 41% to 80%). A much greater disparity in rates was found in the non-systematic reviews, but even in these reviews the average lifetime prevalence was close to 50% and the average current prevalence was about 30% for anxiety disorders in BD. Rates for prevalence among the elderly appeared to be lower (mean23%)[54], while average rates among children/adolescents seemed to be higher (range 14% to 77%) than adult rates[56,58,59].

Table 1 Prevalence of anxiety disorder comorbidity in bipolar disorder: Evidence from meta-analytic and systematic reviews
Epidemiological and clinical studies
Some of the highest rates of anxiety disorder comorbidity in BD have been reported in epidemiological surveys. In these studies, a minimum of one third of the patients with BD appeared to have a lifetime comorbid anxiety disorder[88], with some epidemiological studies reporting exceptionally high lifetime rates of 89% to 100%[76,78,90]. However, most epidemiological investigations have found lifetime rates of about 50% to 60% in those with BD. Current rates were lower and ranged from 7% to 52% in three studies[97-99]. The high rates obtained in epidemiological studies could be explained by the large number of patients examined, many of whom may have never sought treatment. Alternatively, they could be due to the high rates of false positive diagnoses made by lay interviewers who are usually employed to carry out these population surveys[26]. In contrast, while diagnostic ascertainment may be more reliable in clinical settings, clinical samples are also more likely to include severely ill patients with higher chances of having comorbid disorders (the so called Berkson's bias)[8,16,26]. Still, lifetime rates of anxiety comorbidity in BD were about 40% to 50%,while current rates were about 30% across several large-scale clinical studies. Thus,though rates in community samples were somewhat higher than clinical populations[26], these differences were not significant as indicated by two metaanalytic reviews[19,35].
Remitted patients
Although some evidence suggested that anxiety disorder comorbidity was higher during acute, particularly depressive episodes[8,35], reviews of studies of remitted patients with BD have found that about a third to half of such patients (range 7% to 61%) have a comorbid anxiety disorder[16,35,119]. A recent meta-analysis of remitted BD found that the current prevalence rate for any anxiety disorder was 35%, thus confirming that anxiety disorder comorbidity extends beyond the acute to the interepisodic period[35].
Multiple comorbidity
About a third of the patients with BD also develop more than one anxiety disorder during their lifetimes[8,10,27,60]. Rates of such multiple anxiety disorder comorbidity have ranged from 10% to 47% in different studies of BD[9,13-16].
BD in anxiety disorders
The prevalence of BD in anxiety disorders has been examined less often. Though some reviews have reported low rates of BD in primary anxiety disorders[18,40], the majority of reviews and studies have found that the prevalence of BD in anxiety disorders is equivalent to the rates of anxiety disorders in patients with BD[7,8,66,80,128].This appears to be mainly true for OCD[30,32,128,129], but a similar trend has also been found for social phobia and panic disorder[7,8,46,66,128].
PREVALENCE OF INDIVIDUAL ANXIETY DISORDERS IN BD
Not surprisingly, the greatest discrepancy was found in the prevalence of individual anxiety disorders in BD. Nonetheless, some uniform trends were evident from the three different sources of evidence of this review.
The four meta-analytic reviews among adults have reported highest lifetime rates for panic disorder (17% to 22%), GAD (13% to 20%), and social phobia (20%), followed by PTSD (11% to 17%), social anxiety disorder (13%), OCD (10% to 13%), specific phobias (11%), and agoraphobia (8%)[11,18-20]. A similar trend was also apparent in a meta-analysis of remitted patients[35]. Among children/adolescents the mean prevalence of GAD (25%) was very high, as were the rates of separation anxiety disorder (22%), OCD (17%), and social phobia (15%)[34]. Reviews of individualdisorders have usually confirmed these rates. The prevalence of OCD in BD was about 17% (range 11% to 23%) among adults and children/adolescents in three metaanalyses and one systematic review[30-32,42]. The lifetime prevalence of GAD was found to be 15% and that of panic disorder 16% in two separate meta-analyses[36], while a systematic review estimated the lifetime rates of PTSD to vary from 16% to 39%[39].

Table 2 Prevalence of anxiety disorder comorbidity in bipolar disorder: Evidence from open reviews

BD: Bipolar disorder; BP I: Bipolar disorder subtype I; BP II: Bipolar disorder subtype II; AGORA: Agoraphobia; GAD: Generalized anxiety disorder; OCD:Obsessive compulsive disorder; PD: Panic disorder; PTSD: Post-traumatic stress disorder; SAD: Social anxiety disorder; SEP ANX: Separation anxiety disorder; SOC PHOBIA: Social phobia; SP PHOBIA: Specific phobia.
Epidemiological studies, on the other hand have found very high lifetime rates of comorbid phobias in BD including specific phobias, agoraphobia, social phobia, and social anxiety disorder. This is understandable given that phobic disorders are among the most common disorders found in general population surveys[131-134]. Lifetime rates of GAD were also very high while rates of other disorders were more variable.Consequently, most systematic as well as non-systematic reviews based on both epidemiological and clinical studies have found a similar pattern of prevalence of individual anxiety disorders in BD[8-10,22]. While some clinical studies have also found a comparable distribution of anxiety disorders, the more usual finding has been that panic disorder, PTSD, and OCD are about as common as phobic disorders and GAD.
DEMOGRAPHIC CORRELATES OF ANXIETY DISORDER COMORBIDITY IN BD
Correlates of anxiety disorders among patients with BD are depicted in Table 5. Few studies have examined demographic correlates of comorbid bipolar and anxiety disorders. The association with age has yielded conflicting results[8,9,40,70], except for OCD comorbidity in BD, where younger patients have been found to have higher rates in a series of meta-analyses and systematic reviews[20,30,32,40,42]. In contrast, gender seemed to make a significant difference to the prevalence of comorbid anxiety disorders in BD in some studies. Higher prevalence of anxiety disorders has been reported among women, particularly from large-scale clinical studies such as those conducted by the Stanley Foundation[104]. However, the Systematic Treatment Enhancement Program for Bipolar Disorder and other studies have not been able to reproduce these gender differences[52]. There was similar inconsistency among epidemiological studies with some reporting higher prevalence of anxiety disorders in women with BD[74,85]and others finding equivalent rates between the two genders[76,99].One meta-analysis found a significant excess of anxiety disorders among women with BD based on pooled prevalence rates from several studies[18], but many other metaanalyses and reviews have concluded that there are no gender differences in rates of anxiety disorder comorbidity in BD. The association of anxiety disorders with other demographic variables such as marital status, education, or socioeconomic class has been similarly characterized by inconsistent and contradictory results. On the other hand, there was some preliminary evidence of cross-national and ethnic differences in the prevalence of anxiety disorder comorbidity in BD. Geographical variations in rates of anxiety disorders have been found in several meta-analyses and systematic reviews[11,19,30,42]. Ethnic differences have also been noted in epidemiological studies[74].Notably, some reviews have found lower rates of anxiety disorders among Asian patients with BD; genetic differences have been proposed to account for this finding[69,122,135].
CLINICAL CORRELATES OF ANXIETY DISORDER COMORBIDITY IN BD
Unlike demographic variables, there appeared to be considerably more uniformity regarding clinical correlates of anxiety comorbidity in BD.
Age of onset
Joslyn et al[136]examined the effects of age of onset of BD on the clinical profile and outcome of BD in a meta-analysis of 15 studies including 7370 patients. An earlier age of onset was found to be significantly associated with comorbid bipolar and anxietydisorders with an odds ratio of more than two. The association with early onset has been replicated by other meta-analytic reviews of total anxiety disorder comorbidity and meta-analyses of individual anxiety disorders including comorbid GAD, OCD,and panic disorders[18,20,30,33,36]. This relationship has been further endorsed by several systematic reviews of comorbid anxiety disorders in BD[9,10,16,17,22]. Higher prevalence of anxiety disorders among those with a younger age of onset has also been found in epidemiological surveys[73,80,86,93,132]as well as large-scale clinical studies of BD[100,106,107,110,113]. Moreover, earlier age of onset has been associated with poorer outcome in patients with BD and comorbid anxiety disorders[8,17].
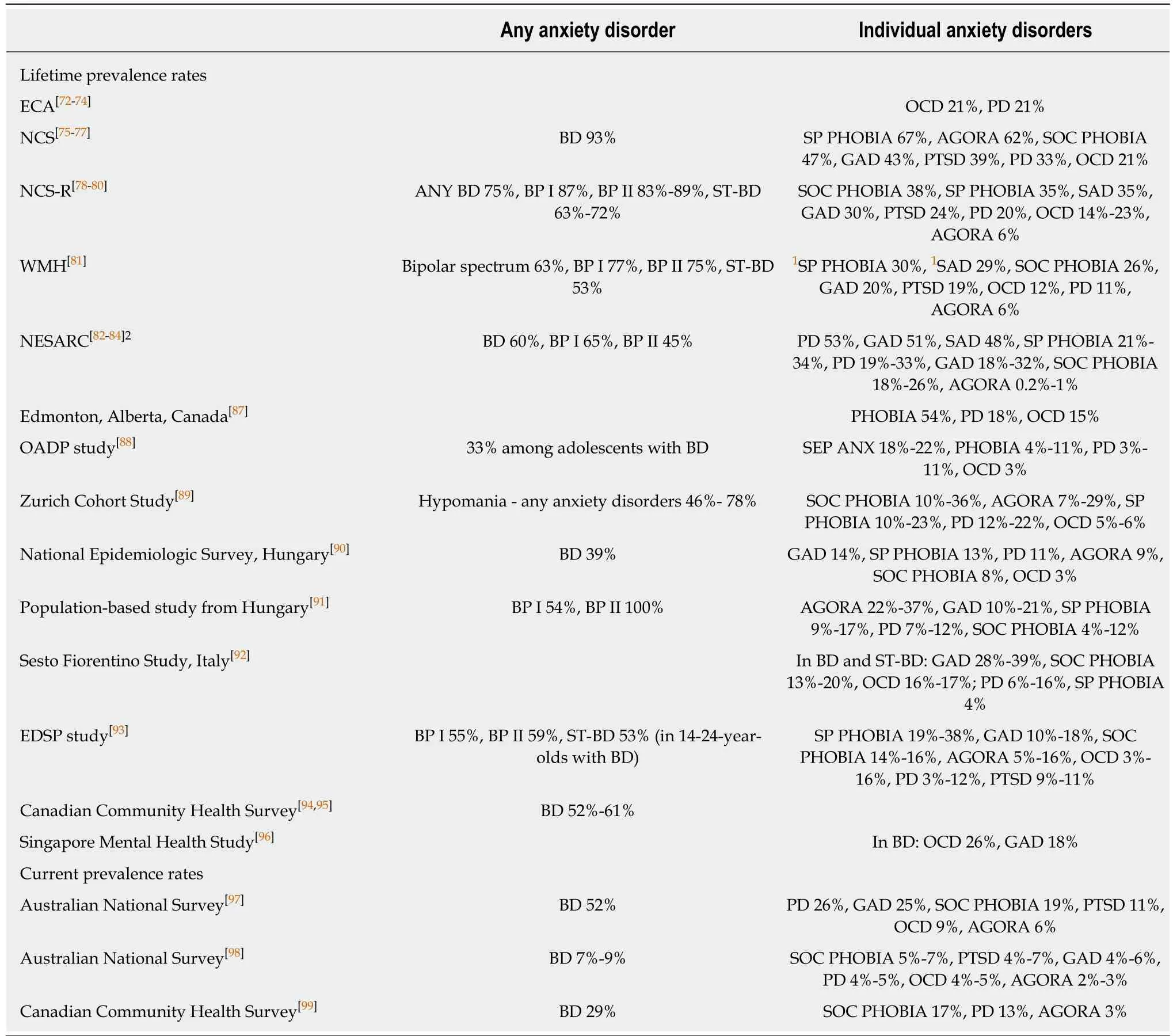
Table 3 Prevalence of anxiety disorder comorbidity in bipolar disorder: Evidence from epidemiological studies
Predominance of depression
A depressive onset, i.e. the first lifetime episode being a depressive one, has been reported more commonly among those with anxiety disorder comorbidity. Comorbid anxiety disorders have also been linked to more frequent and severe episodes of depression in BD. Impaired functioning, poor quality of life, and higher risk of suicide have been attributed to the predominance depressive pathology in comorbid anxiety disorders and BD[15,16,18,36,42]. In contrast, the relationship of this comorbidity with maniawas much less evident[8,14,16,18,36].
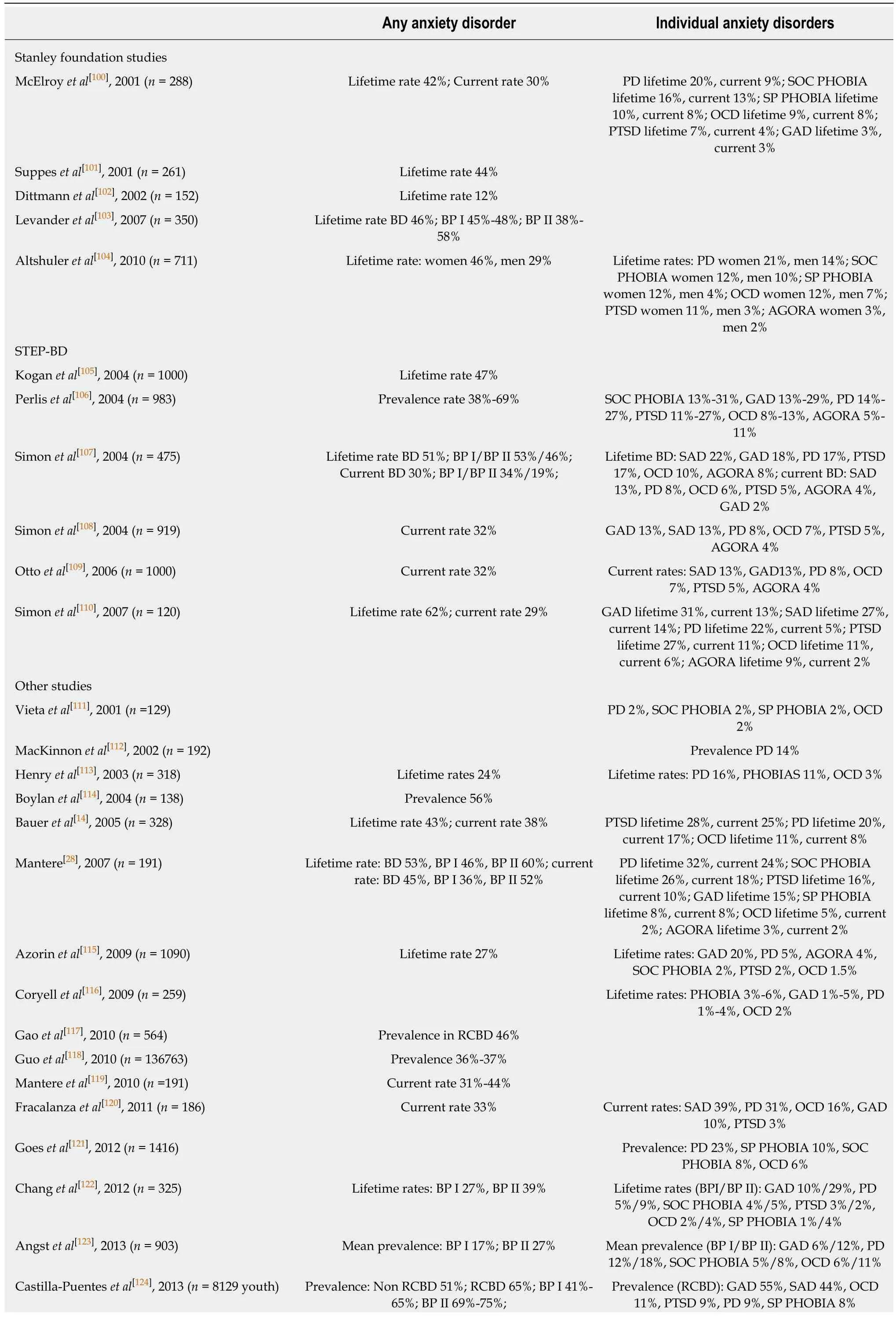
Table 4 Prevalence of anxiety disorder comorbidity in bipolar disorder: Evidence from selected large-scale clinical studies
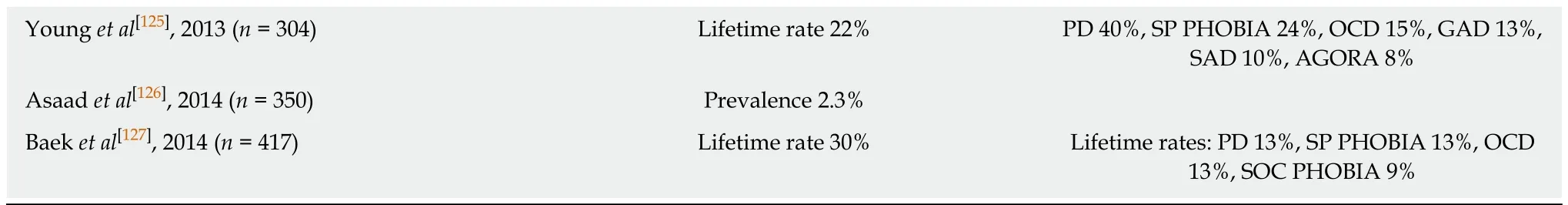
BD: Bipolar disorder; BP I: Bipolar disorder subtype I; BP II: Bipolar disorder subtype II; RCBD: Rapid cycling bipolar disorder; STEP-BD: Systematic Treatment Enhancement Program for Bipolar Disorder.
Other clinical features
Rapid cycling, mixed states or features, and psychotic symptoms are other clinical characteristics frequently associated with anxiety disorder comorbidity in BD[8,9,16,17,22].
Additional comorbidities
Among all comorbid conditions associated with anxiety disorder comorbidity in BD,the most common was substance use comorbidity. Patients with comorbid anxiety disorders and BD were twice as likely to have an additional diagnosis of SUD[9]. The high prevalence of comorbid SUDs in those with anxiety disorders and BD has been noted by a number of meta-analyses and systematic reviews[8,18,20,22,42]. It has been repeatedly documented by almost all major epidemiological studies[74,87,150,152,153], and by the Systematic Treatment Enhancement Program for Bipolar Disorder and Stanley Foundation studies, as well as other large-scale clinical studies of anxiety disorder comorbidity[14,52,100,114,117]. Conversely, only a few studies have been unable to find this relationship between anxiety disorders and SUDs in BD[9,28,113]. The presence of a combination of anxiety disorders and SUDs in BD not only complicates the diagnosis,but also impairs treatment response and can lead to a more severe course of illness and increased suicidal risk[10,17,27,69,154]. Apart from associated SUD comorbidity, anxiety disorders in BD have also been linked with other comorbid conditions such as attention deficit hyperkinetic disorders, eating disorders, and a range of personality disorders[9,14,18,22,42]. Rates of medical comorbidity were also greater in those with comorbid anxiety disorders and BD[155,156].
Bipolar subtypes
In contrast to other clinical correlates, findings regarding the association of anxiety disorder comorbidity with bipolar subtypes I and II have been equivocal and contradictory. While one meta-analysis found somewhat greater rates in patients with bipolar subtype II[20], others have either found a higher prevalence of anxiety disorders in bipolar subtype I[30,33], or more commonly, no significant differences between the two subtypes[18,19,32,36]. This inconsistent association between anxiety disorders and bipolar subtypes has also been found in other reviews[8,10,15-17], in epidemiological studies[78,81,82,84,91], and in clinical samples of patients with BD[52,100,120]. On the other hand,more than a few reviews have reported a considerably higher prevalence of bipolar spectrum disorders[7,42,46,66,128], sub-threshold BD, or subsyndromal bipolar symptoms[7,14,66,69,139]among comorbid anxiety and BDs.
IMPACT OF ANXIETY DISORDER COMORBIDITY IN BD
As is evident from Table 5, existing literature has been fairly consistent in reporting the widespread negative impact of anxiety disorder comorbidity among patients with BD on almost all aspects of the course and outcome of the illness.
Increased symptom-burden
The presence of anxiety disorders in BD has been linked with a marked increase in symptom-burden including increased psychological distress, increased irritability,greater severity of acute episodes, and greater burden of both manic and depressive symptoms.
Longer episodes
The greater severity of mood episodes in individuals with comorbid anxiety disorders is also reflected by the longer duration of these episodes, particularly depressive ones,and the higher rates of chronicity in BD with anxiety disorders.
Poorer remission and recovery
Patients with comorbid bipolar and anxiety disorders have been found to havesignificantly longer times to remission, less likelihood of achieving complete remission or recovery, persistence of subsyndromal symptoms, shorter durations of remission, greater risk of developing an early relapse or recurrence, and higher risk for hospitalizations.
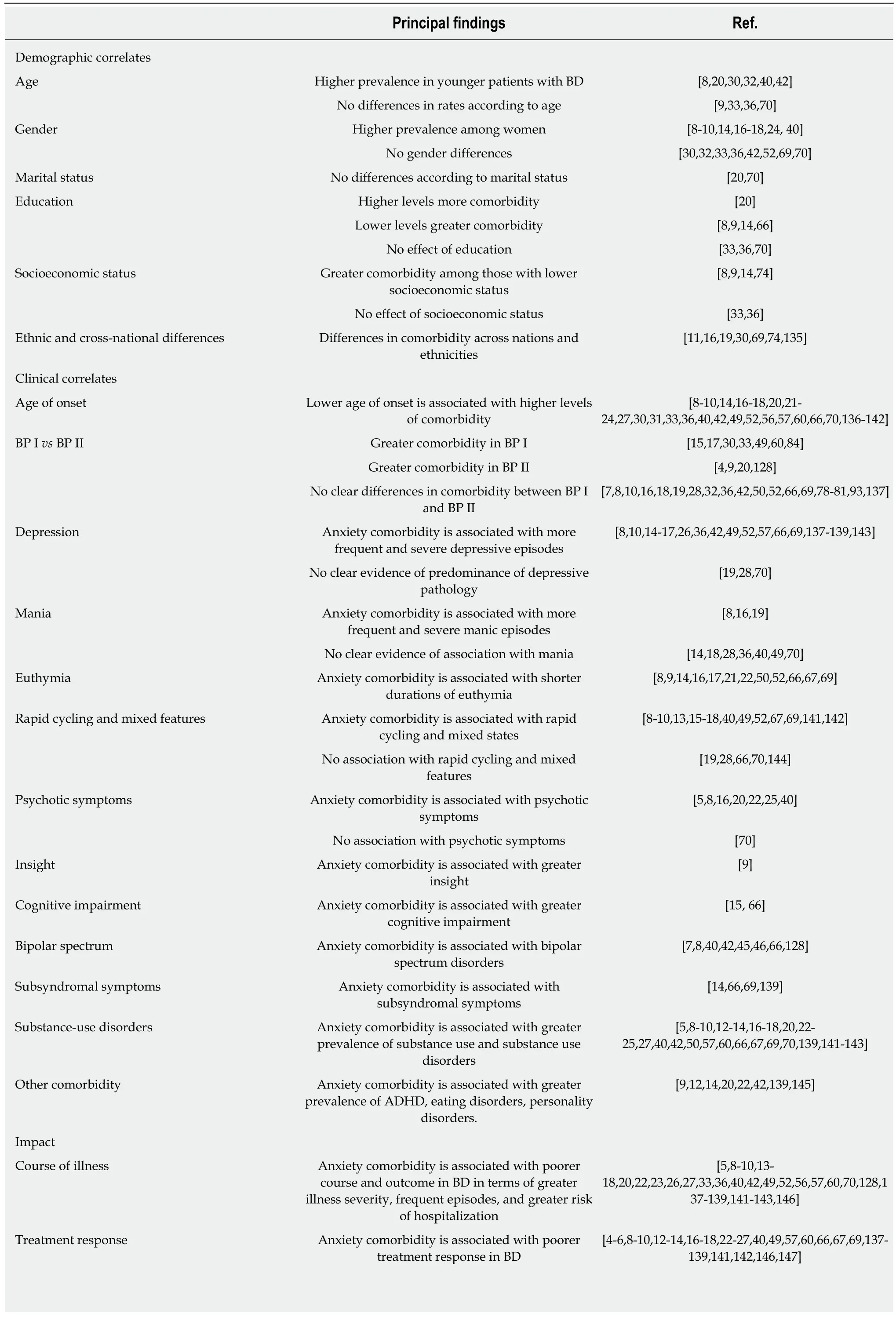
Table 5 Correlates and impact of anxiety disorder comorbidity in bipolar disorder
BD: Bipolar disorder; BP I: Bipolar disorder subtype I; BP II: Bipolar disorder subtype II; ADHD: Attention deficit hyperactivity disorder.
Impaired functioning and quality of life
Patients with comorbid anxiety disorders and BD have greater functional impairment and poorer quality of life than those without this comorbidity.
Inadequate treatment response
Many reviews and studies on anxiety disorder comorbidity in BD have also reported poorer treatment response, delayed diagnosis and institution of treatment, more severe medication side-effects, non-adherence with treatment, increased health-care utilization, and increased costs of care.
Elevated suicidal risk
A large meta-analysis of suicidal risk in BD found that comorbid anxiety disorders were strongly associated with suicide attempts with an odds ratio of two derived from eight studies[148]. Another systematic review also found an increased risk of suicidal behaviour among patients with comorbid panic disorders[149]. Similar increases in suicide risk have been reported among other comorbid anxiety disorders including GAD, PTSD, OCD, and social phobia[33,36,42,45,50]. The elevated risk of suicide has been proposed to be the result of increased illness severity, greater depressive symptom-burden, additional SUD comorbidity, the presence of comorbid personality disorders, and several maladaptive traits such as impulsivity or neuroticism[18,26,33,46,148].
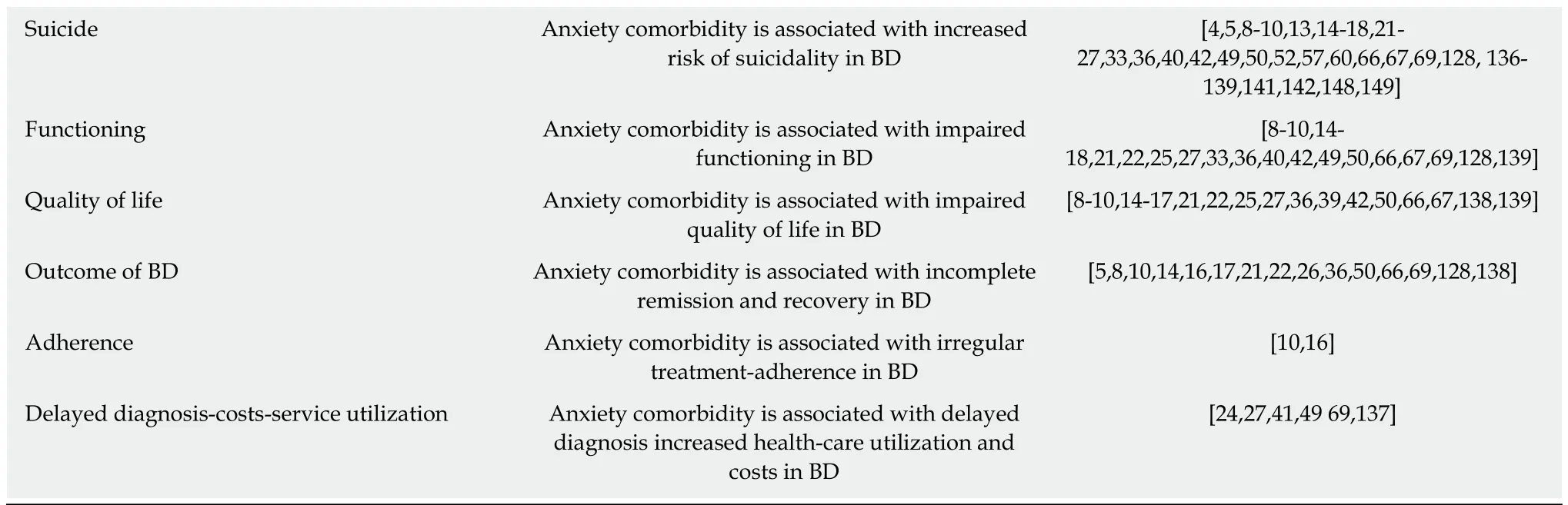
TREATMENT OF ANXIETY DISORDER COMORBIDITY IN BD
In contrast to the substantial data on rates, correlates, and impact of anxiety disorder comorbidity in BD, research on the efficacy of different modalities of treatment for comorbid anxiety disorders in BD has been rather scarce. Table 6 provides a brief summary of this research.
Treatment of anxiety comorbidity in BD is challenging because of inherent difficulties in diagnosing comorbid bipolar and anxiety disorders and the high prevalence of inadequate response to treatment[6,10,17,18,172]. Treatment options include both pharmacotherapy and psychotherapy. Only two randomized-controlled trials of medication treatment have been conducted in comorbid BD and anxiety disorders.One showed some efficacy for olanzapine and lamotrigine in treating anxiety symptoms[173], while the other failed to show similar efficacy for risperidone[174].Therefore, findings from treatment of bipolar depression have been extrapolated to provide the necessary evidence-base for pharmacotherapy of anxiety comorbidity in BD[10,26,15,17,162]. However, despite the lack of evidence there appeared to be considerable consensus that the primary aim of treatment is mood stabilization, although there was little agreement about the mood stabilizer of choice[6,7,9,10,162]. Following mood stabilization, treatment with other specific medications might be considered. Options include second-generation antipsychotics, specific serotonergic reuptake inhibitors,anticonvulsants, and benzodiazepines, though each medication group appears to have its advantages and disadvantages[6,10,15,17,162]. Although psychotherapy,particularly cognitive behavioural treatment is also recommended as a first-linetreatment option, the evidence base for cognitive behavioural treatment was meagre until recently[164]. However, lately several new randomized-controlled trials of cognitive behavioural treatment have demonstrated its efficacy in treating anxiety symptoms in BD, making it a legitimate option for concomitant treatment of anxiety disorders in BD[165,168-171].
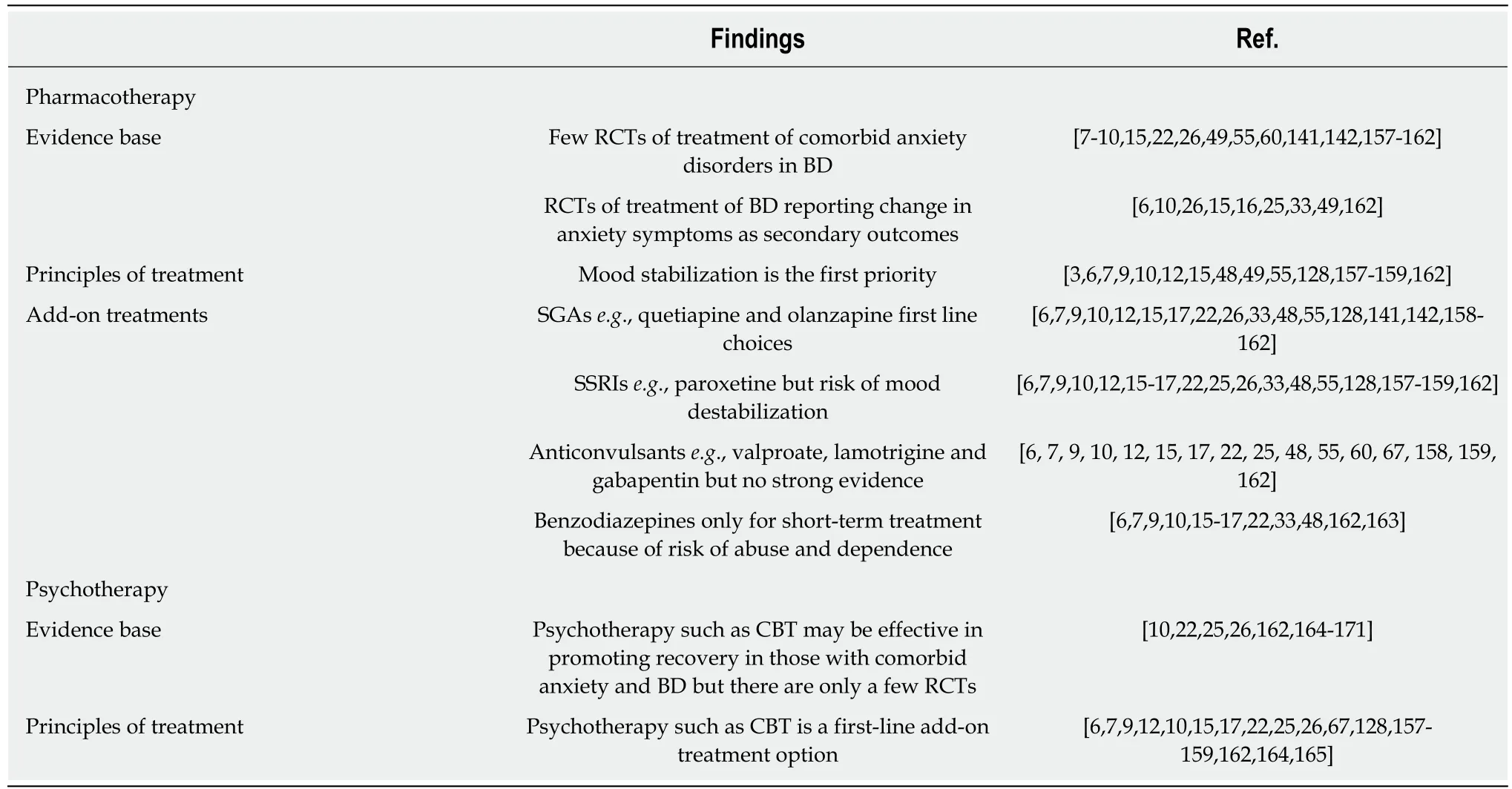
Table 6 Treatment of anxiety disorder comorbidity in bipolar disorder
AETIOLOGY OF ANXIETY DISORDER COMORBIDITY IN BD
Though there is no clarity regarding the aetiology of anxiety disorder comorbidity in BD, several lines of evidence have suggested that family genetics, neurobiology,trauma, and other psychosocial factors may be involved in the genesis of anxiety disorders in BD[6,20]. Different conceptual models have been proposed to explain the co-occurrence of anxiety disorders and BD[3,6,9,13,16]. The first model suggests that comorbid bipolar and anxiety disorders occur together simply by chance. However,the high rates of anxiety disorders in BD negate the possibility of a chance association.The second model suggests that a pathophysiological link between anxiety disorders and BD explains the high rates of anxiety disorder comorbidity in BD. Two possibilities exist within this conceptual model; either the anxiety disorder predisposes to the development of BD, or BD increases the chance of the anxiety disorder emerging. The first possibility is supported by studies indicating that anxiety disorders serve as prodromal conditions preceding the development of BD[7,11,45,175,176].The second possibility of BD contributing to emergence of anxiety disorders is indicated by the evidence suggesting that anxiety symptoms are an integral part of BD[6,8,16], by the episodic course of anxiety disorders in a subset of patients with BD and anxiety disorders[177], by familial genetic links between the two disorders[9,10,17,69,178],and by the benefits of mood stabilization as a primary mode of treatment[3,6,9,10]. The third model posits that higher-order pathophysiological mechanisms contribute to the onset of both anxiety disorders and BD. The list of such core pathophysiological processes includes familial genetic, neurobiological, and psychosocial factors. There is reasonable evidence suggesting genetic links between anxiety disorders and BD[69,130,157], particularly for panic disorder[53,57,112,128,179]and OCD[40,42,70,176,178].Neurotransmitter disturbances, structural and functional brain changes, and alterations of synaptic plasticity could also provide the common link[9,10,20,53,130].Psychosocial factors such as early childhood adversities, particularly trauma as an aetiological factor for comorbid PTSD, have also been implicated[9,10,17,39,50]. Finally, a fundamental disturbance in affective regulation, suggested by the presence of abnormal temperamental and personality characteristics among those with BD and comorbid anxiety disorders, is also a likely underlying mechanism[9,33,50,180].
UNIQUE FEATURES OF ANXIETY DISORDER COMORBIDITY IN BD
In their review of publication trends on the subject, Provencher et al[5]concluded that research on anxiety disorder comorbidity in BD, which had been expanding since the 1990s had almost stopped 20 years later. They also noted that the bulk of the publications were non-specific or descriptive in nature, with little research on causal mechanisms or management of this comorbidity. Similar apprehensions have been expressed by a number of other researchers[6,9,18,70,137]. The results of the current review,however, suggested that such concerns might only be partly true. The present review identified more than 100 prior reviews and over 350 studies on the subject. Therefore,the volume of extant research on this comorbidity was by no means inadequate and interest in the topic does not appear to be diminishing. Then again, the findings of the current review also showed that the majority of the research pertains to rates,correlates, and impact of comorbid anxiety disorders in BD, while research on treatment and aetiological processes is relatively limited.
The principal findings of this review were consonant with prior research in profiling the unique features of anxiety comorbidity in BD. The results reiterated the fact that at least half of those with BD are likely to develop an anxiety disorder in their lifetimes and a third of them will manifest an anxiety disorder at any point of time.The markedly elevated rates of anxiety disorders in BD were not only several fold higher than general population rates of anxiety disorders[18-20,23,35], but also higher than those found in unipolar disorders[6,13,15,20,43]and schizophrenia[181,182]. There was also some evidence, particularly from epidemiological studies, to indicate that anxiety disorders may be the most common comorbid conditions in BD and even more prevalent than comorbid SUDs[8,15,20,60,183]. Other notable characteristics included the coexistence of multiple anxiety disorders and additional comorbidities, especially the link with SUDs. The adverse clinical profile of comorbid bipolar and anxiety disorders as well as its association with poorer course and outcome, including the strong association with increased suicidality were additional distinctive features of anxiety disorder comorbidity in BD. Although these aspects of comorbid anxiety and BDs have been documented earlier, by collating findings from a larger and updated database the present review re-emphasized the significance and uniformity of these findings across multiple types of reports. Moreover, being based on more reliable sources of evidence it provided stronger endorsement for these unique attributes of comorbid anxiety disorders in BD.
LACUNAE IN EXISTING RESEARCH
Treatment and aetiological research
Although concomitant anxiety disorders have important implications for management of BD, evidence on this aspect was scarce. Additionally, the lack of research on aetiology of comorbid bipolar and anxiety disorders was also evident. The expectation that examination of this comorbidity would reveal the etiopathogenetic processes underlying BD has thus not been fully realized.
Methodological issues
Despite the sizeable body of evidence on anxiety disorder comorbidity in BD, metaanalytic reviews have indicated that only 50 studies or less are of sufficient methodological rigor[11,18,19,30,34]. The same meta-analyses have revealed significant heterogeneity in rates of anxiety disorders, while almost all the other reviews have also noted the wide variation in rates. Many potential sources of bias could account for this discrepancy across studies including the method of diagnostic ascertainment,the type of investigators employed, the source and nature of patient samples, study designs, and the type of rates used[11,15,16,26,27]. Notwithstanding these numerous methodological confounders, two meta-analyses have concluded that all these methodological variables did not fully explain the heterogeneity in rates across studies, suggesting that unknown and unexplored factors were possibly the chief sources of the differences found[19,35].
Conceptual issues
Although there is substantial evidence that anxiety disorder comorbidity is commonplace in BD, critics have proposed that some of this apparent comorbidity could be an artefact of current nosological systems and diagnostic practices[3,13,157,184,185].In medicine (from where the term comorbidity originates), Feinstein's definition specified that the two co-occurring disorders should be independent and distinct,presumably based on aetiological differences between the disorders[186]. This concept cannot be easily transposed to psychiatry because of the lack of knowledge about the causes of most psychiatric disorders and because of overlap in diagnostic criteria sets in current classifications[26,28,139,184]. Therefore, it remains uncertain whether this comorbidity is a product of two independent disorders, or of additive interactions between two coexisting disorders, or simply a part of the range of symptomatic expression of BD[11,18,22,26]. True comorbidity presupposes that the comorbid conditions will be fully diagnosable axis I or axis II disorders with minimal overlap in the content of their symptoms[1,3]. However, certain studies have moved beyond these precise definitions by including sub-threshold anxiety disorders or anxiety symptoms as a part of the anxiety disorder comorbidity of BD. This often leads to over-diagnosis and over-inflated rates of comorbidity[3,13]. Finally, a series of meta-analyses, systematic reviews, and studies of comorbid OCD in BD have found that spurious comorbidity,in which OCD was confined to the depressive episodes and disappeared during mania or remission, was present in nearly 50% to 75% of patients with BD-OCD comorbidity[30,32,42,68,177]. Truly comorbid OCD, where OC symptoms were not confined exclusively to mood episodes was less common. Unfortunately, there are very few longitudinal studies of BD, which could allow an accurate estimation of the rates of such true anxiety disorder comorbidity in BD.
LIMITATIONS OF THE PRESENT REVIEW
Though the current review was based on a reasonably comprehensive literature search, some sources especially those not in English may have been missed.Additionally, the present review relied mainly on results of prior meta-analyses and reviews, while it only included selected epidemiological and clinical studies. Thus,some findings from smaller studies might have been ignored. Moreover, it was difficult to know which source to trust when findings from the three sources were in conflict. However, an attempt was always made to present a balanced perspective by considering both the more dependable findings from research as well as the controversial ones.
CONCLUSIONS
Despite the deficiencies of research and limitations of the present review, it is quite clear that clinicians need to be fully aware of the substantial nature of anxiety disorder comorbidity in BD and its deleterious consequences, especially because it often goes unrecognized in routine clinical practice[9,12,33,46]. Such awareness is necessary for proper identification and accurate diagnosis of both BD and the anxiety disorder[3,6,9,15,19]. Firstly, patients with BD will need to be routinely screened for the presence of anxiety disorders; when detected a comprehensive and systematic assessment of the anxiety disorder comorbidity should be performed. Similarly,clinicians should examine patients presenting with anxiety disorders for the presence of comorbid BD[3,7,8,30,45]. Secondly, while managing anxiety disorder comorbidity in BD precedence is almost always given to adequate mood stabilization as the first step in treatment[3,6,7,9,10]. Following this, clinicians can either adopt a sequential or a hierarchical approach to treatment[3,10]. The hierarchical approach involves determining the primary condition and comprehensively managing it before focusing on the treatment of the secondary condition[3]. In the more commonly used sequential approach, after initial mood stabilization a stepped-care strategy may be employed in which pharmacological and psychosocial interventions can be added sequentially depending on the patient's treatment needs[3,10,164]. In either approach utmost caution must be exercised to prevent the treatment of one condition from adversely affecting the outcome of the other. The final component of management is regular monitoring and on-going treatment to prevent the long-term adverse consequences of this comorbidity[48].
For researchers there are many unresolved questions to answer including the significance of anxiety disorder comorbidity in BD, the nature of its underlying mechanisms, and the best possible ways to effectively manage this comorbidity[5,13,18,20,26]. The current investigative methodology needs to be improved by examining truly representative samples of patients, focusing on individual disorders as well as overall anxiety disorder comorbidity, and by longitudinal and more in-depth analyses of comorbid anxiety and BDs. However, since added efforts on the part of both clinicians as well as researchers are likely to alleviate the burden of anxiety comorbidity on patients with BD, they are worth pursuing.