Clinical observation of needling gluteus medius muscle trigger point plus chiropractic for sacroiliac joint subluxation
2019-01-14ZhouWenchun周文春WangHongnan王宏南ZhangSheng张盛
Zhou Wen-chun (周文春), Wang Hong-nan (王宏南), Zhang Sheng (张盛)
Zhoushan Maternity and Infant Hospital, Zhejiang Province, Zhoushan 316000, China
Abstract Objective: To observe the clinical effect of needling gluteus medius muscle trigger point (TrP) plus chiropractic for sacroiliac joint subluxation.
Keywords: Acupuncture Therapy; Tuina; Massage; Chiropractic; Trigger Points; Joint Dislocations; Sacroiliac Joint
Sacroiliac joint subluxation is caused by external force or other pathogenic factors. The peripheral tendons and muscles around auricular joint connecting the sacrum and ilium are injured and thus exceeded their normal motion range, and then a tiny offset occurs around auricular joint (only 1.0-2.0 mm in the most tiny case)which cannot be offset naturally. Leading to the imbalance of external and internal force around the joint and the related soft tissue damage and causing clinical symptoms. Common symptoms include pain and functional disorder caused by sacroiliac joint subluxation[1]. As reported, the subluxation of the sacroiliac joint, normally the tiny offset which leads to
low back and leg pain, is generally not easy to be discovered in X-ray examination[2-4]. Sacroiliac joint subluxation can give rise to low back and hip pain and sciatica, which is one of the common reason for low back and leg pain clinically. Changing of sacroiliac joint anatomy structure will influence on the physical functions of the joint which causes swelling pain[5].Research showed patients with sacroiliac joint subluxation took up 15%-25% of all patients with low back and leg pain[6]. Besides, without the in time correction of the subluxation, patients' spine and four limbs structure will also be affected and thus cause grave physical and psychological impact on those patients, increasing treatment duration and medical expenses and also adding work load of medical personnels. Therefore, choosing a safe, convenient and effective approach to treat such case is of great importance. In this study, we used needling gluteus medius muscle trigger point (TrP) plus chiropractic to treat sacroiliac joint subluxation and compared its clinical effect with conventional acupuncture plus chiropractic, the reports were now given as follows.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Western medicine diagnostic criteria
Western medicine diagnostic criteria was based on European guidelines for the diagnosis and treatment of pelvic girdle pain[7]. ① A history of injury or gestation.② Unilateral or bilateral sacroiliac pain or external superior hip pain, may also show lower limbs movement limitation. Limping with restricted walking duration; loaded on the healthy side during standing;cannot keep sitting for a long time, and usually bear the weight on the unaffected side of the hip. In serious condition, patients cannot stretch their legs on supine position, and were prone to bend their affected limb on supine position or lied on one side. ③Physical examination showed pelvic inclination and idiopathic scoliosis, showed the slanting hip limping posture, and cannot keep the chest out and low back erection posture. Sacroiliac joint muscle spasm, the joint on affected side showed heave or sunken compared with the unaffected side, with pressing pain and percussion pain, may show palpable pain sinew nodes; asymmetric posterior superior iliac spine or posterior superior iliac spine or other bone landmark on bilateral sides, iliac crest showed different height, sacrospinale was not centered or asymmetric sacral groove; lower limbs showed different length. Positive pelvis separation test,compression test, Patrick test, rear protraction test of lower limbs and standing on single foot test. ④ Pelvic X-ray examination showed broaden sacroiliac joint gap on the affected side and pubic symphysis were not on the same level; It may also show hyperplasia of the joint margin or increased bone mineral density. Other indirect symptoms included different height of bilateral iliac crest, different width of the hip bone, asymmetric obturator and not centered sacrum. CT scan of the sacroiliac joint shows asymmetric joint gaps.
1.1.2 Diagnostic criteria in traditional Chinese medicine (TCM)
TCM diagnostic criteria was based on the Guidelines for Diagnosis and Treatment of Common Diseases of Spinal Orthopedics in Traditional Chinese Medicine[8].① With a history of injury, heavy load on the low back and hipbone, or women with a history of gestation. ②Lower back pain, with unilateral or bilateral sacroiliac joint pain or external superior pain on hip. Ischialgia like pain on unilateral or bilateral sides alternatively.Peripheral muscle spasm on sacroiliac joint of the affected side with motion limitation of lower limbs,cannot bear load, limping, symptoms may aggravate during bending, turning over and on supine position.Feeble of the affected lower limbs, may show the radiation pain of the lower limb, occasional numbness,awareness of extension or shorten of the lower limb.③Physical examination showed pressing pain or percussion pain on local sacroiliac joint, different length of the bilateral lower limbs, a sunken or satiation feeling on posterior superior iliac spine, positive result in standing on one foot test, pelvic separation test, Patrick test or bedside test. ④ Anteroposterior pelvic X-ray examination showed rotation of the pelvis (asymmetry obturator), some patients may show broaden or narrow sacroiliac joint gap on affected side, disordered joint facets arrangement, tiny vertical movement of the pubic symphysis. It may also show hyperplasia of the joint margin or increased bone mineral density in patients with a long course of disease. CT scan showed asymmetry joint facets.
1.2 Inclusion criteria
Conforming to the diagnostic criteria above, and showed gluteus medius muscle TrP when pressing on related area; without receiving other treatment methods or showed invalid results; only received needling muscle TrP and chiropractic therapy during treatment course, didn't participate in other treatment;informed consented.
1.3 Exclusion criteria
Those with a history of lower limbs bone fracture;those with spine or pelvis congenital malformation,tumor, tuberculosis, bone fracture or ankylosing spondylitis; those with lumber intervertebral disc hernation; women during lactation or gestation or patients with mental disorders; those with serious organic cardiovascular and cerebrovascular diseases or other diseases endangering life; those receiving surgery or tuina treatment in other hospital or clinics before visit; aged beyond 18-60 years.
1.4 Elimination criteria
Didn't conform to the treatment protocol; used Western or TCM medicine prohibited in this study and thus interfering therapeutic efficacy evaluation;presence of serious adverse events.
1.5 Drop-out criteria
Dropped from the treatment automatically; lost of visit during the follow-up period.
1.6 Blinding method
During the experiment period, we had set blind to symptom and sign evaluation personnel and statistics evaluation researchers, in which the practitioners,evaluation personnel and statistics researchers were separated.
1.7 Statistical methods
All data were processed using the SPSS version 21.0 software. Measurement data were described by mean ±standard deviation (±s), independent sample t-test was used for between-group comparison, paired sample t-test was used for intra-group comparison.Chi-square test was used for comparison of rate. A P level less than 0.05 indicated a statistical significance.
1.8 General data
A total of 141 patients were included between June 2015 and July 2017 in the Acupuncture Department of our hospital. Patients were all conforming to the inclusion criteria of sacroiliac joint subluxation. After examination, there were 2 patients with a history of lower limb bone fracture, 1 with hip bone fracture, 2 with lumber vertebral bone fracture, 5 with lumber disc herniation, 2 with lumbosacral malformation and 1 with depression, cases above were excluded from our study.Four patients took non-steroidal anti-inflammatory drugs (NSAIDs) during the treatment period, for NSAIDs was an effective and common medication for sacroiliac joint inflammation[9]and thus these 4 patients were eliminated from study. Finally, a total of 124 cases were included, there were 37 male and 87 female patients,and 63 cases with anterior subluxation and 61 cases with posterior subluxation. Cases were aged between 21 and 57 years with a course between 1 and 18 weeks.13 patients were dropped out due to volunteer exit or lost of visit, their final data were included for data analysis. The differences of the gender, age and duration of patients in the two groups showed no statistical significances (all P>0.05), indicating that the two groups were comparable (Figure 1 and Table 1).
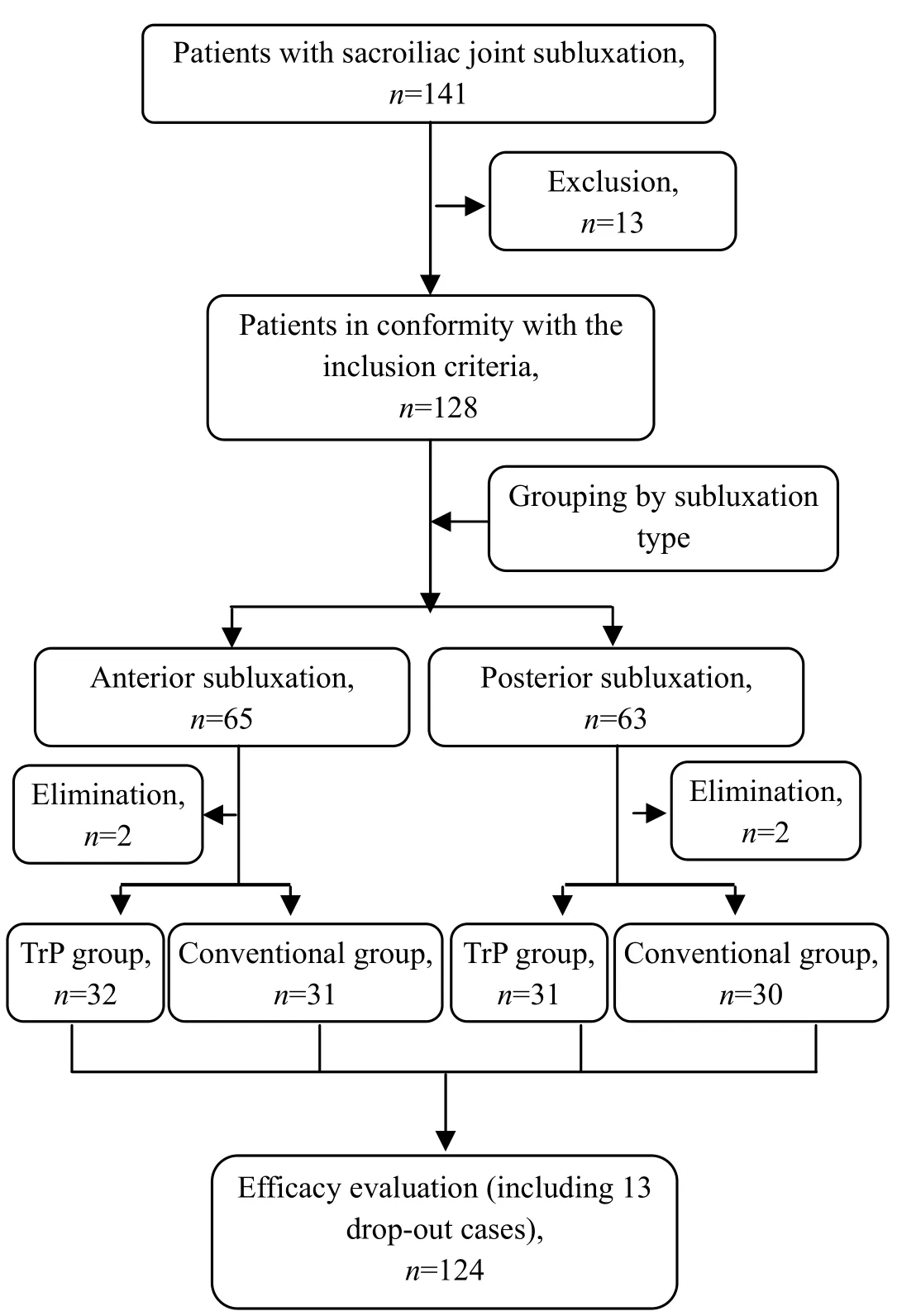
Figure 1. Flow chat of study
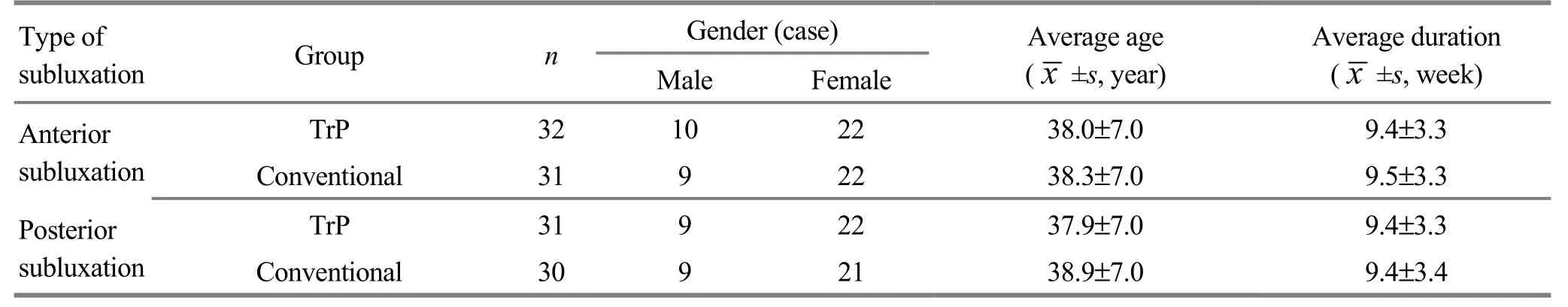
Table 1. General data comparison
2 Treatment Methods
2.1 Conventional group
2.1.1 Conventional acupuncture
Acupoints: Zhibian (BL 54), Baohuang (BL 53),Huantiao (GB 30), Juliao (GB 29) and Weizhong (BL 40)on the affected side.
Methods:Patients took a prone position. Filiform needles of 0.35 mm in diameter and 50-75 mm in length were used for manipulation. After routine sterilization, needles were inserted at acupoints above and retained for 30 min after qi arrived. Applied chiropractic method after needle withdrawing, the treatment was done twice a week.
2.1.2 Chiropractic manipulation (left side as example)
(1) Anterior subluxation
Patients' position: patients lied on their right side,bended their left knee and straightened right leg while still kept a mild curvature, stretched the medial foot into right popliteal space, hanged right knee outside the bed, crossed both hands in front of the chest, embraced left side upper arm with right hand and kept left upper arm parallel to the body, kept upper arm vertically to the body, moved the body close to the bedside and kept the body straight along bedside. Kept lower shoulder to the front and upper shoulder to the back, kept the back vertically to the bed surface and held the same level with spine.
Practitioner's position: Kept a bow stance in front of patients, leaned on the front leg, attached patients' left lower leg with practitioners' right thigh and then pushed forward slowly, until the motion transferred to ischial tuberosity. Dragged patients's right upper arm with the left hand until the motion transferred to ischial tuberosity. Touched patients' right arm genteelly,pressed on patients' left ischial tuberosity with pisiform bone on right hand. Then the preparation was finished.Faced to the patient, held patients' right wrist with left hand and then pressed it on patients' left arm. Used pisiform bone on right hand to shove surrounding soft tissue and pressed on upper middle point of the ischial tuberosity; Spread two feet as external as possible,curved right foot from posterior and lateral position to the inside position, and pressed patients' left knee to hang the left knee on bedside, formed a lever position with right foot drowning and left hand pushing forward position to finish the lock.
Adherent point: Ischial tuberosity.
Force direction: Forward.
Correction method: Practitioner took hip joint as axis,and bended upper body swiftly towards patients' back,with a force of drowning downward and toward right superior direction. On the verge of pressing pisiform bone posterior to the limit position, exerted a quick force on the 45° anterior and downwardly, during which a correction sound might be heard (Figure 2).

Figure 2. Chiropractic manipulation for anterior subluxation
(2) Posterior subluxation
Patients' position: Patients lied on their right side,bended their left knee and straightened right leg while still kept a mild curvature, stretched the medial foot into right popliteal space, hanged left knee outside the bed, crossed both hands in front of the chest, embraced left side upper arm with right hand and kept left upper arm parallel to the body, kept upper arm vertically to the body, moved the body close to the bedside and kept the body straight along bedside. Kept lower shoulder to the front and upper shoulder to the back, kept the back vertically to the bed surface and held the same level with spine.
Practitioner's position: Same preparation position as those in anterior subluxation. Then, faced to patients,held patients' right wrist with left hand and pressed on patients' left arm with force, used pisiform bone on right hand to shove surrounding soft tissue and pressed on interior side of the left posterior superior iliac spine;Spread two feet as external as possible, curved right foot from posterior and lateral position to the inside position, and pressed patients' left knee to hang the left knee on bedside, formed a lever position with right foot drowning and left hand pushing forward position to finish the lock.
Adherent point: Posterior superior iliac spine.
Force direction: Forward and upward.
Correction method: Practitioner took hip joint as axis,and bended upper body swiftly towards patients' back,with a force of drowning downward and toward right superior direction. On the verge of pressing pisiform bone posterior to the limit position, exerted a quick force on the 45° anterior and upwardly, during which a correction sound might be heard (Figure 3).

Figure 3. Chiropractic manipulation for posterior subluxation
2.2 TrP group
2.2.1 Needling TrP
The first step is finding TrP. Conforming to the criteria for hidden and activated TrP[10]: with tangible muscle belt in tension; with strong pressing pain points along tension muscle belt; Identifiable pain complaint when pressing on the point; Movement limitation caused by pain in traction range.
Fixed TrP: Hip TrP located deeply into muscle,patients may lie on the unaffected side with lower limbs bent slightly to find the TrP. Normally the TrP was hard and not easy to be punctured, causing poor therapeutic effect. Therefore, practitioner needed to fix the TrP with helping hand before puncturing manipulation.
Preparation before needling, manipulation and notifications: Marked the body surface display of the TrP with an ‘X' when the point was identified. For the shallow TrP, practitioners could use smooth palpation to fix the point between two fingers; for the deeper TrP,took forceps pinching method for fixing, or took deep palpation to hold the point between thumb and other finger tips, or directly pressed on thumb tip. Marked the possible insertion location with an ‘O' along muscle fiber. After routine sterilization, filiform needles of 0.35 mm in diameter and 75 mm in length were punctured in an angle of 30-45° with muscle fiber. During insertion,practitioner should avoid blood vessels and nerves and choose the shortest route along muscle fiber into the TrP. After insertion, to feel the slight resistance of needle tip and inquire the patients. On puncturing the TrP, practitioner may feel an increase of resistance on the holding hand, and patients felt local pain aggravation like spreading or referred pain along meridian, which was the manifestation of the correct insertion. Adjust vertical angle and horizontal direction until puncturing the correct TrP. Increase the insertion force to permeate node. Then, use rapid techniques(repeated and rapid lifting and thrusting on insertion)on the exact TrP to induce muscle fiber contraction,namely the local spasm reaction. Stop the manipulation when local spasm ceased and retain the needle for 30 min. If the needle tip reached bone during manipulation,practitioner can felt a strike or bone fracture on the needle. To avoid needle tip coarse, needle should be replaced. To avoid accident, practitioner should explain such details before manipulation, and observed patients' reaction in time.
2.2.2 Chiropractic manipulation
Same as that in the conventional group.
3 Therapeutic Efficacy Evaluation
After treatment, patients may feel an obvious swelling pain in local tissue which may continue to exist in the following 24 h. Therefore, the visual analog scale(VAS), Oswestry disability index (ODI) and therapeutic efficacy evaluation should be tested in 24 h following the last treatment.
3.1 Observation items
3.1.1 VAS score
A colored ruler of 10 cm in length and 1 mm in precision was used for VAS evaluation. 0 cm indicated no pain, 10 cm indicated unbearable pain. Informed patients to mark on the ruler to represent pain severity according to their feelings as VAS. A higher score indicated a more serious pain condition.
3.1.2 ODI score
ODI was comprised of 10 questions including pain severity, normal living activities, lifting things, walking,sitting, standing, sleep disturbance, sex, social life and travel. There were 6 choices in each question with a highest score of 5 and lowest score of 0. If 10 questions were all answered, the counting method was: actual score ÷ 50 (possible highest score) × 100%. If one of the questions hadn't been answered, the counting method was: actual score ÷ 45 (possible highest score) × 100%.A higher score indicated a more serious condition.
3.2 Therapeutic efficacy evaluation[11]
Cured: Disappeared lumbosacral pain and normal low back and leg movement.
Improvement: Alleviated lumbosacral pain and improved function.
Invalid: No improvement of clinical symptoms and signs.
3.3 Results
3.3.1 Clinical efficacy
Regardless of the anterior and posterior subluxation,the curative rate and overall effective rate in the TrP groups were all higher than those in the conventional group, between-group comparisons showed statistical significances (all P<0.05), (Table 2).
3.3.2 VAS and ODI scores
Regardless of the anterior and posterior subluxation,after treatment, the VAS and ODI scores were all dropped obviously, the differences showed statistical significances (all P<0.05), the VAS and ODI scores in the TrP groups were substantially lower than those in the conventional groups (all P<0.05), (Table 3).
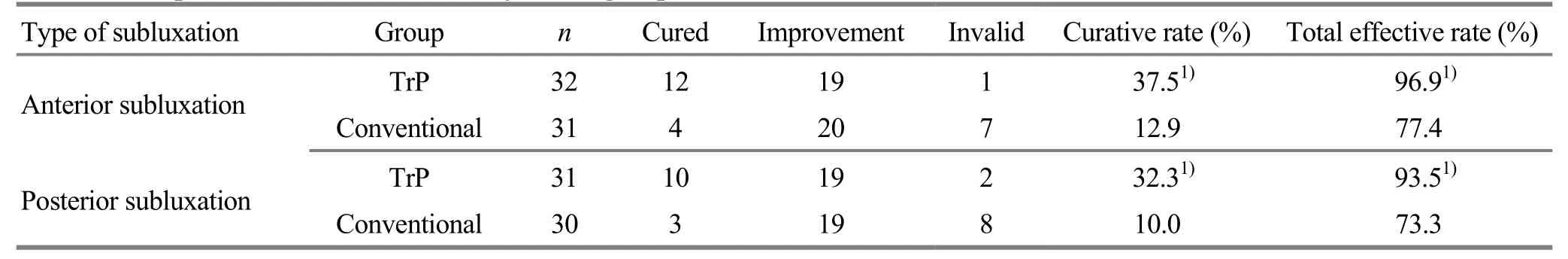
Table 2. Comparison of the clinical efficacy in two groups (case)
Table 3. Comparison of VAS and ODI scores (±s, point)
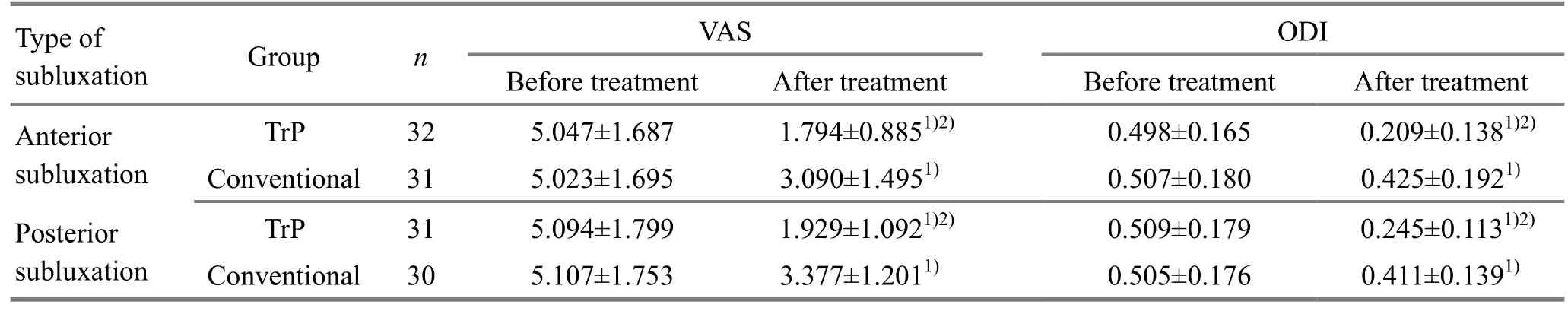
Table 3. Comparison of VAS and ODI scores (±s, point)
Note: Inter-group comparison, 1) P<0.05; between-group comparison, 2) P<0.05
Type of subluxation Group n VAS ODI Before treatment After treatment Before treatment After treatment Anterior subluxation TrP 32 5.047±1.687 1.794±0.8851)2) 0.498±0.165 0.209±0.1381)2)Conventional 31 5.023±1.695 3.090±1.4951) 0.507±0.180 0.425±0.1921)Posterior subluxation TrP 31 5.094±1.799 1.929±1.0921)2) 0.509±0.179 0.245±0.1131)2)Conventional 30 5.107±1.753 3.377±1.2011) 0.505±0.176 0.411±0.1391)
4 Discussion
The diagnosis of sacroiliac subluxation is based on symptoms, physical examination and history consultation, while lack specific examination at present time. Some symptoms and signs in the diagnosis of sacroiliac subluxation will also exist in other lumbosacral disorders[12]. The Patrick test, bedside test and pelvis separation test may also show positive result in other diseases. Moreover, for some patients with symptoms alleviation, their image results still reveal the presence of subluxation. Actually, sacroiliac subluxation is a group of symptoms caused by many diseases, not a single disease[13]. Therefore, we used VAS and ODI for therapeutic evaluation methods and didn't include image examination into the evaluation criteria.
Gluteus medius originates from the lateral side of ilium between anterior and posterior hip line, and attached to the lateral side of greater trochanter of femur. It governs the abduction of hip joint, flexion of its anterior fiber can rotate hip joint internally; extension of its posterior fiber can rotate hip joint externally[14]. In daily activities, body movement like walking, squatting and bending all require the function of the gluteus medius. Therefore, long term exercise may easily cause gluteus medius damage, followed by local muscle spasm, scar, adhesion and cause movement limitation.Compared with normal gluteus medius muscle fiber, the spasm muscle belt shows obvious difference in terms of material mechanics properties: the ultimate strength,elasticity modulus of the spasm belt are obviously higher than those in normal gluteus medius fiber; the ultimate strain of the normal gluteus medius is obviously higher than that of spasm belt, indicating that in the spasm condition, elasticity of gluteus medius decrease and intensity increase significantly[15]. Once gluteus medius is injured, ilium on the same side will be affected and sacroiliac subluxation occurs; If not be corrected in time, pelvis mechanical equilibrium will aggravate, leading to the constant presence of gluteus medius TrP. For only the material property and sacroiliac subluxation are all corrected in time, pelvis can sustain a long-term stability. Needling gluteus medius TrP can improve biomechanics in gluteus medius and thus can facilitate functional recovery of the sacroiliac joint.
TrP is the abbreviation of myofascial TrP (MTrP). The existence of TrP is related with myofascial pain, visceral pain and nerve root pain, in which the myofascial pain is most closely related. The definition of TrP is hyperirritable regions in the fascia surrounding skeletal muscle[16]. Pressing pain can be induced in the region along with specific referred pain and autonomic nerve reaction. TrP acupuncture is a further development of traditional acupuncture theory (especially the meridian and Ashi point); the location, allocation and pain pattern of TrP are close to those of conventional acupuncture, it's one of the component of traditional acupuncture[17]. Until now, there are 255 TrPs known on 147 muscles around the whole body, their area is normally less than 1 cm × 1 cm. Needling or sustained pressing (10 s) can induce referred pain in the related area. There are also palpable nodules in those area[18].TrP is similar to Ashi point. Therefore, TrP could be the modern medicine explanation of ashi point. For pain usually generates in the location of qi stagnation and blood stasis, according to the treatment principle of taking pain site as acupoint, needling TrP can direct needle sensation to the affected area, and thus dredging channel, regulate qi and blood[19].
Conventional acupuncture aims to stimulate fixed acupoint, and treat disease by the function of acupoints and meridians. On qi arrival process, patients may feel swelling pain or other needling sensation and then needle can be retained, the modern medical mechanism is still not clear yet. While in the process of needling TrP, patients may feel a stronger swelling pain than that in the conventional acupuncture. Moreover, a TrP requires multiple piercing stimulation, causing distending pain or even local spasms to finish the treatment, such method can increase pain threshold in pain receptor of local muscles.
With regard to the formation of TrP, the most famous theory is the synthesis TrP hypothesis[20]: the joint construction of the energy crisis hypothesis and the endplate dysfunction hypothesis. The energy crisis hypothesis: due to the lacking of adenosine triphosphate (ATP), the myosin-troponin transverse bridge cannot be broken and the myosine is unable to relax and form TrP; during the reabsorption of calcium by sarcoplasmic reticulum, lacking of ATP causes the myosin-troponin transverse bridge fails to maintain the connection, and finally result in muscle continuous contraction and the formation of TrP. Endplate dysfunction hypothesis: motor neurons continuously transmit contractile messages to muscle fibers, and therefore secreting too much acetylcholine to synapse,causing excessive action potential in the motor endplates on the muscle fibers, and forming persistent motor endplates depolarizing. Therefore local muscle fibers demand more ATP, and thus adenosine triphosphate is depleted in the motor endplate area and finally resulting in an energy crisis near the motor end plate. Continuous muscle contraction causes continuous arterial blood supply blockage and venous return blocking. Metabolic wastes stimulate muscle tissue and cause pain. Pain causes more muscle contraction, so the accumulation of metabolic wastes in veins will become more serious and finally, forming the vicious cycle of pain-spasm-ischemia. The causes of TrP in daily life are roughly as follows: long time repeated limb movements, bad postures, cold, fatigue, long time injury without proper healing, and long time pain without relief. The two mechanisms of acupuncture treatment for TrP are to block the vicious cycle of pain-spasm-ischemia, improve the blood circulation of local muscles at TrP, and therefore reducing pain, and obviously blocking the process of the vicious cycle.However, conventional acupuncture rarely stimulates TrP accurately, so it is ineffective for spastic muscles in the area of TrP.
Results in this study showed: regardless of anterior and posterior subluxation, VAS and ODI scores in the TrP group and conventional group all dropped significantly,while the improvement in the TrP group was higher than those in the conventional group. The cured rate and total effective rate in the TrP group were all higher than those in the conventional group. These results indicate that needling TrP plus chiropractic had a better therapeutic effect than conventional acupuncture plus chiropractic for sacroiliac joint subluxation.
Conflict of Interest
The authors declared that there was no potential conflict of interest in this article.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in this study.
Received: 25 September 2017/Accepted: 29 October 2017
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Analysis of acupoint-selection patterns in acupuncture-moxibustion treatment of polycystic ovarian syndrome based on data mining
- Clinical observation on tuina plus foot bath with Chinese medicine for diabetic foot in early stage
- Effect of tuina exercise on simple obesity in college students
- Therapeutic effect observation on acupuncture plus umbilicus application with Chinese medicine in treating detrusor underactivity
- Memory response to manual acupuncture in chronic insomniacs: evidence from event-related potentials
- Fire-needle therapy for deglutition disorders in post-stroke pseudobulbar palsy:a randomized controlled trial