Effective use of the Japan Narrow Band Imaging Expert Team classification based on diagnostic performance and confidence level
2019-03-16DaizenHirataHiroshiKashidaMineoIwatateTomomasaTochioAkiraTeramotoYasushiSanoMasatoshiKudo
Daizen Hirata,Hiroshi Kashida,Mineo Iwatate,Tomomasa Tochio,Akira Teramoto,Yasushi Sano,Masatoshi Kudo
Abstract
Key words:Japan Narrow Band Imaging Expert Team; Classification; Magnifying endoscopy; Narrow-band imaging; Validation; Diagnostic performance; Colonoscopy;Colorectal neoplasms
INTRODUCTION
The Sano classification was proposed as the first Narrow Band Imaging (NBI)classification in 2006[1]. Following this,three classifications were proposed in Japan[2-4].Colon Tumor NBI Interest Group proposed the Narrow Band Imaging International Colorectal Endoscopic (NICE) classification in 2009 (Figure1). The NICE classification is easily applicable and can be used without magnification. However,previous validation studies revealed two problems with the NICE classification. One was that the confidence rate was reported to be only 50%-75%[5,6]though the diagnostic performance was acceptable in cases with high confidence. This means that the amount of polyps that can be diagnosed by the NICE classification is not high enough.The other problem was that endoscopists could not differentiate malignant neoplasia[high grade intramucosal neoplasia (HGIN) and invasive cancer] from benign neoplasia [low grade intramucosal neoplasia (LGIN)] using the NICE classification.This differentiation is clinically valuable for deciding treatment options because the invasion depth of malignant neoplasia should be evaluated by the specimen obtained en-bloc by endoscopic mucosal resection (EMR) or endoscopic submucosal dissection(ESD). In 2014,the Japan Narrow Band Imaging Expert Team (JNET) classification was published and showed the NBI diagnosis with magnification had the potential to increase the confidence rate and enable endoscopists to differentiate malignant neoplasia from benign neoplasia[7,8].
The JNET classification consists of 4 categories; JNET type 1,type 2A,type 2B,and type 3. Each type represnts the histological features of the polyps,and they are categorized by focusing on two specific features,the vessel pattern and the surface pattern (Figure2). JNET type 1 refers to hyperplastic polyps and sessile serrated polyps. Type 2A refers to LGIN and type 2B corresponds to HGIN or shallow submucosal invasive cancer (S-SMC). Type 3 refers to deep submucosal invasive cancer (D-SMC).
The aim of this review is to reveal the diagnostic performance and the confidence level of the JNET classification. Since there were no previous studies concerning the diagnostic performance and the confidence level of the JNET classification,we analyzed them based on the study data compiled at Sano hospital.
In this review we evaluate the diagnostic performance of the JNET classification and its confidence level (high or low) based on data from the study conducted at Sano Hospital from March 2015 to September 2018,and also those from the systematic review carried out in Medical Literature Analysis and Retrieval System On-Line(MEDLINE) from January 2014 through March 2019.
OUR STUDY

Figure1 Narrow Band Imaging International Colorectal Endoscopic classification1.1Can be applied using colonoscopes with/ without optical (zoom)magnification. 2These structures (regular or irregular) may represent the pits and the epithelium of the crypt opening. 3In the WHO classification,sessile serrated polyp and sessile serrated adenoma are synonymous. 4Type 2 consists of Vienna classification types 3,4 and superficial 5 (all adenomas with either low or high grade dysplasia,or with superficial submucosal carcinoma). The presence of high grade dysplasia or superficial submucosal carcinoma may be suggested by an irregular vessel or surface pattern,and is often associated with atypical morphology. SSP:Sessile serrated polyp.
We investigated the diagnostic performance of the JNET classification including its confidence level (high or low) at Sano Hospital from March 2015 to September 2018.In this study,all colorectal polyps were diagnosed using the JNET classification before endoscopic resection or surgery. NBI magnifying observation was performed by 5 experts and 3 trainees. “High-confidence diagnosis” is defined as a diagnosis that the endoscopist has confidence of more than 90% probability. Both the endoscopic diagnosis and confidence level were recorded in real time during the colonoscopy,and the histopathological diagnosis was reported by an expert pathologist. We evaluated the relation between the JNET type,its confidence level,and the histopathological diagnosis for all polyps as the primary endpoint. The diagnostic performance and the high confidence rate were analyzed based on this data. We evaluated the diagnostic performance in differentiating “neoplasia (type 2A) from non-neoplasia (type 1)”,“Malignant neoplasia (type 2B,3)vsBenign neoplasia (type 2A)”,and “Deep submucosal invasive cancer (type 3) from other neoplasia (type 2A,2B)”.
LITERATURE SEARCH
For the purpose of this review,a systematic search was carried out in MEDLINE from January 2014 through March 2019. Keywords included “the Japan NBI Expert Team”or “JNET classification” by two endoscopists. Non-English articles were excluded.Fourteen articles were selected. Non-original articles were also excluded. The full texts of 12 original articles were reviewed. Articles about the diagnostic performance were included. Articles about other modalities and other issues such as study protocol and treatment were excluded. Finally,3 original articles were selected and included in this study (Figure3)[9-11].
DIAGNOSTIC PERFORMANCE WITH ITS CONFIDENCE LEVEL IN OUR STUDY
The authors examined 6138 colorectal polyps which were diagnosed using the JNET classification before endoscopic resection or surgery from March 2015 to September 2018. The histopathological diagnosis of the 6138 polyps were 979 hyperplastic polyps,244 sessile serrated polyps,4642 LGIN,214 HGIN or S-SMC,and 59 D-SMC.Five thousand six hundred twenty-four polyps were diagnosed with high confidence.The high confidence rate was 91.6%. The relation between the JNET classification(with or without confidence level) and the histopathological diagnosis is shown in Table1. Rate of correspondence between each JNET type and the histopathological diagnosis was 85.4%.
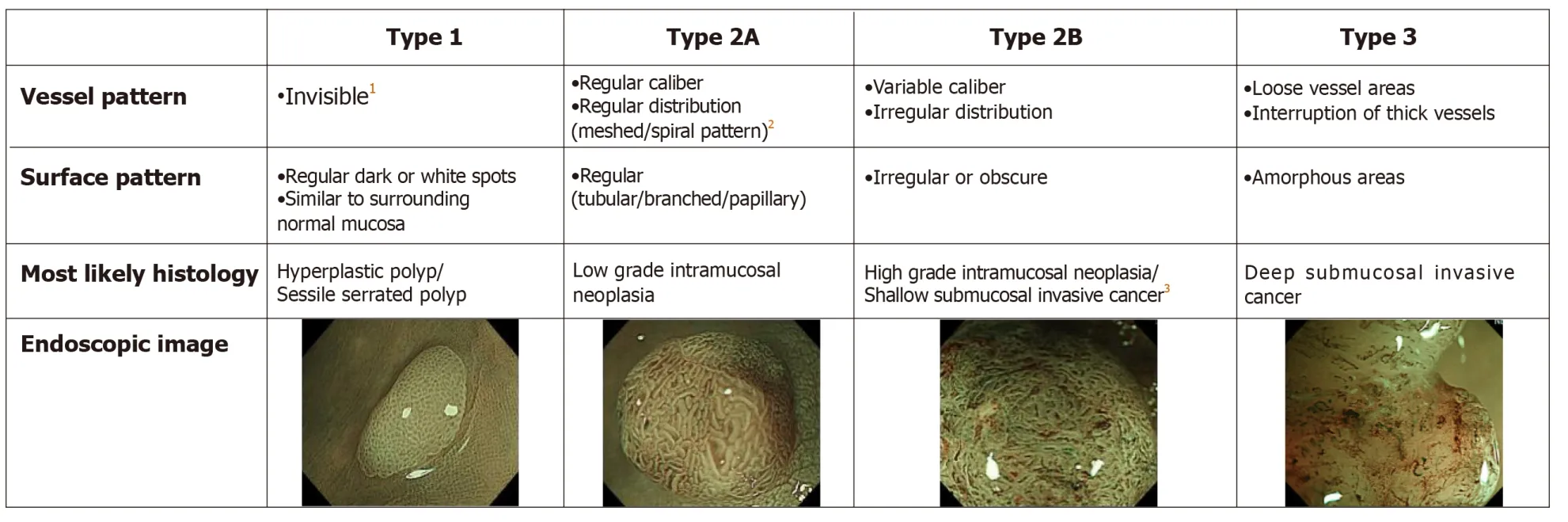
Figure2 The Japan Narrow Band Imaging Expert Team classification.1If visible,the caliber in the lesion is similar to surrounding normal mucosa. 2Micro-vessels are often distributed in a punctate pattern and well-ordered reticular or spiral vessels may not be observed in depressed lesions. 3Deep submucosal invasive cancer may be included.
PREVIOUS REPORTS ABOUT THE DIAGNOSTIC PERFORMANCE OF THE JAPAN NARROW BAND IMAGING EXPERT TEAM CLASSIFICATION
Three articles about the diagnostic performance were reviewed in this study. These articles and our study are summarized in Table2[9-11].
Sumimotoet al[9]conducted a retrospective analysis of 2933 colorectal lesions (136 hyperplastic polyps/sessile serrated polyps,1926 LGIN,571 HGIN,87 S-SMC,and 213 D-SMC). The accuracy of type 1,2A,2B,and 3 were 99.3%,77.1%,78.1%,and 96.6% respectively.
Komedaet al[10]performed a retrospective image evaluation study in 199 colorectal lesions (14 hyperplastic polyps/sessile serrated polyps,127 LGIN,22 HGIN,19 SSMC,and 17 D-SMC). The accuracy of type 1,2A,2B,and 3 were 98.5%,90.9%,87.4%,and 94.0%,respectively. They also analyzed of the relation between the macroscopic type and the diagnostic performance. They concluded that the JNET classification was useful for the diagnosis of hyperplastic polyps,sessile serrated polyps,LGIN,HGIIN and D-SMC,but not S-SMC.
Minodaet al[11]conducted a retrospective image evaluation study of 40 colorectal lesions involving 22 doctors (11experts and 11 non-gastrointestinal trainees). The average diagnostic accuracy was 76.6% for the experts and 61.4% for the trainees,though the relation between the JNET classification and the histopathological diagnosis was not disclosed. They concluded that the JNET classification was useful for differentiating malignant polyps from benign ones for every doctor. They also revealed orientation and training were necessary to use this system adequately even for experienced colonoscopists.
THE DIAGNOSTIC PERFORMANCE OF THE JAPAN NARROW BAND IMAGING EXPERT TEAM CLASSIFICATION
The diagnostic performance is important in determining the treatment strategy. In particular,the three differentiations:neoplasia (type 2A)vsnon neoplasia (type 1),malignant neoplasia (type 2B,3)vsbenign neoplasia (type 2A),and deep submucosal invasive cancer (type 3) from other neoplasia (type 2A,2B). The details of each diagnostic performance are shown in Table3-5. We analyzed the diagnostic performance for each differentiation in our study and the previous reports. Minoda’s report was excluded in these analyses,since necessary details and relations were not disclosed.
Neoplasia (type 2A) vs non neoplasia (type 1)
The diagnostic performance in differentiating neoplasia (type 2A) from non-neoplasia(type 1) is directly associated with the necessity of endoscopic treatment. Type 2A polyps should be resected by polypectomy. However,it is usually not necessary to resect type1 polyps. The sensitivity,the accuracy and the negative predictive value(NPV) were 98.1%-99.8%,88.8%-99.0%,and 88.9%-99.1%,respectively. According to this classification,endoscopists can identify almost all neoplasia.
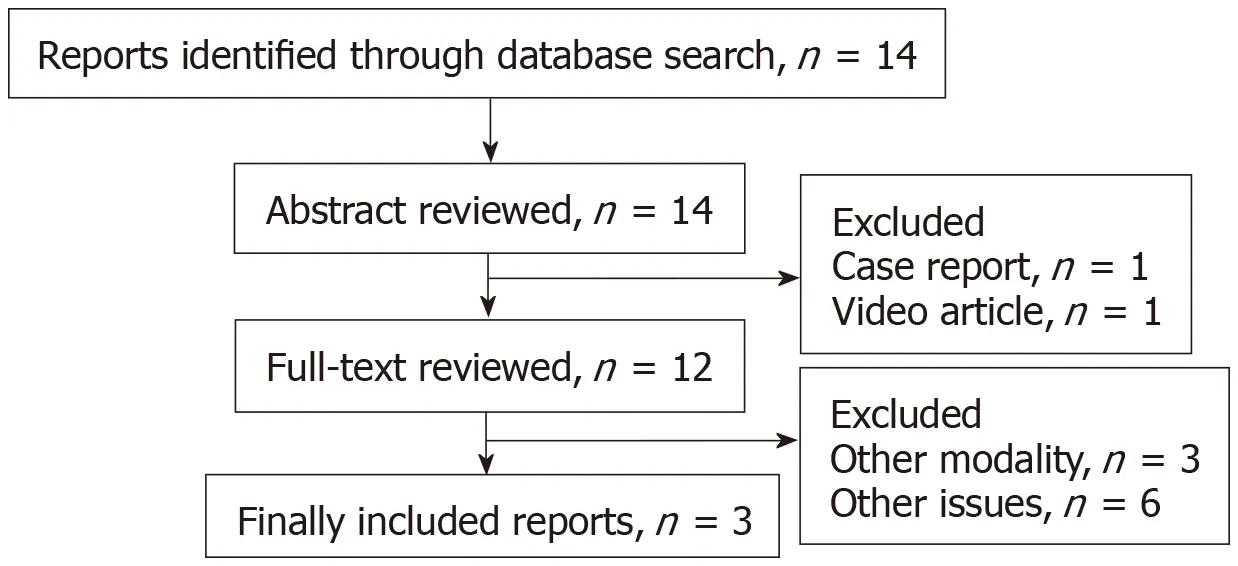
Figure3 Flow diagram of study selection.
In high confidence cases,counting 93.1% among all polpys,they were high enough to enable “Detect InSpect ChAractrise Resect and Discard strategy”,according to“Preservation and incorporation of valuable endoscopic innovations initiative” from American Society For Gastrointestinal Endoscopy[12,13].
Malignant neoplasia (type 2B,3) vs benign neoplasia (type 2A)
The diagnostic performance in differentiating malignant neoplasia from benign neoplasia is associated with the necessity of en bloc resection. While type 2A polyps can be treated by piecemeal EMR or polypectomy,type 2B polyps should be resected en bloc to obtain a precise histologic diagnosis from the specimen. The accuracy,specificity,and NPV of this diagnosis are 80.7%-96.1%,84.7%-98.2%,and 87.0%-97.7%,respectively. This is considered beneficial in diagnosing polyps as malignant neoplasm. By using the JNET classification,endoscopist can appropriately determine whether to perform en bloc resection or not.
Deep submucosal invasive cancer (type 3) from other neoplasia (type 2A,2B)
The diagnostic performance in differentiating deep submucosal invasive cancer from other neoplasia is associated with the necessity of surgical resection. As for this distinction,the specificity was extremely high being 99.8%-100.0%. The JNET classification enables endoscopists to avoid unnecessary surgery for non-invasive neoplasia. In our study,the unnecessary surgeries were only two cases. On the other hand,10.6%-23.9% of type 2B lesions were D-SMCs,and 0.0%-5.1% of type 3 lesions were S-SMCs. Additional magnifying chromoendoscopy is recommended in cases where it is difficult to differentiate between shallow and deep submucosal invasive cancers.
DISCUSSION
This is the first review concerning the diagnostic performance of the JNET classification taking account of the confidence level. Based on this review,we propose treatment strategy for colorectal localized lesions using the JNET classification with its confidence level (Figure4).
Type 1 polyps generally do not need resection except for sessile serrated polyps[14].Type 2A polyps shall be resected by polypectomy or EMR. Utsumiet al[15]reported that additional chromoendoscopy in type 1 and 2A polyps with low confidence prediction did not improve accuracy enough. Therefore,additional chromoendoscopy is considered to be unnecessary in order to differentiate type from type 1.
Whereas type 2A polyps can be resected by piecemeal EMR,type 2B polyps should be resected en bloc by EMR or ESD to obtain a precise histologic diagnosis concerning the invasion depth and determining endoscopic curability. Our review revealed the usefulness of the JNET classification,in that it accurately differentiated malignant polyps (type 2B,3) from benign (type 2A). It should be noted that 37.3%-70.6% of deep submucosal invasive cancers showed type 2B findings,magnifying chromoendoscopy is recommended before high-risk endoscopic resection for deep submucosal invasive cancer in type 2B polyps,if it is available. Type 3 lesions were diagnosed to be D-SMC with more than 99% specificity in our review,and therefore they are indicated for surgical resection.
The JNET classification is considered to have as high diagnostic performance as the NICE classification. However,there have been no studies directly comparing the JNET classification with the NICE classification. For comparison with the NICE classification,we evaluated the diagnostic performance with high confidence prediction and the high confidence rate in regards to two differentiations; “Neoplasiavsnon neoplasia” and “Deep submucosal invasive cancervsother neoplasia” (Table6). In both differentiations,the high confidence rate in the JNET classification was significantly higher than that of the NICE classification. It may demonstrate the JNET classification is clearer and easier to use than the NICE classification for the endoscopists. Magnifying observation may increase the high confidence rate of endoscopic diagnosis.
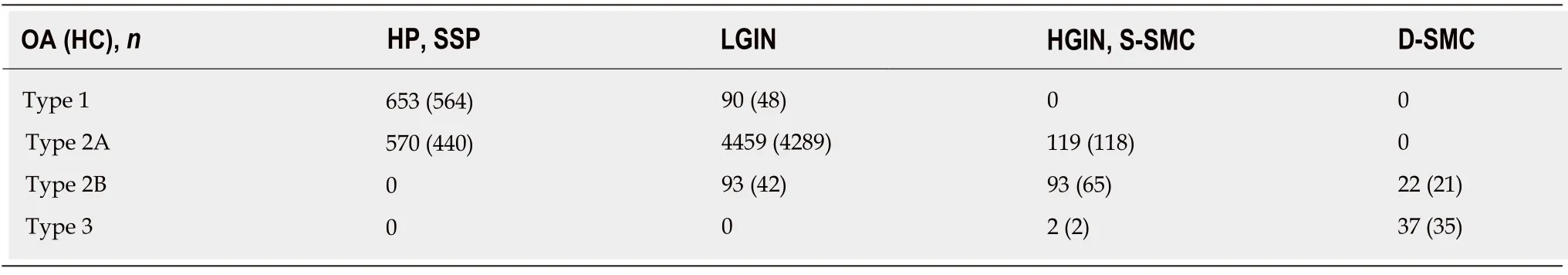
Table1 The relation between the Japan Narrow Band Imaging Expert Team classification and the histopathological diagnosis at Sano Hospital
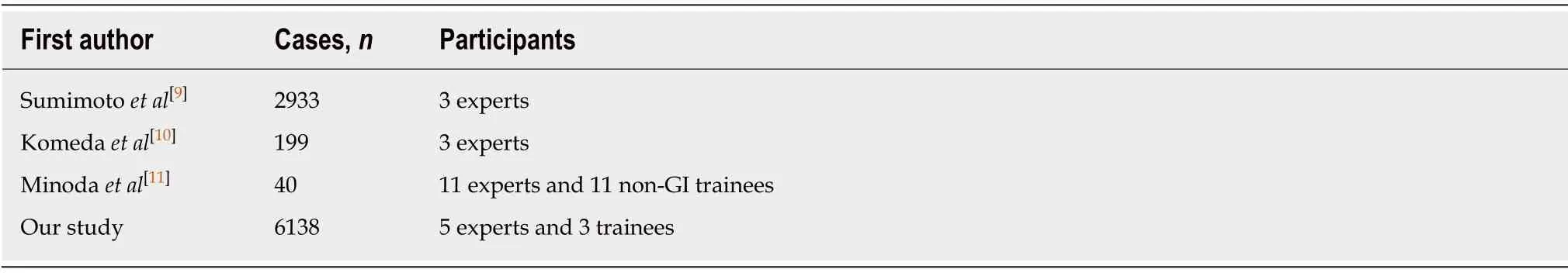
Table2 Reports about diagnostic performance of the Japan Narrow Band Imaging Expert Team Classification
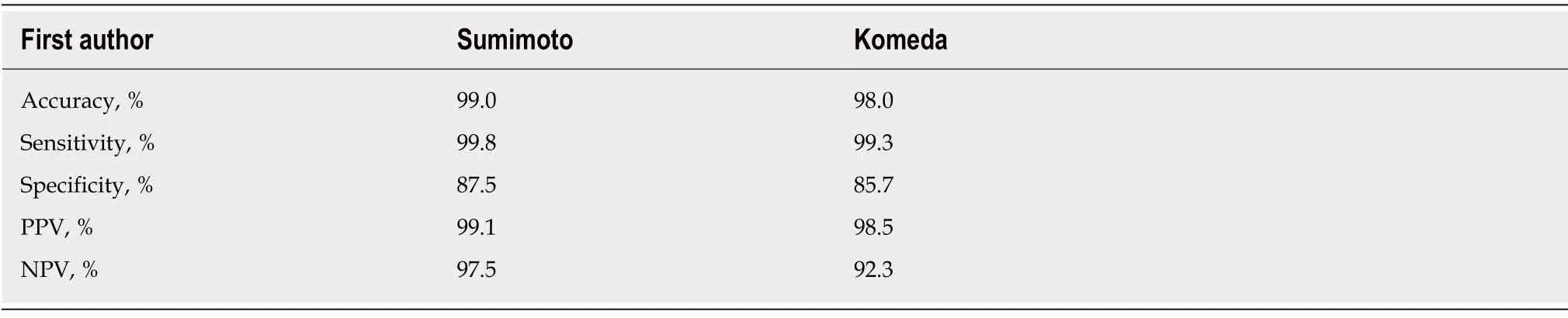
Table3 Neoplasia (type 2A) vs non neoplasia (type 1)
The JNET classification is compatible with the NICE classification in that both classifications are divided into three major categories (type 1,2,and 3) corresponding to the similar histopathology. The NICE type 2 corresponds approximately to the JNET type 2A and type 2B. Thanks to this similarity,endoscopists using the NICE classification should be able to use the JNET classification easily. A video article explaining typical examples and key points will help to adopt the JNET classification[16].
The limitation in this review is that there were only 3 articles about the diagnostic performance of the JNET classification. The previous studies were all retrospective single center studies. A large-scale prospective multicenter validation study of the JNET classification is awaited in the future. About the comparison the JNET classification with the NICE classification,though it is better to compare in the same endoscopic and histopathologic center,we did not such a comparative trial yet.
We predict that the JNET classification will provide endoscopists with a useful treatment strategy based on precise histopathological predictions and a higher confidence level for optical diagnosis.
CONCLUSION
The JNET classification enables endoscopists to identify almost all neoplasia,to appropriately determine whether to perform en bloc resection or not,and to avoid unnecessary surgery.

Table4 Malignant neoplasia (type 2B,3) vs benign neoplasia (type 2A)
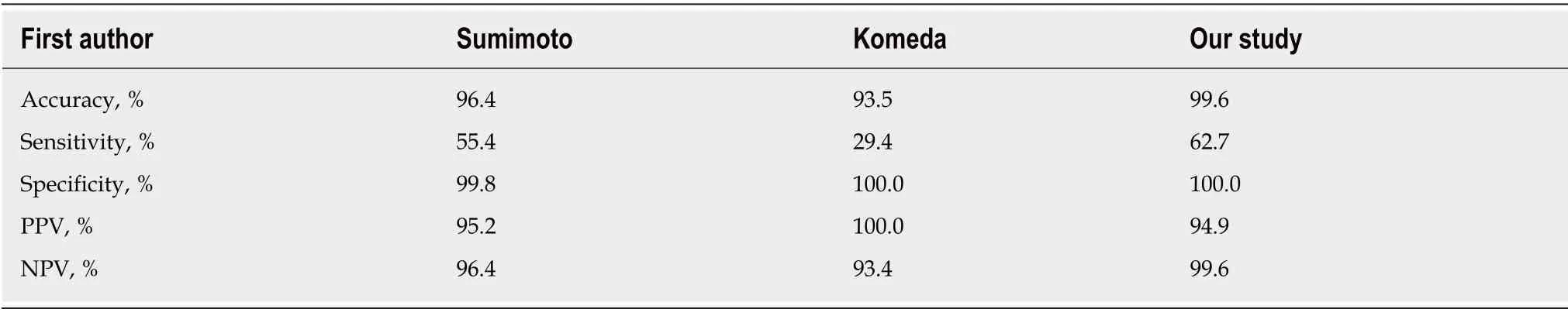
Table5 Deep submucosal invasive cancer (type 3) vs other neoplasia (type 2A,2B)
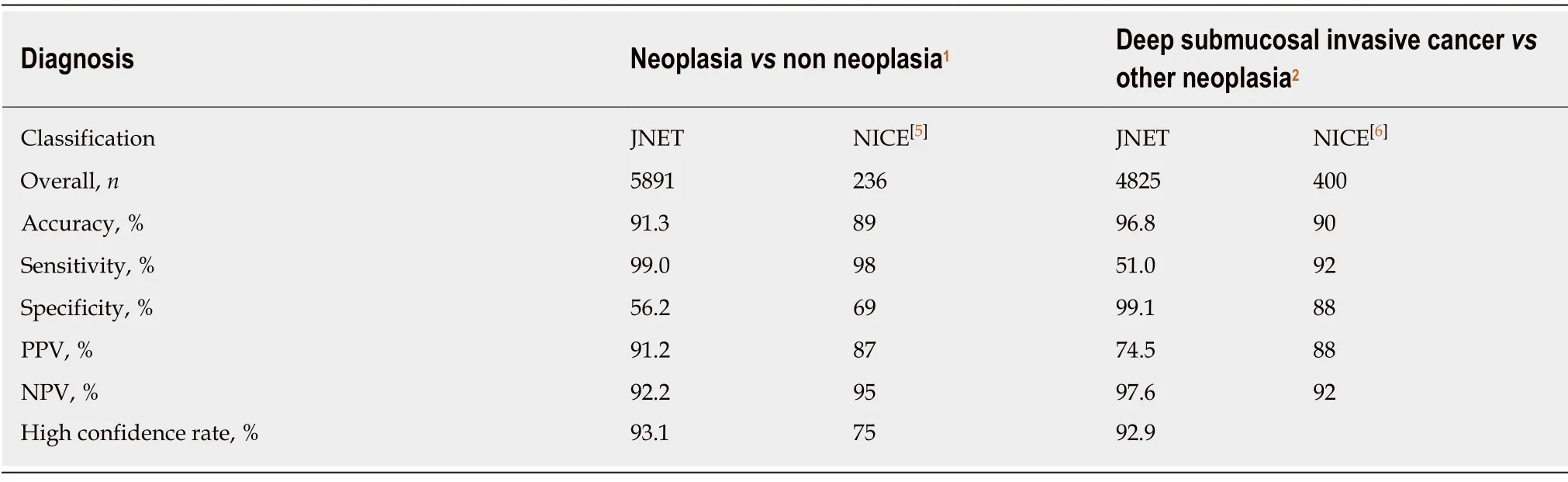
Table6 Comparison with Narrow Band Imaging International Colorectal Endoscopic classification
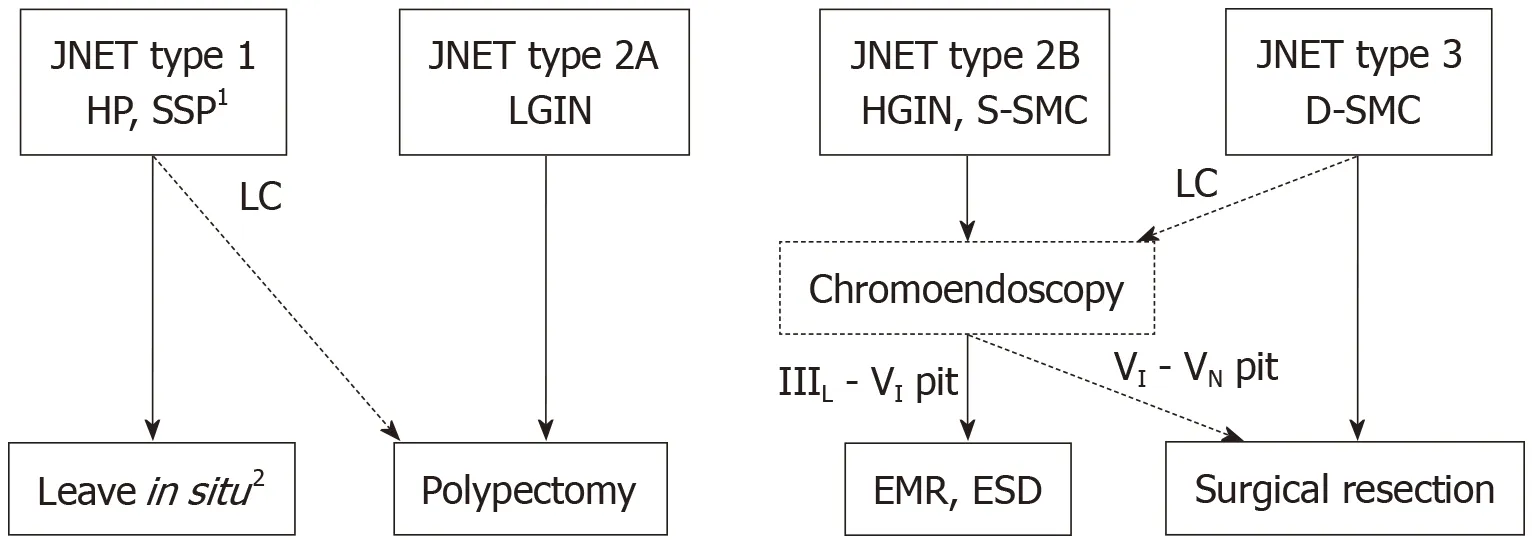
Figure4 Treatment strategy of colorectal lesions using the Japan Narrow Band Imaging Expert Team classification.1Any polyps suspected of SSPs should be resected by endoscopic treatment. 2Hyperplastic polyps less than 5mm in size are commonly left in situ. HP:Hyperplastic polyp; SSP:Sessile serrated polyp;LGIN:Low grade intramucosal neoplasia; HGIN:High grade intramucosal neoplasia; S-SMC:Shallow submucosal invasive cancer; D-SMC:Deep submucosal invasive cancer; LC:Low confidence.