Miniaturised percutaneous nephrolithotomy:Its role in the treatment of urolithiasis and our experience
2018-12-25GuohuaZengWeiZhuWayneLam
Guohua Zeng *,Wei Zhu 1,Wayne Lam
a Department of Urology,Minimally Invasive Surgery Center,The First Affiliated Hospital of Guangzhou Medical University,Guangzhou,China
b Guangzhou Institute of Urology,Guangdong Key Laboratory of Urology,Guangzhou,China
c Division of Urology,Department of Surgery,Queen Mary Hospital,Hong Kong,China
KEYWORDS Percutaneous nephrolithotomy;Mini-percutaneous nephrolithotomy;Super-minipercutaneous nephrolithotomy;Irrigation-suction sheath
Abstract Miniaturized percutaneous nephrolithotomy(PCNL)procedures have gained increased popularity in recent years.They aim to reduce percutaneous tract size in order to lower complication rates,while maintaining high stone-free rates.Recently,miniaturized PCNL techniques have further expanded,and can currently be classified into mini-PCNL,minimally invasive PCNL(MIP),Chinese mini-PCNL(MPCNL),ultra-mini-PCNL(UMP),micro-PCNL,mini-micro-PCNL,and super-mini-PCNL(SMP).However,despite its minimally-invasive nature,its potential superiority in terms of safety and efficacy when compared to conventional PCNL is still under debate.The aim of this review is to summarise different available modalities of miniaturized PCNL,details of instruments involved,and their corresponding safety and ef ficacy.In particular,this article highlights the role of the SMP and our experience with this novel technique in management of urolithiasis.Overall,miniaturized PCNL techniques appear to be safe and effective alternatives to conventional PCNL for both adult and pediatric patients.Well-designed,randomized studies are required to further investigate and identify specific roles of miniaturized PCNL techniques before considering them as standard rather than alternative procedures to conventional PCNL.
1.Introduction
The incidence of nephrolithiasis continues to increase worldwide across all ages,leading to an increasing number of both adults and children requiring treatment for renal stone disease.The goal of active stone treatment strategies should aim to achieve complete stone clearance in a short operative time with a short hospital length of stay,and minimal risk of complications.Common approaches in active treatment of renal stone disease include extracorporeal shock wave lithotripsy(ESWL),retrograde intrarenal surgery(RIRS),and percutaneous nephrolithotomy(PCNL).Open and laparoscopic surgery are other treatment options but reserved only for selected patients.
PCNL was first described by Fernstro¨m and Johansson in 1976[1],and has since become an established treatment modality in the management of renal stones that are larger than 2 cm[2].PCNL has the advantage of achieving high stone-free rate(SFR)when compared to other treatment modalities,but it is relatively invasive[3].Based on the data reported by British Association of Urological Surgeons(BAUS)[4]and Clinical Research Office of the Endourological Society(CROES)[5],risks associated with PCNL include postoperative sepsis(2%),fever(10%-16%),and perforation of adjacent organs(0.4%).In particular,blood transfusion(3%-6%)and significant bleeding(8%)are not uncommon complications after PCNL,with potentially devastating consequences.To reduce risk of bleeding,the use of smaller PCNL tract size has recently been advocated to decrease renal parenchymal trauma.In 1998,Jackman et al.[6]first developed a specifically designed minimally invasive PCNL(mini-PCNL)device for children.In 2001,a specially designed miniaturized nephroscope for mini-PCNL in adults was first coined by Lahme et al.[7]in Germany.Since then,the “mini-PCNL” technique has developed rapidly and become increasingly popular worldwide.
2.Currently available miniaturized PCNL techniques
The common denominator of the mini-PCNL technique is the use ofsmaller instruments through smaller diameter sheaths.The use of a variety of endoscopes has been described by various authors for stone disintegration and removal,using accesssheath size ranging from11 to 20 Fr.However,the term“mini-PCNL” remains poorly defined,with many studies using overlapping terminology for the same size sheath.The growing diversity of the surgical technique has led to an increasing confusion in the terminology of mini-PCNL.Terminologies recommended by different groups over the years are summarized in Table 1[6,8-13].
2.1.Mini-PCNL
The term “mini-perc” appears through the literature,using access sheath size between 11 and 20 Fr[8,9,14].The procedure is performed with the use of an 11 Fr peel-away vascular access kit.An access needle is introduced through the desired calyx,followed by the insertion of a guidewire.The sheath and the trocar are railroaded over the guidewire under fluoroscopic guidance.Following the removal oftrocar,the sheath is peeled down to obtain optimal working length.The necessary endoscopes for mini-PCNL are a 7.0 Fr rigid pediatric cystoscope and a 9.5 Fr flexible ureterorenoscope.For stone disintegration,either a holmium laser or lithoclast can be used.Fragments are removed by irrigation and suction,or by a grasping device.A recent study,which involved a series of 1368 patients,demonstrated that mini-PCNL was able to achieve a high SFR of 82%using a 16 Fr tract[15].Compared with conventional PCNL,significant bleeding complications were less common(1.4%).When compared with RIRS,mini-PCNL was able to provide a significantly higher SFR with better efficiency[16].

Table 1 Current nomenclature of mini-PCNL techniques.
2.2.Minimally invasive PCNL(MIP)
MIP was first described in 2007 by Nagele et al.[8].The MIP system utilizes a 12 Fr nephroscope with a 6.7 Fr central channel,single stage dilators and corresponding operating sheaths.It is available in three different sizes,including the 15/18,16.5/19.5,and 21/24 Fr sheaths(representing the inner and outer circumferences).There is an irrigation channel within the sheath as well as the working channel.The key features of the MIP system include single step dilation and automatic pressure control.Stone fragmentation is carried out using a ballistic lithotripter.The fragments are evacuated with a combination of its low-pressure irrigation system and the retraction motion of the nephroscope from the sheath.Stones are evacuated due to the difference of the intrarenal pressure and the pressure outside the apparatus.This phenomenon has been described as the “vacuum effect” [17].In contemporary urological practice,MIP serves as an alternative to ureterorenoscopy for both small and large complex renal stones,as well as in the treatment of upper ureteric calculi.A retrospective analysis of 83 MIP procedures demonstrated that this technique was not only effective in small renal stones,but also in patients with high stone burden,including patients with complex renal stones.SFR was shown to be excellent.The study also demonstrated that MIP was able to reduce blood loss and transfusion rate,and significant complications reported in the series were low[18].Kruck et al.[19]carried out a retrospective study comparing efficacy and safety of RIRS and MIP,and their results showed that MIP had a higher efficacy despite treating larger stones in the series,and was associated with low treatment failure and stone recurrence rates.
In another study,Hennessey et al.[20]identified other advantages of MIP over both standard PCNL and RIRS.Firstly,patients’position was more flexible than RIRS and at least as equally flexible as standard PCNL.The compact design of the MIP system allowed a wide range of movement even with limited exposure when performing PCNL in prone position.Secondly,the MIP single-stage dilatation design required fewer and simpler steps than conventional standard PCNL to create precise renal access and track.Thirdly,supra costal access could be achieved with less restriction when compared with conventional PCNL during MIP.This was likely due to the narrower and more robust metal MIP sheath design,allowing it to pass between the ribs smoothly and manipulated downward easily without the need to bend the sheath.Finally,their paper also suggested that MIP does not have a steep learning curve,and is a straightforward for surgeons experienced with standard PCNL.For surgeons with lesser experience,the authors suggested that MIP appeared to be an excellent PCNL learning tool,with the smaller dilators providing reassurance of lesser trauma and bleeding.
2.3.Chinese mini-PCNL(MPCNL)
We have previously investigated the use of MPCNL in the management of upper urinary tract stones in over 12 482 patients at our center,which is currently the most popular miniaturized PCNL technique in China.The instruments involved consist of an 8.0/9.8 Fr semi-rigid ureteroscope[21]or a specially designed 8.5/12.5 Fr mini nephroscope[9],and a pulsatile high-pressurized endoscopic perfusion pump.The dilation of the percutaneous tract was serially performed with scaled fascial dilators,starting from 8 Fr and could be dilated up to 14-20 Fr[22].The use of fascial dilators with scaled marker to create percutaneous access in MPCNL was shown to reduce radiation duration,as depth of sheath insertion required for dilatation can be better estimated.
Both SFR and complication rate remains high[22].Majority of stone fragments when using this technique were pushed out via the sheath with the pulsed perfusion pump.The pump used is able to generate pressure up to 300 mmHg forapproximately 3 s,and then pause for2 s,before the cycle repeats.Rapid removal of the endoscope out of the sheath synchronized with the low-flow irrigation period further creates a relative vacuum within the sheath.This,together with the recoilofthe system fromthe transient high pressure generated by the irrigant,stone fragments are flushed out effectively.This method has been shown to be able to significantly shorten the operative time,as stone fragmentation and removalcan be carried outcontinuously with little down time for instrument.Importantly,the pressurized irrigation did not create a dangerously high intrapelvic pressure.Our previously published data showed that during MPCNL with 14,16,18 Fr sheaths,and in patients where double-16 Fr percutaneous tracts were required,the average renalpelvic pressure(RPP)were 24.85,16.23,11.68,and 5.80 mmHg,respectively,which were lower than the level needed for a backflow(30.00 mmHg)[23].
Currently,the indication for MPCNL has been broadened to all the upper urinary tract calculi that require standard PCNL intervention in many centers across China.We retrospectively reviewed 5 761 simple renal stones and 8 223 complex renal stones that were managed by MPCNL between 1992 and 2011[24].The one-session SFRs of MPCNL were 77.6%for simple stones and 66.4%for complex stones.The overall complication rate was 17.9%-19.0%and the blood transfusion rate was 2.2%-3.2%.No significant difference in SFR between the MPCNL and standard PCNL was demonstrated.However,MPCNL was shown to be able to achieve a better stone clearance rate for multiple caliceal stones in another study(85.2%vs.70.0%)[25].Higher SFR was also achieved in the treatment of staghorn stones by using MPCNL via multiple access tracts(89.7%vs.68.0%)[26].In patients with solitary kidney with renal stones larger than 2 cm in size,MPCNL was proved to be a significantly more effective treatment alternative to RIRS,with a better SFR and a comparable complication rate[27].In patients with anomalous kidneys such as horseshoe kidney,polycystic kidney and transplanted kidney,MPCNL has been shown to be safe and feasible[25-28].
2.4.Ultra-mini-PCNL(UMP)
UMP is a recent addition to the armamentarium in the everevolving PCNL techniques,which makes use of a 3 Fr telescope with a specially designed 7.5 Fr nephroscope that allows the surgeon to carry out PCNL with an 11-13 Fr sheath[29].The smaller tract size ultimately provides a reduction in cross-sectional surface area to nearly 1/8 of the original tract size used in convention PCNL(30 Fr),reducing risks of bleeding and tissue trauma.Even if UMP is being carried out in kidneys with a narrow infundibulum,the small-sized UMP sheath is able to advance without causing significant injury to the infundibulum.The working sheath of UMP system has a very small tube of 3 Fr welded to the inner wall before being connected to a port externally.This special design of the working sheath has the advantage of stone fragment retrieval without the use of baskets or graspers.UMP has been shown to be associated with a minimal complication rate,a high SFR and a very low rate of requiring auxiliary procedures[10,30],and is in particularly useful in the treatment of stones<20 mm in diameter in lower pole calyx.On the other hand,when compared with ESWL,UMP has been found to be beneficial when treating lower calyx stones with long and narrow calyces and a sharp angle where fragments do not pass easily[31].Wilhelm et al.[32]performed a matched analysis to compare UMP and RIRS for treatment of renal stones 10-35 mm and found that both techniques achieved high SFRs and favorable complication rates.However,both operation and in-hospital times were longer in the UMP cohort.
2.5.Micro-PCNL
“How small can we go?” This was the hypothetical question and the basis for developing micro-PCNL.This technique is carried out using a 4.85 Fr “all-seeing needle” [11].The most important advantage of micro-PCNL is its ability to reduce blood loss.The renal access and PCNL were performed in one single step under direct visualization.The working hypothesis of the “all-seeing needle” is that if the initial tract is perfect,then the tract-related morbidity can be reduced.The perfect tract or the tract that causes the least amount of bleeding is the one that provides access to the kidney in the shortest possible distance through the cup of the calyx.The microoptics of the needle will help to confirm the visual cues of a correct papilla,avoiding traversing incorrect viscera.The needle then confirms the correct entry from the cup of the planned calyx.The operator could withdraw the needle and enter in the correct plane and angle if the tract is not perfect.This advantage,when using the “all-seeing needle”,is particularly evident when puncturing ectopic kidneys,as it provides direct optical visualization when accessing the pelvicalyceal system.This enables the surgeon to be assured that no bowel structure has been traversed.
During micro-PCNL,stone clearance relies on adequate vaporization and pressurized irrigation,as this procedure does not allow any fragment retrieval at all.micro-PCNL has been used to manage both single and multiple renal calculi,the latter can be achieved with additional punctures but with a cumulative diameter of still less than 1.5 cm in diameter.Reduced risk of blood loss is a major advantage of micro-PCNL.In the first micro-PCNL study,the mean decrease in hemoglobin level was low at 14 mg/L.Blood loss requiring transfusion was reported as very low at 0.71%in a the subsequent study[33].
Sabnis et al.[12]compared micro-PCNL and RIRS in the management of renal calculi<1.5 cm.Similar SFR and low risk of complications were found in both arms.However,RIRS had favorable postoperative pain scores and a lower hemoglobin drop.On the other hand,micro-PCNL was associated with better surgeon comfort and lesser need for ureteric stenting.The advantage of micro-PCNL in terms of operative efficiency and stone clearance efficacy appeared to be especially evident when managing lower calyceal stones.
2.6.Mini-micro-PCNL
This procedure is a modification of the previously described micro-PCNL[34].As the micro-PCNL is such narrow caliber,with a propensity to bend during manipulation and stone treatment,an 8 Fr metallic sheath is introduced,which allows passage of a lithoclast probe with suction.A ureteric catheter further reduces the intrarenal pressure.The minimicro-PCNL sheath has the advantage of easier intrarenal manipulations,can accommodate the 1.6 mm ultrasonic lithotripter and allow the attachment of the three-way connector of the standard micro-PCNL.
3.Super-mini-PCNL(SMP)and authors’experience
3.1.First-generation SMP
The aforementioned miniaturized PCNL procedures have gained increasing popularity in the recent years,with reduced percutaneous tract size lowering bleeding-related complication rates while maintaining good SFRs.However,there are disadvantages of miniaturized PCNLs when using smaller tract sizes.These include limited continuous irrigation flow,poorer endoscopic visualization,difficult stone fragment extraction,and the theoretical risk of persistently elevated RPP intraoperatively.In 2012,we developed thefirst-generation SMP system to address many of these defi ciencies in the miniaturized PCNL techniques[13].The basic components of the first-generation SMP system are a 7 Fr miniature nephroscope with enhanced irrigation capability and a modified nephrostomy access sheath with continuous negative pressure aspiration.The nephroscope has a 3.3 Fr working and irrigation channel that can accommodate a 0.8 mm pneumatic lithotripter probe,a laser fiber up to 365 μm or a 2.5 Fr stone basket.The major difference between first-generation SMP and the UMP and micro-PCNL is the way the stone fragments are managed.In UMP,the stone fragments are flushed out by the recoil of pressurized irrigation together with rapid removal of the endoscope out of the working sheath.In micro-PCNL,the stone fragments are simply left in situ for later spontaneous passage with stones being dusted and not fragmented,the principle of which is similar to flexible ureterorenoscopic stone dusting.Without the help of an outer sheath,puncture must be precise at the desired calyx to accommodate the use of a thin scope.If the stone is migrated into a calyx distant from the puncture site,or access has been created into an inappropriate calyx,treatment using this technique could be challenging.
In SMP,stone fragments are removed by negative pressure aspiration,with the ultimate goal of rendering the patient completely stone free at the end of the procedure.There are several advantages when using SMP.Firstly,stone extraction is feasible,therefore both stone fragmentation and dusting can be used.Secondly,stone fragments tend to aggregate at the opening of the sheath making lithotripsy and removal of stone fragments more efficient.Thirdly,with the ability to use a continuous irrigation despite in a miniaturized system,visual field is clearer.This is because“dust storm”traditionally caused by stone pulverization is minimized with such a irrigation system.Bleeding caused by large PCNL tracts becomes minimal with the use of a miniaturized puncture system,which further improves thefield of vision.Lastly,the use of negative pressure aspiration facilitates irrigation drainage but at the same time maintains a low average RPP throughout the procedure.This is the case even when a high-pressure irrigation using a peristaltic pump is being used.This offers the benefit of reducing the risk of sepsis due to excessive RPP intraoperatively(Table 2)[35].
The clinical outcomes of the first-generation SMP system have been shown to be favorable in our previous studies.Between September 2012 and September 2014,SMP was successfully completed in 146 patients in 14 medical centers.This series included patients who had failed stone treatment with RIRS or ESWL.The mean stone size was 2.2 cm,and 90.1%of patients were rendered stone-free after a single-session procedure.Only 3.4%of patients required conversion to the conventional mini-PCNL.Complication rate was 12.8%.However,they were all of Clavien-Dindo classification Grade 1 or 2 only.No transfusion was required in any patient.Around 72.3%ofpatients did not require any upper tract drainage(totally tubeless).The mean postoperative hospital stay was 2 days.

Table 2 Character of RPP during the first-or new-generation SMP[35].
SMP can also potentially benefit pediatric patients.There has been concerns that RIRS may be associated with a small but not insignificant risk of injury to the delicate pediatric ureters[36].Kim et al.[37]reported that more than half of pediatric patients required passive dilatation of the ureter 1-2 weeks before a ureteroscope could be inserted into the ureter.Another limitation of RIRS in the pediatric population includes the instrument’s short life span and high cost of maintenance.
In contrast,it is possible to perform an SMP in the first setting in nearly all children.The results from our series study have demonstrated that SMP is safe and effective for the management of renal stones in children.In our previous study which investigated a cohort of pediatric patients with a mean stone burden of 1.4 cm,the one-session SFR was high at 84.7%[38].Other advantages include short treatment time,high tubeless rate and its effective accessibility to lower pole stones.The complication rate of SMP,as per our initial experience,has been low.
3.2.New-generation SMP system
The first generation SMP consists of an irrigation system that is delivered through the same channel as the working instruments.This design restricted irrigation flow once a laser fibre or pneumatic lithotripter device was inserted,leading to suboptimal visualization requiring longer operative times.To overcome this limitation,the newgeneration SMP utilizes a novel irrigation-suction sheath to improve irrigation,which also enables the use of more efficient stone fragmentation devices to improve stone clearance[39].
The basic components of the new-generation SMP system are an 8.0 Fr miniaturized nephroscope,together with a newly designed irrigation-suction sheath(Fig.1).The SMP telescope has a 1.4 mm working diameter with a 40 000-pixel resolution.The sheath consists of a two-layered metal structure,available in either 12 or 14 Fr[39].The space between the two layers of the sheath forms an independent irrigation channel,and the central lumen of the sheath works as a conduit for continuous suction.To achieve this irrigation-suction system,the sheath contains both an irrigation port and a suction port(Fig.2)[35].
With the new-generation SMP,irrigation inflow is delivered through the sheath.This frees up a working channel space adjacent to the nephroscope,which enables surgeons to introduce larger working instruments(such as a 550 μm laser fiber or a 1.0 mm lithotripter)for better stone fragmentation without reducing irrigation efficacy.

Figure 1 New-generation super-mini-percutaneous nephrolithotomy system.
The new-generation SMP system is also able to provide a more efficient hydrodynamic mechanism for retrieval of fragments when compared to other miniaturized PCNL systems.In irrigation systems utilized in other miniaturised PCNL such as the first-generation SMP and MPCNL,both inflow and outflow of irrigation take place within the same lumen of the sheath.As a result,the inflow partially offsets the effect of outflow,subsequently pushing stone fragments back into the collecting system,which potentially leads to stone migration and increases the operation time.The irrigation-suction sheath in the new-generation SMP systems allows the inflow and outflow to follow separate channels,creating a one-way flow system.The inflow that enters the collecting system via the irrigation channel of the sheath,and is then aspirated back out of the system through the suction conduit of the sheath(Fig.3).This system allows efficient stone removal,and results from our prospective study showed that the new-generation SMP using the new irrigation-suction sheath had a shorter operative time than the first-generation SMP[35].
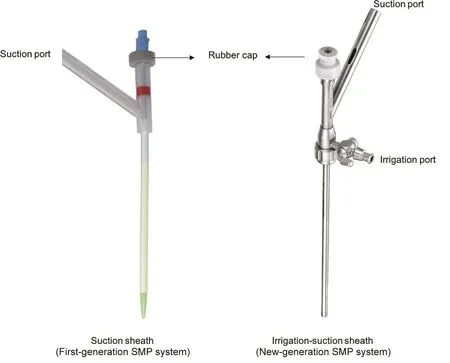
Figure 2 The working sheath used in the first-and the new-generation super-mini-percutaneous nephrolithotomy system[35].
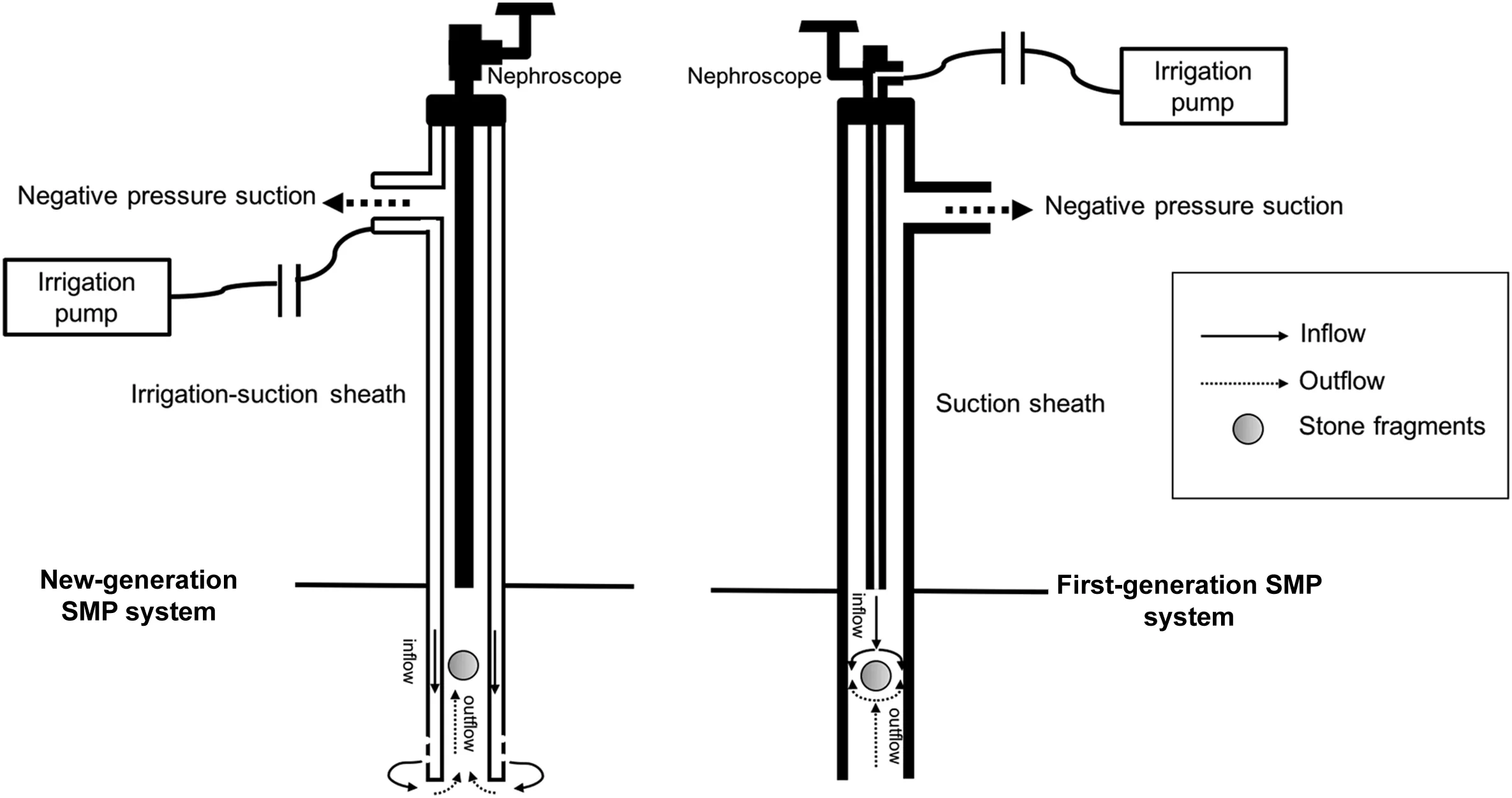
Figure 3 The hydrodynamic mechanisms for retrieval fragments in the first-and new-generation percutaneous nephrolithotomy systems[35].
Another modification of the new-generation SMP is the use of medically-graded steel instead of plastic,which was used in the first generation SMP with an intention to reduce renal parenchymal trauma.The reason for this is that,in our experience,the flexibility associated with a plastic sheath allowed nephroscope to be bent excessively leading to scope damage.
3.3.Comparison of SMP with conventional techniques
Several comparative studies have been conducted to compare SMP with other modalities of management of renal stone,with many studies demonstrated that SMP had a higher efficacy and lower complication rate[40,41].
3.3.1.SMP vs.RIRS
According to the available literature,SFR with RIRS ranges from 65%to 92%,and it is known to be associated with a low risk of complications when treating small renal stones[42].However,when treating lower calyceal calculi,SFR of RIRS falls,especially if the lower calyceal infundibulum is narrow with an acute infundibulo-pelvic angle.Other disadvantages of RIRS include the need to carry out staged procedures if ureter requires passive dilatation for access,high cost,need of multiple sessions to improve SFR in many cases if stone size is large or at unfavourable positions,risk of ureteric damage,and the fact that many patients require temporary ureteric stenting[27].In our recently concluded multi-centers prospective randomized trial comparing SMP with RIRS in management of lower-pole renal calculi<2 cm(NCT 02519634),we found that SMP was more effective than RIRS in terms of a better SFR and lesser auxiliary rate.The complications and hospital stay were comparable between the two modalities,although RIRS has the advantage of less postoperative pain(article in press).This study demonstrated that SMP could be considered as a safe and effective alternative to RIRS in the management of small renal calculi,in particular when managing patients with lower calyceal calculi.
3.3.2.SMP vs.MPCNL
MPCNL is a multistep procedure similar to conventional PCNL,except for the smaller tract size.The complication risks related to tract size in MPCNL is expected to be lower in SMP.Although SMP has been shown to be safe and feasible in both adults and pediatric populations with moderate renal calculi size,the use of SMP in patients with larger stone burden has yet to be determined.Our results from propensity score-matched analysis showed that SMP was equally effective as MPCNL for large renal stones(>2 cm),and was comparatively more effective in management of patients with simple stone.Meanwhile,SMP was comparatively superior in terms of length of hospital stay and tubeless rate[40].Due to the inherent limitations of the study,further large cohorts prospective,multi-center,and randomized controlled trial should be conducted to confirm our findings.
3.3.3.SMP vs.ESWL in pediatric patients
Despite its relatively uncommon incidence,management of the urinary stones in children poses a specific technical challenge.Taking their relatively higher stone recurrence rates within small,growing kidneys in the pediatric population into account,aims of the management include complete stone clearance,preservation of renal function and prevention of new stone formation.ESWL has been a popular treatment of choice.However,the main disadvantage of ESWL is the need of multiple treatment sessions,and many patients often require additional auxiliary procedures to achieve complete stone clearance.Although ESWL is still the treatment of choice in the majority of pediatric kidney stones due to its safe and non-invasive nature,our recent retrospective study[41]suggested that SMP is a valuable alternative.SMP in selective pediatric patients is able to achieve a comparatively higher SFR through a single treatment session,with a high totally tubeless rate,lesser need for auxiliary procedures to clear stones,and comparable complication rates when managing stones sizing less than 25 mm[41].Moreover,when compared with ESWL,the use of SMP is not limited by both stone(size,location,and density)and patient(obesity and anatomic abnormalities)related factors.
3.4.Current role of SMP
SMP is still in its early stages of development.In our center,it is most commonly used to manage moderatesized renal calculus or in patients with multiple renal calculi.Although SMP can be used in treatment of larger stones,the decision to use SMP should be prudent and the procedure should be performed by an experienced surgical team familiar with the equipments.Patient selection is of the utmost importance for successful treatment with SMP.In our experience,optimal indications for SMP include 1)Adult patients with stone size≤3.0 cm,especially for patients with previous failed SWL or RIRS approaches,or in patients not amenable to RIRS due to unfavourable anatomy(acute lower calyceal angle,long infundibulum);2)Pediatric patients with stone size<2.5 cm in whom treatment with ESWL failed.
4.Conclusion
Despite being first described nearly 2 decades ago,miniaturized PCNL techniques have yet to gain widespread acceptance,and its place within the armamentarium of renal stone surgery remains to be defined.The safety and efficacy of the many miniaturized PCNL techniques have been investigated in both adults and pediatric populations.Miniaturized PCNL appears to be a reasonable alternative for patients with small-to-medium-sized stone,and has been demonstrated to be associated with higher totally tubeless rate.Further well-designed,randomized studies are needed to better understand specific roles in the use various currently available miniaturized PCNL techniques,before considering them as standard rather than alternative procedures in the management of renal stone.
Author contributions
Study design:Guohua Zeng.
Data acquisition:Wei Zhu.
Data analysis:Wayne Lam.
Drafting of manuscript:Wei Zhu.
Critical revision of the manuscript:Guohua Zeng,Wayne Lam.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgement
This work was financed by a grant from the National Natural Science Foundation of China(Nos.81670643 and 81370804)and the Science and TechnologyProgram of Guangzhou,China(No.201604020001).
杂志排行
Asian Journal of Urology的其它文章
- Present indications and techniques of percutaneous nephrolithotomy:What the future holds?
- Ureteral stents in urolithiasis
- Retrograde intrarenal surgery:An expanding role in treatment of urolithiasis
- Indications and contraindications for shock wave lithotripsy and how to improve outcomes
- Medical therapy for nephrolithiasis:State of the art
- Defining metabolic activity of nephrolithiasis-Appropriate evaluation and follow-up of stone formers
