Peroneus longus tendon rupture: A case report
2019-02-20DonKohLincolnLiowJosephCheahKevinKoo
Don Koh, Lincoln Liow, Joseph Cheah, Kevin Koo
Abstract BACKGROUND Peroneal tendinopathies are an under-diagnosed and potentially under-treated pathology. If left untreated it can be a cause of chronic lateral hindfoot pain. Its diagnosis is challenging owing to its low incidence and vague clinical presentation.CASE SUMMARY We share a case of a patient who experienced a chronic lateral ankle pain exacerbated after alighting from a bus. This patient came to our attention only after failing conservative management on two separate occasions. Plain radiographs and magnetic resonance imaging revealed rupture of the peroneus longus tendon (PLT). Findings were confirmed intra-operatively and tenodesis of the PLT to the peroneus brevis was performed. Patient was kept non-weight-bear with his foot everted and in plantarflexion before being converted to an offloading boot at two weeks. Patient was started on a progressive rehabilitation programme at six weeks and was able to return to work shortly after with excellent outcomes.CONCLUSION We aim to share our experience in managing this patient and propose some pointers guided by available literature to avoid missing this commonly overlooked pathology.
Key words: Chronic lateral ankle pain; Peroneus longus rupture; Peroneal tendinopathy;Tenodesis; Diagnostic challenge; Case report
INTRODUCTION
Ruptures of the peroneus longus tendon (PLT) are rare. The mechanism of injury is due to a combination of mechanical and anatomical factors. The peroneus longus undertakes a tortuous course from its origin at the proximal tibia and fibula to its insertion at the first metatarsal and medial cuneiform. The tendon travels within the posterior fibula groove, passes under the peroneal tubercle of the calcaneus and bends sharply along the cuboid groove before inserting medially at the base of the first metatarsal. These sites are potential sources of attrition[1]and avascularity[2-4].Incompetence of the superior peroneal retinaculum over the fibula groove can predispose PLT subluxation[1,3]. Varus deformities of the hindfoot or lateral ankle ligamentous laxity can subject the PLT to increased tension and frictional forces at transitional points described above[3]. In addition, anatomical variability such as the presence of an os peroneum in approximately 20% of the population may predispose to PLT rupture[5-9].
PLT pathologies can present acutely or insidiously, typically presenting with chronic pain. Patients who are able to relate an initiating injury are defined as acute;whilst patients who were unable to are classified as chronic[6,10]. Non-surgical management rarely yield acceptable outcomes[11,12]. Due to the PLT’s role in mid and hindfoot stability, surgical correction is often warranted with most authors achieving reproducible results. Timely intervention yields best results[6,10].
Its incidence remains ill-defined and the condition has only been described in case series or cadaveric studies. Dombek et al[12]documented 5 cases of isolated peroneus longus tears in their series of 40 patients with peroneus tendon pathologies. In contrast, Sobel et al[13]did not report any PLT ruptures in a cadaveric study of 124 ankles. Due its low incidence, peroneus tendon pathologies are often overlooked and often misdiagnosed. The duration between injury and diagnosis of PLT tear ranges from 6 to 48 mo[6,10,12]. In addition, the ambiguity of its symptoms makes PLT pathologies a diagnostic challenge. In the largest retrospective study available, only 60% of peroneal tendon injuries were accurately diagnosed on initial consult[12].Prudent history-taking, adequate examination and appropriate investigations cannot be overemphasized. We aim to share our experience managing a case of PLT rupture and strive to highlight the diagnostic challenges involved in this unique case.
CASE PRESENTATION
Chief complaints
A 51-year-old male flight attendant complained of chronic lateral ankle pain without prior trauma or twisting injury.
History of present illness
Three-month history of left lateral ankle pain. He sought treatment at other Orthopaedic centres but failed conservative management on two separate occasion.He subsequently presented to our care after he exacerbated his lateral ankle pain and heard a “click” whilst alighting from a bus. He denied any traumatic or inversion injury.
History of past illness
Known history of gout and previous left total hip replacement secondary to left hip avascular necrosis.
Personal and family history
None.
Physical examination
On clinical examination, he presented with an antalgic gait, swelling and tenderness over the posterolateral hindfoot. He demonstrated weakness in eversion
Laboratory examination
Not performed.
Imaging examination
Radiograph of the left foot showed a proximally displaced os peroneum compared to contralateral foot (Figures 1 and 2). Peroneal tendon pathology was suspected and magnetic resonance imaging (MRI) of the left foot revealed a full-thickness rupture of the PLT distal to the os peroneum with underlying tenosynovitis (Figure 3).
FINAL DIAGNOSIS
Full-thickness rupture of the PLT with underlying tenosynovitis.
TREATMENT
Surgical repair of the PLT was performed 4 wk after injury. Patient was positioned lateral with a thigh tourniquet applied. Incision was centred over the os peroneum and made from the left fibula tip to the base of the fifth metatarsal (Figure 4). The os peroneum was identified and excised. Unhealthy portions of the PLT and devitalised synovium were debrided. Proximal and distal ends of the PLT was mobilised and the defect was measured (Figure 4F). During surgery, a 1.5 cm longitudinal split of the peroneus brevis was noted and was repaired via tubularisation using vicryl sutures(Figure 4G). Side-to-side tenodesis of the PLT to the peroneus brevis tendon was performed using size 2-0 braided polyethylene sutures (ULTRABRAID Suture, Smith and Nephew, York, United Kingdom). The wound was irrigated with normal saline and hemostasis was performed. Layered closure was performed and a backslab was applied over the operated foot, keeping it in plantarflexion and eversion.
OUTCOME AND FOLLOW-UP
Patient was discharged on post-operative day one and was kept non-weight bear on the operated leg. Follow up was done in the outpatient setting at two weeks and six weeks post-operatively. At two weeks, the wound was inspected, skin sutures removed. The backslab was converted to a tall-aircast with heel wedges for the next four weeks and the patient was allowed to perform partial weight-bearing. At six weeks after surgery, patient was allowed full weight-bearing on the aircast and started on a rehabilitation programme aimed at improving range of motion and strength through stretching and isometric exercises.
At three months after surgery, patient demonstrated excellent clinical outcomes(Table 1) with significant improvements in American Orthopedic Foot and Ankle Score, visual analogue pain score as well as the Physical Component Score. He was allowed full weight bearing on normal footwear and returned to ground duties at the airport. At 6 mo, he had returned to sport and was allowed to return to flying duties.This patient continued to demonstrate excellent clinical outcomes at 12 mo post op(Table 1).
DISCUSSION
In a patient with posterolateral hindfoot tenderness and swelling refractory to conservative management, peroneal tendon pathology should be considered. A thorough history detailing the initial injury, exacerbating symptoms, evidence of instability or clicking should be elicited. Associated conditions such as rheumatoid arthritis, neuropathies, gout, local steroid injections and known ankle pathologies(e.g., enlarged peroneal tubercle) can predispose peroneal tendinopathy[14-18].
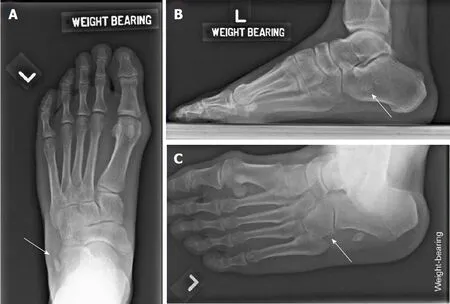
Figure 1 Initial weight bearing radiographs of the injured foot.
The presence of cavovarus or hindfoot varus may increase peroneal tendon tension and increase risk of rupture due to the unopposed action of the posterior tibialis.Physical examination, in particular, palpation should be focused along the course of the peroneal tendons. Common sites of discomfort and swelling include posterolateral hindfoot, cuboid groove and insertion site over at the plantar and medial aspect of the foot[3]. Eversion weakness should increase clinical suspicion of PLT pathology as the peroneal tendons contributes to 63% of eversion strength - with the peroneus longus contributing more than peroneus brevis[19]. However, it must be noted that the absence of weakness doesn’t preclude peroneal tendinopathy. Tenderness on active eversion,passive inversion or during plantarflexion of first ray may also suggest peroneal tendinopathy with the latter specific for the peroneus longus. Lateral ankle ligamentous laxity should also be assessed to rule out concomitant anterior-talofibular ligament (ATFL) incompetence.
Despite having a known history of gout, our patient did not require pharmacological control for his condition and denied any previous local steroid injections. Extra-articular tophaceous gout can predispose to PLT tendinopathy but rarely involves peroneal tendons. To date, there have only been two documented cases of PLT tendinopathy secondary to gout. De Yoe et al[17]described a patient with peroneus brevis tendon rupture and ATFL attenuation secondary to gouty infiltration.Radice et al[16]reported longitudinal tears of both peroneus longus and brevis tendons caused by urate crystal deposition. In our patient, intra-operative findings revealed no gouty infiltration.
Imaging investigations should be guided by clinical findings. Appropriate initial investigations involves weight-bearing anteroposterior, lateral and oblique views of affected foot (Figure 1). Although not routinely performed, the contralateral foot should be imaged in suspected PLT pathologies as it will be helpful in detecting subtle anatomical differences (Figure 2). In our patient, fracture of the os peroneum resulting in proximal migration of the os is pathognomonic of PLT ruptures. This is best seen on oblique and lateral views. There are numerous cases documenting the association of an os peroneum with PLT tears[5-9]. Some authors however disagree,reporting the lack of association in their series[3,6]. In addition, the oblique foot view also enables assessment of the peroneal tubercle. Enlargement of the peroneal tubercle alters biomechanics of the peroneus longus and is associated with tears of the PLT[20,21].In our patient, the peroneal tubercle was not enlarged.
Ultrasound of the peroneal tendons allow for dynamic assessment, particularly useful in examining peroneal tendon subluxation. It has been shown to provide 90%to 94% diagnostic accuracy of peroneal tendon tears with excellent sensitivity and specificity[22,23]. MRI is also widely employed, especially since the clinical presentation of PLT can be difficult to diagnose initially[6]. T2-weighted images allow detection of tendinosis or oedema within the tendons. However, there are a high rate of false positives and false negatives attributed to signal artefacts[10,24,25]. O’Neil et al[26]believes that the magic angle effect takes place as the PLT curves postero-inferiorly around the lateral malleolus - mitigatable through plantarflexion of the foot[26].

Figure 2 Comparing radiographs of bilateral oblique foot views.
In minimally symptomatic patients without ankle instability or loss of function, a trial of conservative management can be offered. Non-surgical treatment protocols are poorly defined but consist of non-steroidal anti-inflammatory medication, rest,orthosis or immobilisation with a short leg cast. Graded rehabilitation programs aiming to increase flexibility and strength are normally started two to four weeks post-immobilisation[6,19]. Outcomes with non-surgical management remains poor -especially for PLT ruptures[6,25]. In a series involving 40 patients with peroneal tendon tears, 36 patients reported undergoing unsuccessful non-surgical treatment[12].
Surgery is the mainstay of treatment for PLT ruptures. Sammarco proposed surgery when a trial of non-operative management has been unsuccessful or when an unstable or varus foot is noted. In the presence of an os peroneum, excision is indicated before repair is attempted. In the absence of an os peroneum, an MRI is indicated to identify cause of rupture or concomitant ligamentous or bony injuries[6].
Redfern and Myerson’s algorithm of treatment considers the condition of the peroneus brevis[25]. Type I lesions occur when both tendons appear grossly intact;Type II lesions on the other hand occurs when one tendon is torn, whilst the other tendon remains intact and finally Type III lesions occur when both tendons are torn.In the case of a PLT rupture with a usable PBT, this is classified as a Type II lesion in the algorithm and can be managed by tenodesis. Similarly in our patient, the postdebridement gap was too large (four centimetres) (Figure 4F) and did not allow for a direct repair despite maximal mobilization of the proximal and distal ends of the PLT.The use of tendon transfers and autografts have been proposed within literature, but evidence is limited and mostly employed in concomitant PBT ruptures[27,28]. At present, all studies surrounding the management of peroneal tendon tears or ruptures evolve around Level IV or V evidence and the consensus is that surgical intervention yields the most consistent and reproducible results.
Rehabilitation post-operatively is crucial in achieving positive outcomes. Most authors kept patients non-weight bearing for at least two weeks. During this period, a backslab or hinged boot can be employed to prevent inversion/dorsiflexion which may disrupt the tendon repair. Between two to eight weeks post-surgery, early mobilisation is encouraged through the use of an off-loading walker boot. Redfern and Myerson employs the use of stirrup brace for an additional six weeks and have a low threshold to extend the use of the boot should there be concerns regarding the repair or patient compliance[25]. It is at this point that most patients are started on a range of motion and strengthening rehabilitation programme[3,10,12,19,25].
Peroneal tenosynovitis, tendinosis, subluxation or dislocation, stenosing tenosynovitis, os peroneum fracture, acute and chronic tendon tears are part of a spectrum of peroneal tendinopathies. These conditions may co-exist or precipitate one another. In the case discussed, peroneal tendinosis likely precipitated PLT rupture.Peroneal tendinopathy was not considered and therefore, inadequate conservative treatment was prescribed.
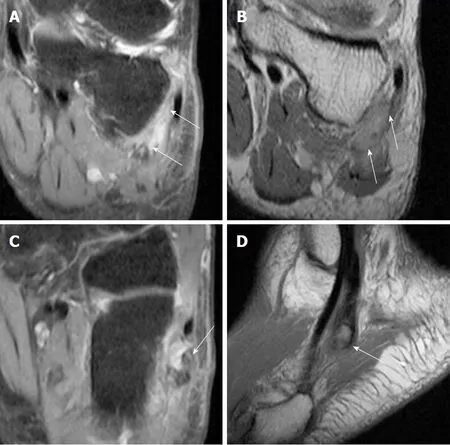
Figure 3 Magnetic resonance imaging of left foot.
We can appreciate the difficulties faced in arriving at this diagnosis. Many other authors have described similar challenges[6,10,12]. Common differential diagnosis such as lateral ankle ligament injury, base of 5thmetatarsal fractures and sinus tarsi syndrome are often considered before investigating for peroneal tendinopathy. In their series of 6 cases, Arbab et al[10]reported requiring an average of 10.8 mo to achieve diagnosis. Sammarco shared similar findings, with a series of 14 cases symptomatic between 7 to 48 mo before definitive diagnosis[6]. Patients who present acutely and receive timely surgical intervention, achieve the best outcomes. It is therefore essential to diagnose these peroneal tendinopathies early so that appropriate treatment can be commenced promptly. We propose an investigation pathway when reviewing patients with lateral ankle discomfort (Figure 5). Paramount to this is an astute clinical history and examination as well as focused radiographic investigations of the affected ankle and foot. Most differential diagnosis of lateral ankle pain can be ruled out at this juncture. In the event of raised clinical suspicion, radiographic presence or displacement of the os peroneum, persistent symptoms or the absence of a clear diagnosis - early MRI is warranted.
Tenodesis of the proximal stump of the ruptured peroneus longus to the intact peroneus brevis is a useful technique allowing for early return to activity as well as excellent post-operative clinical outcome (Table 1). More studies are required to further evaluate this technique as well as compare clinical outcomes against other techniques available within literature.
CONCLUSION

Figure 4 Intra-operative images.
PLT ruptures are rare and form part of a spectrum of peroneal tendon pathologies that is being increasingly recognized today. This case demonstrates how elusive diagnosing peroneal tendon pathology is - especially when it is rarely considered. We shared our experience in promptly diagnosing and surgically treating this patient.Tenodesis of the peroneus longus to the peroneus brevis is a useful technique in the management of peroneus longus ruptures. We achieved excellent early clinical outcome measures that remained excellent 12 mo after surgery.
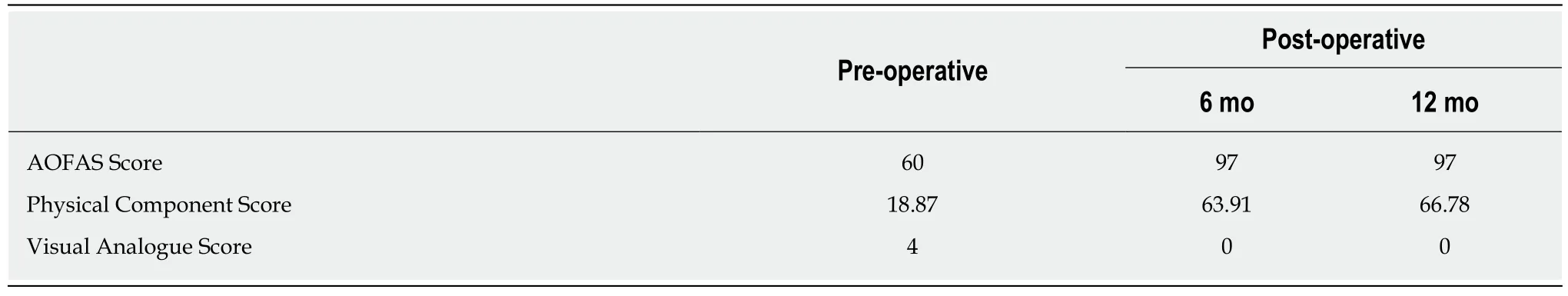
Table 1 Significant improvement in clinical outcome scores at 6 mo after surgery (excellent results were maintained at 12 mo after surgery)
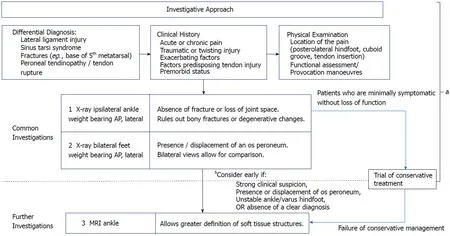
Figure 5 Investigative pathway when approaching patients with lateral ankle discomfort.
杂志排行
World Journal of Orthopedics的其它文章
- Damage control orthopaedics: State of the art
- Contralateral trapezius transfer to treat scapular winging: A case report and review of literature
- Validation of the Danish version of the musculoskeletal tumour society score questionnaire
- Inter- and intra-rater reliability of vertebral fracture classifications in the Swedish fracture register
