The Fontan Circulation: Contemporary Review of Ongoing Challenges and Management Strategies
2018-07-04AhmedKheiwaMDAnushreeAgarwalMDandAnithaJohnMDPhD2
Ahmed Kheiwa, MD, Anushree Agarwal, MD and Anitha John, MD, PhD2
2Division of Cardiology, Department of Pediatrics, Children’s National Health System, George Washington University,111 Michigan Avenue Northwest, WW 3rd Floor, Washington, DC 20010, USA
lntroduction
The Fontan operation, fi rst described by Fontan and Baudet [1] in 1971, was introduced as a palliative procedure for patients with tricuspid atresia.It later evolved to become the palliative surgery for other forms of congenital heart disease (CHD) with single ventricle physiology in which biventricular repair is not feasible.Since the original description, there have been multiple modifications of the surgical technique [2, 3].The procedure creates nonpulsatile pulmonary fl ow via direct connection of the venae cavae to the pulmonary arteries and results in an immediate elevation in central venous pressure.The unique physiological consequences of the Fontan circulation not only impact the cardiovascular system but also impose challenges at a multisystem level.In this review, we provide a summary of the Fontan surgeries and resultant physiology, discuss long-term complications, and provide a contemporary review of the management strategies.
Evolution of the Fontan Operation
The Fontan procedure attempts to circumvent the need for a subpulmonary ventricle by redirecting systemic venous return from the superior vena cava and inferior vena cava directly to the pulmonary arteries.The initial concept, when Fontan palliation was fi rst described, was to use the right atrium as a pumping chamber.The surgical technique included a classic Glenn anastomosis with a valved homograft between the right atrial appendage and the main pulmonary artery, trying to use the right atrium as a pump to the pulmonary arteries, which led to the classic Fontan procedure, or the atriopulmonary connection (APC; see Figure 1A).This procedure leads to substantial adverse hemodynamic consequences, including massive right atrial dilatation and resultant complex atrial arrhythmias and thromboembolic events.
Subsequently, multiple modifications to the surgical technique have been proposed to improve the fl ow dynamics of the Fontan circuit.In 1987, de Leval et al.[2] described the creation of an intraatrial channel to direct the inferior vena cava fl ow to the pulmonary artery called theintracardiac lateral tunnel(ILT, Figure 1B).Soon thereafter, in 1990,Marcelletti et al.[3] described the use of extracardiac conduit directing the inferior vena cava fl ow to the pulmonary arteries called theextracardiac conduitmodification (Figure 1C).In the current era the latter two modifications are the standard surgical techniques used in most surgical centers.Another modification of the Fontan procedure was the creation of a fenestration to permit a controlled right-toleft atrial shunt so as to maintain cardiac output in high-risk patients, particularly during phasic elevation of pulmonary vascular resistance (PVR) [5].This technique has been used to reduce the complications of low postoperative cardiac output, pleural and pericardial effusions, ascites, ventricular dysfunction, diminished exercise performance, and protein-losing enteropathy (PLE) and to improve postoperative survival [6 ,7].In the long term,patients are at increased risk of systemic embolization and systemic desaturation.Careful assessment should be performed before fenestration closure is undertaken [6, 8, 9].The practice of creating a fenestration initially differs at different centers.
Hemodynamic Principles of the Fontan Circulation and lts Consequences
The hemodynamic principle of the Fontan operation is to separate the systemic circulation from the pulmonary circulation by connecting the systemic venous circulation directly to the pulmonary circulation.In the absence of a pumping chamber to the pulmonary circulation, the pulmonary fl ow relies on the differential pressure gradient between the central systemic veins and left atrial pressure,along with low PVR [10].The systemic ventricle acts as a suction pump during diastole, adding to the forward driving force, emphasizing the importance of ventricular diastolic function in the Fontan circulation [11].Spontaneous respiration also plays a role through the negative intrathoracic pressure generated during inspiration; therefore positive pressure ventilation is usually poorly tolerated in Fontan patients.
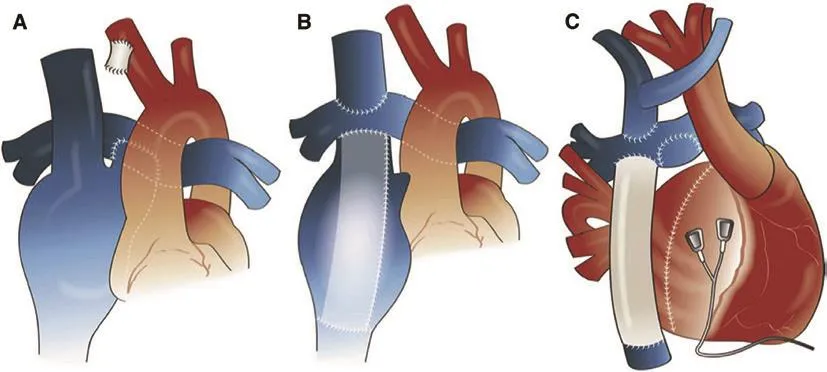
Figure 1 Variations of the Fontan Operation.
The main hemodynamic sequelae of the Fontan operation are systemic venous hypertension and chronic low cardiac output.The underlying cause of low cardiac output is multifactorial, and it can occur despite normal single ventricular dysfunction.The causes include (1) elevation in systemic venous pressures, (2) passive pulmonary blood fl ow reliant on low pulmonary vascular resistance, which in the absence of a subpulmonary ventricle limits the preload reserve and the ability of the single ventricle to augment cardiac output in response to higher metabolic demands, and (3) the inability to augment heart rate in many patients because of underlying sinus node dysfunction [10, 12].
This chronic state of low cardiac output leads to hepatic venous hypertension, elevation of pressures in the thoracic duct with a potential risk of prolonged chylous effusion in the early post-Fontan period, and development of plastic bronchitis and PLE at long-term follow-up [13, 14].
Cardiac Performance During Exercise
Exercise performance in patients with a Fontan circulation is decreased because of inadequate augmentation of cardiac output.This is due to a variety of factors, including blunted heart rate response from sinus node dysfunction, lack of a subpulmonary pumping chamber, abnormal pulmonary vasculature adaptation to exercise, and inadequate preload reserve.
Cardiopulmonary exercise testing provides valuable information as a predictor for various adverse events, with peak oxygen uptake (Vo2max)reported as an independent predictor for death and morbidity [15–18].Ohuchi et al.[17] reported a cutoff value of 21 mL/kg/min for Vo2max (corresponding to 49% of the predicted value for age)as a strong predictor for mortality.Recent studies have suggested that serial cardiopulmonary exercise testing could add significant value in routine evaluation of exercise tolerance in Fontan patients as well as in risk stratification for clinical outcomes [19].
Long-term Complications and Management Strategies
With advances in surgical, catheter, and medical therapies, the survival rates of patients undergoing the Fontan operation have increased dramatically over time.As many patients are now surviving to adulthood, there is growing interest in studying the long-term functional status and prevalence of late morbidities specific to the Fontan circulation.In a systemic review by Alsaied et al.[20] of 6700 Fontan patients with an average follow-up of 8 years, the most common cardiac cause of longterm death was heart failure, including Fontan failure (22% of late deaths), followed by arrhythmia/sudden death (16%), and the most common noncardiac causes were respiratory failure (15%) and renal diseases (12%).The rate of freedom from death or transplant has been reported to be 90% at 10 years,83% at 20 years, and 70% at 25 years [21], and the 30-year survival rate has been reported as 43% [22].Some reported predictors of adverse outcomes include impaired preoperative ventricular function,pulmonary artery pressure greater than 15 mmHg,atrioventricular valve (AVV) regurgitation before Fontan completion, AVV replacement at the time of the Fontan procedure, heterotaxy syndrome,pacemaker implantation, including in patients in nonsinus rhythm before Fontan palliation, older age at the time of the operation (>7 years), hypoplastic left-sided heart syndrome, and APC Fontan procedure [22–27].
Cardiovascular-Related Complications
Arrhythmia/Sudden Death
Development of early and late arrhythmias remains a challenging and extremely common complication after the Fontan operation.The overall incidence of postoperative arrhythmias has been reported to be 48% at an average follow-up of 15.3 ± 9.3 years,while the 20- and 30-year rates of freedom from new-onset arrhythmia are 42% and 24%, respectively [22].The incidence is much higher in APC Fontan patients, with atrial arrhythmias occurring in to 50–60% of these patients [28, 29].The newer modifications of ILT and extracardiac conduit Fontan modifications were introduced with the hope to reduce the arrhythmia burden by improving the fl ow dynamics in the Fontan circuit, and on longterm follow-up the incidence was found to be lower with these newer approaches as compared with the APC Fontan procedure [30, 31].However, there is likely a similar arrhythmia burden when these newer modifications are compared with each other[30].Reported risk factors for increased arrhythmia in Fontan patients include severe branch pulmonary artery stenosis, systemic ventricular end-diastolic pressure greater than 12 mmHg preoperatively,AVV replacement during the Fontan operation, and early postoperative arrhythmia [32].
Intra-atrial reentrant tachycardia is the most common type of supraventricular tachycardia, accounting for 75% of supraventricular tachycardia in these patients [33].Focal atrial tachycardia can also occur in some patients, and atrial fi brillation incidence is increasing as the population ages [34, 35].Patients with single ventricle physiology may present with symptoms of decompensated heart failure, especially those with elevated Fontan pressures and poor ventricular function.Sinus node dysfunction is also commonly seen in patients following the Fontan operation as injury to the sinus node can frequently occur during the surgery [30].Epicardial pacemaker therapy will often be needed, although there is potential for a transvenous atrial lead in APC or ILT Fontan patients.Ventricular arrhythmias account for 5% of the arrhythmias that occur in Fontan patients, and can be seen in patients with poor ventricular function, likely accounting for the incidence of sudden cardiac death [34].Risk factors for sudden cardiac death include AVV replacement at the time of the Fontan operation and Fontan pressures greater than 20 mmHg [32].
A thorough evaluation should be performed in Fontan patients with arrhythmias, especially in patients with frequent atrial arrhythmia or a severer presentation.This may include evaluation of ventricular function, assessment for anatomical connections by cross-sectional imaging, and hemodynamic measurements through cardiac catheterization,with intervention as needed.Cardioversion can be performed in cases of symptomatic rapid conduction, but radiofrequency ablation and long-term medical therapy is often needed in addition [25, 27].Radiofrequency ablation can be helpful in reducing the occurrence of arrhythmia, but because of new reentrant pathways emerging, the recurrence rate is 50% within 4–5 years [34].Although rate control can be an option, most patients are dependent on atrioventricular synchrony to maintain cardiac output and can feel unwell without it.Anticoagulation needs to be initiated in patients with atrial arrhythmias, and careful assessment for thrombosis should be performed.Fontan conversion surgery can be considered in carefully selected cases to treat refractory intra-atrial reentrant tachycardia [36].
Ventricular Dysfunction
Loading conditions on the ventricle throughout the various stages of Fontan palliation can cause structural remodeling (such as dilatation and hypertrophy) and cardiac dysfunction [37].There are limited data supporting the use of medical therapy for ventricular dysfunction in single ventricle patients.Angiotensin-converting enzyme inhibitors and beta-blockers have been shown to have some benef it for systolic dysfunction of the single ventricle,but data are limited [38].Carvedilol has been shown to improve New York Heart Association class and increase ejection fraction in Fontan patients, but use of beta-blockers may be limited by the degree of sinus node dysfunction [39].Diuretic therapy with both loop diuretics and aldosterone antagonists can be used to treat fl uid overload; additionally, aldosterone antagonists may have some positive effect on the pulmonary vascular bed [40].
Maintaining atrioventricular synchrony can be of symptomatic benef it in patients with a single ventricle.Cardiac resynchronization therapy in patients with a single ventricle (multisite pacing) can be considered to improve synchronous ventricular activation and has shown some improvement in cardiac function after surgery [41]; however, long-term data are limited, and usually the technical limitations imposed by the need for thoracotomy for epicardial lead placement makes it a less attractive modality.
Elevated Pulmonary Vascular Resistance
PVR increases with the process of aging, but there are additional factors that contribute to abnormal pulmonary vasculature in the patient following the Fontan operation.A few anatomical subtypes result in pulmonary overcirculation and elevated PVR from a young age due to unobstructed pulmonary blood fl ow or palliative shunts.These patients continue to have changes in the vascular bed, with decreased capillary recruitment and medial hypertrophy even after the Fontan operation [42], resulting in altered nitric oxide synthesis and an increase in endothelin receptor expression [43, 44].Elevated PVR has been associated with Fontan failure and is predictive of death in the population of patients with PLE [37, 38].
Modifying the PVR in Fontan patients to increase cardiac output and exercise capacity has been an attractive hypothesis for many investigators.Mixed results with pulmonary vasodilator medical therapy have been reported [45–48].Van De Bruaene et al.[45] demonstrated that sildenafil increased cardiac index during exercise, with a significant decrease in PVR.Targeting the endothelin 1 system with an endothelin receptor antagonist such as bosentan has been shown to increase Vo2max and improve functional status in the short term [33, 34], although the benef its were not seen after 6 months of therapy [48].Some studies have shown the benef it of spironolactone in combination with endothelin A receptor antagonists to increase exercise capacity in patients with pulmonary arterial hypertension [40].While the effects have been attributed to improved cardiac function and its diuretic properties, spironolactone has also been shown to improve endothelial cell function and reduce inflammation [49].Further multicenter randomized controlled trials are needed to explore the true benef it of pulmonary vasodilator therapy in Fontan patients.
Cyanosis
Pulmonary arteriovenous malformations (AVMs),persistent fenestrations, or the presence of venovenous collaterals (systemic veins–pulmonary veins) can result in persistent cyanosis in the Fontan patient [50].Careful hemodynamic evaluation,including measurement of the Fontan pressures and the degree of shunting across the fenestration,can help identify patients with favorable hemodynamics for closure [51].Pulmonary AVMs are seen commonly in patients who have an isolated Glenn shunt with the lack of inclusion of hepatic venous fl ow into the Fontan circuit or if there is a mechanical obstruction diverting the hepatic venous fl ow from the pulmonary circulation [52, 53].Surgical revision to include hepatic vein fl ow into the Fontan baffle can be performed to treat pulmonary AVMs.Venovenous collaterals can be coiled, but Fontan pressures and patency should be carefully assessed as part of the evaluation [54].
Mechanical or Structural Lesions
Careful assessment for obstruction of the Fontan pathway, pulmonary arteries, and pulmonary veins should be performed by noninvasive imaging such as magnetic resonance imaging (MRI) or cardiac computed tomography.Stenosis or narrowing can potentially be treated in the cardiac catheterization laboratory or operating room.In some cases,the pulmonary veins can be mechanically compressed by the massively enlarged right atrium in an APC Fontan patient [55].Certain anatomical subtypes might also have components of outflow tract obstruction, such as subaortic obstruction, coarctation of the aorta, or stenosis at the sites of neoaortic anastomosis such as in the Norwood operation.Alleviating these obstructions can increase cardiac output.Patients with severe valve regurgitation may need valve replacement if they are symptomatic and showing signs of low cardiac output [56].
Extracardiac Organ System lnvolvement
Fontan-Associated Liver Disease
The liver is one of the main organs affected by the altered hemodynamics of the Fontan circulation.Recent studies have reported approximately 21% of Fontan patients develop cirrhosis [57, 58].Probably the strongest predictor of liver dysfunction is the time since the Fontan operation.Pundi et al.[58]demonstrated that the 10-, 20-, and 30-year rates of freedom from cirrhosis are 99%, 94%, and 57%,respectively.
The cause of Fontan-associated liver disease is likely multifold, with chronic venous congestion/elevated central venous pressures, hypoxia,and decreased cardiac output all playing a role in development [59, 60].Other potential mechanisms include pre-Fontan hypoxemia [61], perioperative liver injury [62], and altered hepatic blood fl ow.
However, it is not evident how long these changes have to exist for significant hepatic dysfunction to occur.Additionally, the diminished portal venous fl ow in the setting of systemic venous hypertension increases the hepatic arterial fl ow, leading to the formation of hypervascular nodules [63].Usually these nodules are benign and reported as focal nodular hyperplasia, but they often raise a concern for hepatocellular malignancy, which has been observed in Fontan patients [64, 65].
The most common histological feature of the liver in Fontan patients is the presence of hepatic fi brosis, which can be either portal or sinusoidal, which is different from other causes of cardiac cirrhosis,where the predominant feature is sinusoidal fi brosis [66, 67].Results from imaging modalities have not corresponded consistently with biopsy results,but ultrasonography, computed tomography, or MRI should be considered for baseline screening and evaluation in these patients [68].Elastography(ultrasonography or MRI) can quantitate the degree of fi brosis noninvasively, but limited data exist in the Fontan population.The imaging modalities could also identify markers for portal hypertension,including splenomegaly and esophageal varices,collateral vessels, including intrahepatic and extrahepatic venovenous collaterals, and portopulmonary venous collaterals.
Regular screening for liver dysfunction could include checking the hepatic panel (alanine aminotransferase, aspartate aminotransferase,γ-glutamyltransferase, prothrombin time, activated partial thromboplastin time, albumin, total protein)and complete blood count (especially platelet count)every year.Usually hepatic function as measured by routine blood parameters is well preserved in these patients [58, 69–71], although mild elevation of indirect bilirubin and alkaline phosphatase levels in addition to decreased platelet levels might be seen in some.All patients should undergo evaluation for hepatitis B and hepatitis C, especially those operated on before routine screening, and it is reasonable to check alpha fetoprotein levels during initial screening in all patients.Vaccination against hepatitis A and hepatitis B should be considered in all Fontan patients.Screening guidelines are being established, but in general, imaging should be performed as a screening tool with frequency determined by the cardiac and hepatology teams.In cases with suspected more advanced liver disease, liver biopsy may be indicated and can be performed through the transjugular or percutaneous approach, simultaneously with cardiac catheterization.Fontan patients should be counseled to avoid hepatic toxins, including alcohol, and to adhere to available preventive measures, including hepatitis vaccination.There are no established screening or treatment protocols,although use of therapies to maximize cardiac output, decrease pulmonary pressures and resistance,and optimize oxygen delivery is a strategy that may delay the progression of disease.
Thromboembolism
Patients after the Fontan operation have been reported to have numerous clotting abnormalities, including deficiencies of protein C, protein S, and antithrombin III, in addition to increased platelet reactivity [64,65].The combination of decreased cardiac output, a nonpulsatile low-flow state to the pulmonary circulation, atrial arrhythmias, and the presence of prosthetic material places these patients at high risk of thrombus formation.The rate of thromboembolism has been reported to be as high as 20% in patients after Fontan completion; for those with extracardiac conduit, it is estimated to be 7.1% at 10 years after Fontan completion [66, 67, 72].Among patients with underlying atrial arrhythmia, the prevalence of thromboembolic complications is 18% and 55% at 5 and 10 years, respectively [73].This can result in pulmonary emboli, acute and chronic; systemic embolithrough patent fenestration or baffle leaks; and systemic thrombi in the atria, pulmonary artery stump,or rudimentary ventricle.Thromboemboli in the pulmonary vasculature can produce acute hemodynamic instability and chronically result in elevated Fontan pressures and increased PVR.Systemic sources of thrombi place the patient at risk of stroke and endorgan system damage.Cerebrovascular events have been reported in 4.1–5.5% of patients; most are embolic in nature [74, 75].
Prophylactic treatment guidelines recommend aspirin, heparin, or vitamin K antagonists,although the efficacy of each has not been well established.In patients with atrial arrhythmia after the Fontan operation, anticoagulation with vitamin K antagonists with or without antiplatelet therapy reduces the risk of thromboembolic complications by 2.5-fold as compared with those not receiving anticoagulation, and is associated with lower risk of death and hospitalization, while the rates of bleeding are similar (at 7%) [73].There is a global ongoing prospective registry (NOTE registry) evaluating the safety of initiation of treatment with novel oral anticoagulants and transition from vitamin K antagonists to novel oral anticoagulants; promising results were shown during the fi rst month [76].
Pulmonary/Plastic Bronchitis
Plastic bronchitis is a debilitating late complication after the Fontan procedure.It is characterized by the formation of casts in the tracheobronchial tree.The exact cause is unknown; it is speculated that it could be related to hypersecretion of mucus in the presence of chronically elevated systemic venous pressure, or lymph leak into the airway [77,78].It is a strong predictor of poor outcome as the onset of plastic bronchitis within 1 year of Fontan surgery is associated with a fi ve-fold increase in mortality rate [77].The risk factors for developing this complication include prolonged chest tube drainage after Fontan surgery, history of chylothorax associated with staged palliation, and history of ascites.Various management strategies have been proposed, including systemic steroids, dornase alfa, inhaled tissue plasminogen activator,and casts removed via bronchoscopy, all of which have only marginal benef it [79, 80].More recently,embolization of pulmonary lymphatics has been shown to be an effective treatment for patients with plastic bronchitis and abnormal pulmonary lymphatic fl ow [81].This is a promising new treatment for a subset of these patients where lymphatic contribution is a basis for the development of plastic bronchitis.Heart transplant for severe plastic bronchitis refractory to medical treatment has a high mortality rate; however, patients who survive the early postoperative period have a resolution of the plastic bronchitis.
Fontan patients are at a risk of other pulmonary complications, also seen in other CHD or non-CHD populations.Airway disease such as ciliary dysfunction has a high prevalence in patients with heterotaxy syndrome.These patients can present with impaired airway clearance, and may require prolonged intubation after the procedure, which can be harmful for a Fontan patient.Any single-ventricle patient with heterotaxy should be evaluated for symptoms of ciliary dysfunction [69].Pulmonary venous desaturation in the absence of venovenous collaterals should prompt a pulmonary evaluation for lung parenchymal disease.
Obstructive sleep apnea, very commonly seen in the general population, can also raise pulmonary pressures, increase PVR in Fontan patients, and increase the risk of refractory atrial arrhythmias[82].While continuous positive airway pressure may seem harmful for the Fontan physiology, the rise in pressure during periodic obstruction causes greater alterations in Fontan fi lling and rise in Fontan pressure.Untreated sleep apnea can alter endothelial function, further compounding the vascular changes.Screening for sleep apnea in Fontan patients should be performed when clinically indicated [83].Finally, restrictive lung disease from prior surgery, scoliosis, and obesity is very common in the adult CHD population and places these patients at higher risk of elevated PVR and impaired fi lling of the Fontan pathway.Cardiopulmonary rehabilitation may be needed for respiratory muscle training to help relieve symptoms and increase forced vital capacity [84].
Chronic Venous lnsufficiency
Chronic venous insuf fi ciency (CVI) is associated with chronic pain, decreased physical function,social isolation, and depression.It is usually graded according to a scale describing clinical, etiological,anatomical, and pathophysiological (CEAP) classifications [85, 86].The prevalence of CVI is twice as high in Fontan patients compared with the general population [87], with 22% of Fontan patients having severe venous insufficiency (CEAP grade ≥4).The cause of CVI in Fontan patients is due to underlying systemic venous hypertension on distention and engorgement of the veins with induction of inflammation in the vascular wall and venous valves,leading to loss of function of the venous valves and reflux [88, 89].
Renal Failure
Renal failure has been demonstrated as one of the predictors of late death in Fontan patients, with a hazard ratio of 2.5 [22].There are limited data on the prevalence and exact pathology of renal dysfunction in Fontan patients.Anne et al.[90] reported the presence of microalbuminuria in a small cohort of Fontan patients, defined as albumin/creatinine ratio greater than 20 μg/mg.Microalbuminuria is usually an early indicator of glomerulopathy, and in diabetic patients corresponds to increase in cardiovascular morbidity and mortality [91].The renal injury in Fontan patients is likely related to the elevated central venous pressure with its effect in increasing the efferent arteriolar pressure.Renal hypoperfusion, due to decrease cardiac output, could also be a contributing factor through decreasing the afferent arteriolar pressure, analogous to the pathophysiology encountered in Fontan-associated liver disease.Other potential mechanisms include the effect of cardiopulmonary bypass injury [92].The use of angiotensin-converting enzyme inhibitors may be beneficial in preserving the renal function in these patients.Further studies are required to explore the prevalence, pathophysiology, and management of renal dysfunction in Fontan patients.
Protein-Losing Enteropathy
PLE is a rare complication that occurs in cardiac diseases where there are chronically elevated systemic venous pressures, such as constrictive pericarditis,long-standing congestive heart failure, and after the Fontan operation [93, 94].The exact pathophysiology is unknown, although it is hypothesized that elevated systemic venous pressures in the superior vena cava lead to disturbed thoracic duct drainage, with increase in the lymphatic system pressures, resulting in intestinal protein loss.Moreover, inflammatory response caused by chronic lymphatic congestion and chronic protein leakage from the lymphatics could contribute.PLE occurs in 5–15% of patients after the modified Fontan operation, and has been historically a difficult complication to treat [95, 96].It is characterized by the enteric loss of proteins such as albumin, immunoglobulins, and clotting factors, leading to the clinical findings of peripheral edema, ascites,diarrhea, weight loss, and malabsorption.Diagnosis is obtained through measurement of serum total protein and serum albumin level.Gastrointestinal protein loss can be assessed by measurement of α1-antitrypsin level in the stool [97].PLE is usually a marker of poor prognosis, with 50% mortality at 5 years after initial diagnosis, although more recent reports have shown an increased survival rate likely related to advances in management strategies [95,98, 99].Patients with Fontan pressures greater than 15 mmHg at the time of diagnosis of PLE had lower 5- and 10-year survival rates (83% and 63%, respectively) compared with patients with Fontan pressures lower than 15 mmHg (95% and 86%, respectively).Additional factors seen with increased mortality are lower cardiac index, decreased ventricular function,elevated PVR, lower mixed venous saturation, New York Heart Association class greater than II, and higher serum creatinine level.
There is no reliable therapy for PLE, and management strategies are primarily individualized.A thorough evaluation should be performed on any Fontan patient with PLE or failing physiology.A suggested evaluation is detailed in Table 1.A treatment algorithm for PLE in Fontan patients has been outlined,and primarily involves the combination of intestinal directed therapies and cardiac and extracardiac directed therapies [99].The proposed mechanisms of benef it from dietary and medical therapies are outlined in Table 2 [101–103].Surgical and interventional therapies include creation of fenestration to decrease the Fontan pressures but at the expense of accepting a degree of cyanosis [103].Patients should be considered for anticoagulation after fenestration because they are at higher risk of embolic phenomena.Data on the impact of heart transplant on PLE are limited; however, resolution of PLE symptoms after transplant has been documented, with similar morbidity and mortality after transplant as compared with patients without PLE [99, 104, 105].More recently, lymphatic embolization has been shown to be effective in increasing albumin levels and reducing symptoms [106].
Fontan Failure
Fontan failure is a complex clinical syndrome that includes some physiological phenotypes in addition to the traditional acquired heart failuredefinitions of “heart failure with preserved ejection fraction” and “heart failure with reduced ejection fraction” [107].As discussed earlier,even in the presence of preserved systemic ventricle function, patients after the Fontan operation are in a chronic state of low cardiac output.The long-term consequences of this circulation affect many organs systems, as described in detail earlier.However, the organ systems in individual patients are affected differently, and to variable extents.These multiorgan complications contribute to the diverse phenotypes of Fontan failure.After anatomical issues contributing to Fontan failure have been ruled out, four phenotypes of Fontan failure have been described on the basis of the underlying hemodynamics [107].The characteristics of Fontan failure may change over time,and therapies should be directed on the basis of individual phenotypes.Clinical response to treatment usually differs depending on the type of phenotype the patient is experiencing.
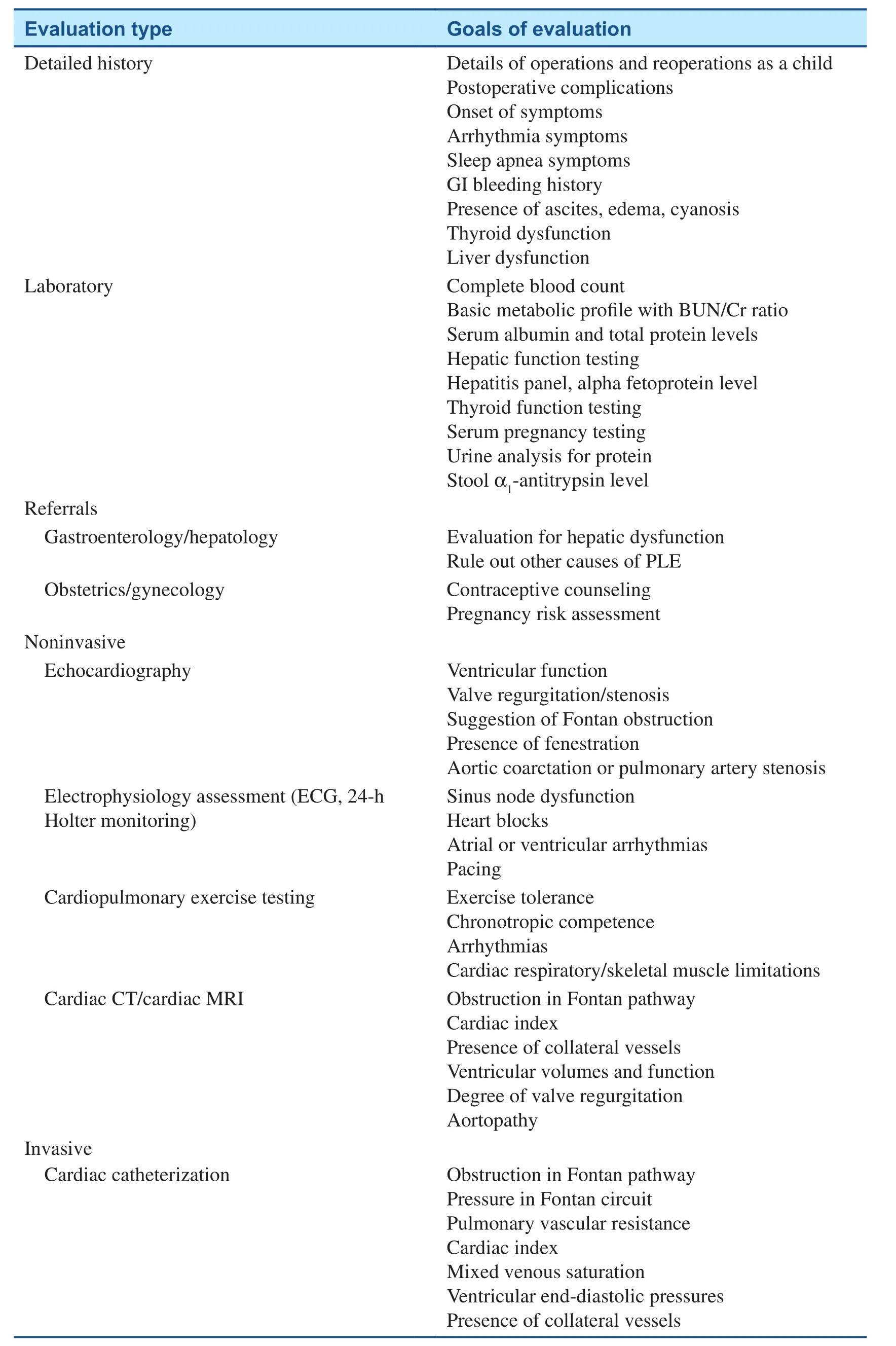
Table 1 Evaluation of Adults with Fontan Palliation.

Table 2 Proposed Mechanism of Benef it of Medical Therapies for Protein-Losing Enteropathy (PLE).
Consideration for Transplantation
While survival has continued to improve in the Fontan population, heart transplant is still reserved for patients after all other medical and surgical therapies have failed.The survival rate has increased overall, although it is still significantly lower in than the general population without CHD [108, 109].Unfortunately, death while on the waiting list or delisting because of worsening clinical status is disproportionately common for adult CHD patients [110].An additional challenge is that many Fontan patients also have high panel reactive antibody levels because of previous blood transfusions and procedures that markedly increase the risk of rejection.
As part of the transplant workup, it is important to perform a multiorgan system evaluation to assess the patient for liver, kidney, and pulmonary dysfunction.In some cases, the heart transplant needs to be performed in combination with transplant for another failing organ system.While elective cardiac operations using cardiopulmonary bypass are contraindicated in patients with moderate to severe cirrhosis (Child-Pugh class B and C), an earlier stage of liver injury tends to be reversible after heart transplant, and in itself is not considered a contraindication for heart transplant [111].Combined heart and liver transplant should thus be considered in patients with irreversible liver disease.However,it is still unknown what criteria should be used to determine when the hepatic changes will be reversible after heart transplant.
Despite all these challenges, the post–heart transplant survival rate for Fontan patients at 1, 5, and 10 years in an Australian and New Zealand Fontan registry [112] was 91%, 78%, and 71%, respectively.Compared with other patients with CHD (n= 87),Fontan patients had similar in-hospital outcomes and long-term survival.Similarly, a Mayo study showed overall 1-, 5-, 10-, and 15-year posttransplant survival rates of 80%, 72%, 69%, and 55%, respectively (in 44 of 1138 Fontan patients, 27% had PLE), suggesting that heart transplant remains a reasonable option for patients with a failed Fontan circulation [113].
The use of ventricular assist devices has gained increasing attention over the past few years.Devices have been used both as a subpulmonary pump to drive blood forward through the pulmonary circuit and also in the standard systemic ventricular position to pull blood through the Fontan circuit by lowering the left atrial pressure [114, 115].Placement of the device may be dependent on the underlying hemodynamics: systemic ventricular failure versus elevation of PVR.Further investigation of ideal device strategies and prototypes is needed as ventricular assist device therapy has the potential to not only serve as a bridge to transplant but as eventual destination therapy for this complex cohort of patients.
Pregnancy in Fontan Patients
With the increase in survival among Fontan patients,more women are reaching the reproductive age group and expressing interest in having children;therefore there has been growing interest in developing risk scores that could predict maternal and neonatal outcomes during pregnancy and at longterm follow-up.Although the existing risk scoring models (CAPREG, ZAHARA, WHO) are helpful,they are not specific and do not take into account the physiological and hemodynamic considerations of the Fontan patient.Preconception evaluation of the Fontan patient should take into account the ventricular function, degree of AVV regurgitation, functional capacity, arrhythmia burden, and any other potential comorbidities, including liver disease, renal disease,and history of thromboembolic events.Care during pregnancy should be provided by a multidisciplinary team including an adult CHD specialist, a high-risk obstetrician, and anesthesia specialists with expertise and experience in managing such complex patients.Although increasing data have been accumulating on the outcomes of pregnant Fontan women, the evidence in this area is still limited to a very small number of patients in the studies.In a multicenter observational study by Gouton et al.[116], the incidence of cardiovascular events during pregnancy was 10% (6 of the 59 pregnancies), with atrial arrhythmia being the most common (three patients), followed by thromboembolic events (two patients).Fetal loss was seen in 34% patients (27% were miscarriages), and among women who completed pregnancy, prematurity (69%) was the most common neonatal complication.There was no significant worsening of clinical status after a median follow-up of 24 months.
Anticoagulation of the Fontan patient during pregnancy is clearly indicated in the presence of atrial thrombus, atrial arrhythmia, or a history of thromboembolic events; however, there is no evidence for the benef it of routine use of prophylactic anticoagulation (recommendation class IIa, level of evidence C) [117].
Conclusions
With recent advances in surgical techniques and medical management, long-term survival after the Fontan operation has significantly improved.However, there are numerous long-term complications, including Fontan failure, arrhythmia, premature cardiac death, liver disease, PLE, and need for reoperation.As more patients survive to adulthood,innovative management strategies to maintain quality of life and extend life expectancy are needed.
Conflict of lnterest
The authors declare that they have no conflicts of interest.
REFERENCES
1.Fontan F, Baudet E.Surgical repair of tricuspid atresia.Thorax 1971;26(3):240–8.
2.de Leval MR, Kilner PJ, Gewillig M, Bull C.Total cavopulmonary connection: a logical alternative to atriopulmonary connection for complex Fontan operations.J Thorac Cardiovasc Surg 1988;96(5):682–95.
3.Marcelletti C, Corno A, Giannico S,Marino B.Inferior vena cavapulmonary artery extracardiac conduit.A new form of right heart bypass.J Thorac Cardiovasc Surg 1990;100(2):228–32.
4.Khairy P, Poirier N, Mercier L.Univentricular heart.Circulation 2007;115:800–12.
5.Bridges ND, Mayer JE, Lock JE,Jonas RA, Hanley FL, Keane JF,et al.Effect of baffle fenestration on outcome of the modified Fontan operation.Circulation 1992;86(6):1762–9.
6.Bridges ND, Lock JE, Castaneda AR.Baffle fenestration with subsequent transcatheter closure.Modification of the Fontan operation for patients at increased risk.Circulation 1990;82(5):1681–9.
7.Ono M, Boethig D, Goerler H,Lange M, Westhoff-Bleck M,Breymann T.Clinical outcome of patients 20 years after Fontan operation – effect of fenestration on late morbidity.Eur J Cardiothorac Surg 2006;30:923–9.
8.Monagle P, Karl TR.Thromboembolic problems after the Fontan operation.Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 2002;5(1):36–47.
9.Kaulitz R, Ziemer G, Paul T, Peuster M, Bertram H, Hausdorf G.Fontantype procedures: residual lesions and late interventions.Ann Thorac Surg 2002;74(3):778–85.
10.Senzaki H, Masutani S, Ishido H,Taketazu M, Kobayashit, Sasaki N, et al.Cardiac rest and reserve function in patients with Fontan circulation.J Am Coll Cardiol 2006;47(12):2528–35.
11.Frommelt PC, Snider AR, Meliones JN, Vermilion RP.Doppler assessment of pulmonary artery fl ow patterns and ventricular function after the Fontan operation.Am J Cardiol 1991;68(11):1211–5.
12.Piran S, Veldtman G, Siu S,Webb GD, Liu PP.Heart failure and ventricular dysfunction in patients with single or systemic right ventricles.Circulation 2002;105(10):1189–94.
13.Akbari Asbagh P, Navabi Shirazi MA, Soleimani A, Razzaz M,Akbari Asbagh N, Rayatzadeh H,et al.Incidence and etiology of chylothorax after congenital heart surgery in children.J Tehran Heart Cent 2014;9(2):59–63.
14.Salman S, Drinkwater DC,Christian KG.Plastic bronchitis:is thoracic duct ligation a real surgical option? Ann Thorac Surg 2006;81(6):2281–3.
15.Diller G-P, Dimopoulos K, Okonko D, Li W, Babu-Narayan SV, Broberg CS, et al.Exercise intolerance in adult congenital heart disease: comparative severity, correlates, and prognostic implication.Circulation 2005;112(6):828–35.
16.Diller GP, Giardini A, Dimopoulos K, Gargiulo G, Müller J, Derrick G,et al.Predictors of morbidity and mortality in contemporary Fontan patients: results from a multicenter study including cardiopulmonary exercise testing in 321 patients.Eur Heart J 2010;31(24):3073–83.
17.Ohuchi H, Negishi J, Noritake K,Hayama Y, Sakaguchi H, Miyazaki A, et al.Prognostic value of exercise variables in 335 patients after the Fontan operation: a 23-year single-center experience of cardiopulmonary exercise testing.Congenit Heart Dis 2015;10(2):105–16.
18.Cunningham JW, Nathan AS,Rhodes J, Shafer K, Landzberg MJ,Opotowsky AR.Decline in peak oxygen consumption over time predicts death or transplantation in adults with a Fontan circulation.Am Heart J 2017;189:184–92.
19.Egbe AC, Driscoll DJ, Khan AR,Said SS, Akintoye E, Berganza FM, et al.Cardiopulmonary exercise test in adults with prior Fontan operation: the prognostic value of serial testing.Int J Cardiol 2017;235:6–10.
20.Alsaied T, Bokma JP, Engel ME,Kuijpers JM, Hanke SP, Zuhlke L,et al.Factors associated with longterm mortality after Fontan procedures: a systematic review.Heart 2017;103(2):104–10.
21.Khairy P, Fernandes SM, Mayer JE,Triedman JK, Walsh EP, Lock JE,et al.Long-term survival, modes of death, and predictors of mortality in patients with Fontan surgery.Circulation 2008;117(1):85–92.
22.Pundi KN, Johnson JN, Dearani JA, Pundi KN, Li Z, Hinck CA,et al.Forty Year follow-up after the Fontan operation: long-term outcomes of 1,052 patients.J Am Coll Cardiol 2015;66(15):1700–10.
23.Hosein RBM, Clarke AJB, McGuirk SP, Griselli M, Stumper O, De Giovanni JV, et al.Factors influencing early and late outcome following the Fontan procedure in the current era.The “two commandments”? Eur J Cardiothorac Surg 2007;31(3):344–53.
24.D’Udekem Y, Xu MY, Galati JC,Lu S, Iyengar AJ, Konstantinov IE, et al.Predictors of survival after single-ventricle palliation:the impact of right ventricular dominance.J Am Coll Cardiol 2012;59(13):1178–85.
25.Nakano T, Kado H, Tatewaki H,Hinokiyama K, Oda S, Ushinohama H, et al.Results of extracardiac conduit total cavopulmonary connection in 500 patients.Eur J Cardiorhorac Surg 2015;48(6):825–32.
26.Iyengar AJ, Winlaw DS, Galati JC,Wheaton GR, Gentles TL, Grigg LE, et al.The extracardiac conduit Fontan procedure in Australia and New Zealand: hypoplastic left heart syndrome predicts worse early and late outcomes.Eur J Cardiothorac Surg 2014;46(3):465–73.
27.Fontan F, Kirklin JW, Fernandez G, Costa F, Naftel DC, Tritto F,et al.Outcome after a “perfect”Fontan operation.Circulation 1990;81(5):1520–36.
28.Collins KK.The spectrum of longterm electrophysiologic abnormalities in patients with univentricular hearts.Congenit Heart Dis 2009;4(5):310–7.
29.Giannakoulas G, Dimopoulos K, Yuksel S, Inuzuka R, Pijuan-Domenech A, Hussain W, et al.Atrial tachyarrhythmias late after Fontan operation are related to increase in mortality and hospitalization.Int J Cardiol 2012;157(2):221–6.
30.Lee JR, Kwak J, Kim KC, Min SK, Kim WH, Kim YJ, et al.Comparison of lateral tunnel and extracardiac conduit Fontan procedure.Interact Cardiovasc Thorac Surg 2007;6(3):328–30.
31.Stamm C, Friehs I, Mayer JE,Zurakowski D, Triedman JK,Moran AM, et al.Long-term results of the lateral tunnel Fontan operation.J Thorac Cardiovasc Surg 2001;121(1):28–41.
32.Pundi KN, Pundi KN, Johnson JN, Dearani JA, Li Z, Driscoll DJ,et al.Sudden cardiac death and late arrhythmias after the Fontan operation.Congenit Heart Dis 2017;12(1):17–23.
33.Mondesert B, Marcotte F, Mongeon FP, Dore A, Mercier LA, Ibrahim R, et al.Fontan circulation: success or failure? Can J Cardiol 2013;29(7):811–20.
34.Deal BJ.Late arrhythmias following Fontan surgery.World J Pediatr Congenit Heart Surg 2012;3(2):194–200.
35.Stephenson EA, Lu M, Berul CI,Etheridge SP, Idriss SF, Margossian R, et al.Arrhythmias in a contemporary Fontan cohort: prevalence and clinical associations in a multicenter cross-sectional study.J Am Coll Cardiol 2010;56(11):890–6.
36.Deal BJ, Costello JM, Webster G,Tsao S, Backer CL, Mavroudis C.Intermediate-term outcome of 140 consecutive Fontan conversions with arrhythmia operations.Ann Thorac Surg 2016;101(2):717–24.
37.Gewillig M, Brown SC.The Fontan circulation after 45 years:update in physiology.Heart 2016;102(14):1081–6.
38.Shaddy RE, Boucek MM, Hsu DT,Boucek RJ, Canter CE, Mahony L,et al.Carvedilol for children and adolescents with heart failure: a randomized controlled trial.J Am Med Assoc 2007;298(10):1171–9.
39.Ishibashi N, Park IS, Takahashi Y,Nishiyama M, Murakami Y, Mori K, et al.Effectiveness of carvedilol for congestive heart failure that developed long after modified Fontan operation.Pediatr Cardiol 2006;27(4):473–5.
40.Maron BA, Opotowsky AR,Landzberg MJ, Loscalzo J, Waxman AB, Leopold JA.Plasma aldosterone levels are elevated in patients with pulmonary arterial hypertension in the absence of left ventricular heart failure: a pilot study.Eur J Heart Fail 2013;15(3):277–83.
41.Sojak V, Mazic U, Cesen M,Schrader J, Danojevic N.Cardiac resynchronization therapy for the failing Fontan patient.Ann Thorac Surg 2008;85(6):2136–8.
42.Presson RG, Baumgartner WA,Peterson AJ, Glenny RW, Wagner WW.Pulmonary capillaries are recruited during pulsatile fl ow.J Appl Physiol 2002;92(3):1183–90.
43.Busse R, Fleming I.Pulsatile stretch and shear stress: physical stimuli determining the production of endothelium-derived relaxing factors.J Vasc Res 1998;35(2):73–84.
44.Ishida H, Kogaki S, Ichimori H, Narita J, Nawa N, Ueno T,et al.Overexpression of endothelin-1 and endothelin receptors in the pulmonary arteries of failed Fontan patients.Int J Cardiol 2012;159(1):34–9.
45.Van De Bruaene A, La Gerche A,Claessen G, De Meester P, Devroe S,Gillijns H, et al.Sildenafil improves exercise hemodynamics in Fontan patients.Circ Cardiovasc Imaging 2014;7(2):265–73.
46.Hebert A, Mikkelsen UR, Thilen U, Idorn L, Jensen AS, Nagy E,et al.Bosentan improves exercise capacity in adolescents and adults after Fontan operation: the TEMPO(treatment with endothelin receptor antagonist in Fontan patients,a randomized, placebo-controlled,double-blind study measuring peak oxygen consumption) study.Circulation 2014;130(23):2021–30.
47.Derk G, Houser L, Miner P, Williams R, Moriarty J, Finn P, et al.Efficacy of endothelin blockade in adults with Fontan physiology.Congenit Heart Dis 2015;10(1):E11–6.
48.Schuuring MJ, Vis JC, Van Dijk APJ, van Melle JP, Vliegen HW,Pieper PG, et al.Impact of bosentan on exercise capacity in adults after the Fontan procedure: a randomized controlled trial.Eur J Heart Fail 2013;15(6):690–8.
49.Elinoff JM, Rame JE, Forf i a PR,Hall MK, Sun J, Gharib AM, et al.A pilot study of the effect of spironolactone therapy on exercise capacity and endothelial dysfunction in pulmonary arterial hypertension: study protocol for a randomized controlled trial.Trials 2013;14:91.
50.Vyas H, Driscoll DJ, Cabalka AK, Cetta F, Hagler DJ.Results of transcatheter Fontan fenestration to treat protein losing enteropathy.Catheter Cardiovasc Interv 2007;69(4):584–9.
51.Goff DA, Blume ED, Gauvreau K, Mayer JE, Lock JE, Jenkins KJ.Clinical outcome of fenestrated Fontan patients after closure: the fi rst 10 years.Circulation 2000;102(17):2094–9.
52.Kavarana M, Jones J, Stroud RE,Bradley S, Ikonomidis JS, Mukherjee R.Pulmonary arteriovenous malformations after the superior cavopulmonary shunt: mechanisms and clinical implications.Expert Rev Cardiovasc Ther 2015;12(6):703–13.
53.Masura J, Borodacova L, Tittel P,Berden P, Podnar T.Percutaneous management of cyanosis in Fontan patients using Amplatzer occluders.Catheter Cardiovasc Interv 2008;71(6):843–9.
54.Magee AG, McCrindle BW, Mawson J, Benson LN, Williams WG,Freedom RM.Systemic venous collateral development after the bidirectional cavopulmonary anastomosis:orevalence and predictors.J Am Coll Cardiol 1998;32(2):502–8.
55.O’Donnell CP, Lock JE, Powell AJ,Perry SB.Compression of pulmonary veins between the left atrium and the descending aorta.Am J Cardiol 2003;91(2):248–51.
56.Menon SC, Dearani JA, Cetta F.Long-term outcome after atrioventricular valve surgery following modified Fontan operation.Cardiol Young 2011;21(1):83–8.
57.Baek JS, Bae EJ, Ko JS, Kim GB,Kwon BS, Lee SY, et al.Late hepatic complications after Fontan operation; non-invasive markers of hepatic fi brosis and risk factors.Heart 2010;96(21):1750–5.
58.Pundi K, Pundi KN, Kamath PS,Cetta F, Li Z, Poterucha JT, et al.Liver disease in patients after the Fontan operation.Am J Cardiol 2016;117(3):456–60.
59.Mori M, Aguirre AJ, Elder RW,Kashkouli A, Farris AB, Ford RM,et al.Beyond a broken heart: circulatory dysfunction in the failing Fontan.Pediatr Cardiol 2014;13(1):569–79.
60.Rychik J.Forty years of the Fontan operation: a failed strategy.Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 2010;13(1):96–100.
61.Ghosh ML, Emery JL.Hypoxia and asymmetrical fi brosis of the liver in children.Gut 1973;14(3):209–12.
62.Matsuda H, Covino E, Hirose H,Nakano S, Kishimoto H, Miyamoto Y, et al.Acute liver dysfunction after modified Fontan operation for complex cardiac lesions.Analysis of the contributing factors and its relation to the early prognosis.J Thorac Cardiovasc Surg 1988;96:219–26.
63.Bryant T, Ahmad Z, Millward-Sadler H, Burney K, Stedman B,Kendall T, et al.Arterialised hepatic nodules in the Fontan circulation:hepatico-cardiac interactions.Int J Cardiol 2011;151(3):268–72.
64.Ghaferi AA, Hutchins GM.Progression of liver pathology in patients undergoing the Fontan procedure: chronic passive congestion, cardiac cirrhosis, hepatic adenoma, and hepatocellular carcinoma.J Thorac Cardiovasc Surg 2005;129(6):1348–52.
65.Wallihan DB, Podberesky DJ.Hepatic pathology after Fontan palliation: spectrum of imaging findings.Pediatr Radiol 2013;43(3):330–8.
66.Johnson JA, Cetta F, Graham RP,Smyrk TC, Driscoll DJ, Phillips SD, et al.Identifying predictors of hepatic disease in patients after the Fontan operation: a postmortem analysis.J Thorac Cardiovasc Surg 2013;146(1):140–5.
67.Schwartz MC, Sullivan L, Cohen MS, Russo P, John AS, Guo R, et al.Hepatic pathology may develop before the Fontan operation in children with functional single ventricle: an autopsy study.J Thorac Cardiovasc Surg 2012;143:904–9.
68.Kendall TJ, Stedman B, Hacking N,Haw M, Vettukattill JJ, Salmon AP,et al.Hepatic fi brosis and cirrhosis in the Fontan circulation: a detailed morphological study.J Clin Pathol 2008;61(4):504–8.
69.van Nieuwenhuizen RC, Peters M,Lubbers LJ, Trip MD, Tijssen JG,Mulder BJ.Abnormalities in liver function and coagulation profile following the Fontan procedure.Heart 1999;82(1):40–6.
70.Kaulitz R, Luhmer I, Bergmann F,Rodeck B, Hausdorf G.Sequelae after modified Fontan operation: postoperative haemodynamic data and organ function.Heart 1997;78(2):154–9.
71.Guha IN, Bokhandi S, Ahmad Z,Sheron N, Cope R, Marshall C,et al.Structural and functional uncoupling of liver performance in the Fontan circulation.Int J Cardiol 2013;164(1):77–81.
72.Elder RW, McCabe NM, Hebson C, Veledar E, Romero R, Ford RM,et al.Features of portal hypertension are associated with major adverse events in Fontan patients:the VAST study.Int J Cardiol 2013;168(4):3764–9.
73.Egbe AC, Connolly HM, McLeod CJ,Ammash NM, Niaz T, Yogeswaran V, et al.Thrombotic and embolic complications associated with atrial arrhythmia after Fontan operation:role of prophylactic therapy.J Am Coll Cardiol 2016;68(12):1312–9.
74.Hoffmann A, Chockalingam P,Balint OH, Dadashev A, Dimopoulos K, Engel R, et al.Cerebrovascular accidents in adult patients with congenital heart disease.Heart 2010;96(15):1223–6.
75.Chun DS, Schamberger MS,Flaspohler T, Turrentine MW, Brown JW, Farrell AG, et al.Incidence,outcome, and risk factors for stroke after the Fontan procedure.Am J Cardiol 2004;93(1):117–9.
76.Yang H, Bouma BJ, Mulder BJM;Non vitamin K antagonist Oral anticoagulants for ThromboEmbolic prevention in adult congenital heart disease (NOTE) investigators.Is initiating NOACs for atrial arrhythmias safe in adults with congenital heart disease? Cardiovasc Drugs Ther 2017;31(4):413–7.
77.Schumacher KR, Singh TP, Kuebler J, Aprile K, O’Brien M, Blume ED.Risk factors and outcome of Fontanassociated plastic bronchitis: a casecontrol study.J Am Heart Assoc 2014;3(2):1–7.
78.Languepin J, Scheinmann P, Mahut B, Le Bourgeois M, Jaubert F,Brunelle F, et al.Bronchial casts in children with cardiopathies:the role of pulmonary lymphatic abnormalities.Pediatr Pulmonol 1999;28(5):329–36.
79.Lubcke NL, Nussbaum VM,Schroth M.Use of aerosolized tissue plasminogen activator in the treatment of plastic bronchitis.Ann Pharmacother 2013;47(3):e13.
80.Gibb E, Blount R, Lewis N,Nielson D, Church G, Jones K,et al.Management of plastic bronchitis with topical tissue-type plasminogen activator.Pediatrics 2012;130(2):e446–50.
81.Itkin MG, McCormack FX, Dori Y.Diagnosis and treatment of lymphatic plastic bronchitis in adults using advanced lymphatic imaging and percutaneous embolization.Ann Am Thorac Soc 2016;13(10):1689–96.
82.Watson NF, Stout K.Management of obstructive sleep apnea in patients with congenital heart disease and Fontan procedures.Sleep Med 2007;8(5):537–8.
83.Watson NF, Bushnell T, Jones TK, Stout K.A novel method for the evaluation and treatment of obstructive sleep apnea in four adults with complex congenital heart disease and Fontan repairs.Sleep Breath 2009;13(4):421–4.
84.Ginde S, Bartz PJ, Hill GD,Danduran MJ, Biller J, Sowinski J, et al.Restrictive lung disease is an independent predictor of exercise intolerance in the adult with congenital heart disease.Congenit Heart Dis 2013;8(3):246–54.
85.Eklöf B, Rutherford RB, Bergan JJ,Carpentier PH, Gloviczki P, Kistner RL, et al.Revised CEAP classification for chronic venous disorders:consensus statement.Phlebologie 2005;34(4):220–5.
86.Porter JM, Moneta GL, International Consensus Committee on Chronic Venous Disease.Reporting standards in venous disease: an update.J Vasc Surg 1995;21(4):635–45.
87.Valente AM, Bhatt AB, Cook S, Earing MG, Gersony DR,Aboulhosn J, et al.The CALF(Congenital Heart Disease in Adults Lower Extremity Systemic Venous Health in Fontan Patients)study.J Am Coll Cardiol 2010;56(2):144–50.
88.Takase S, Pascarella L, Bergan JJ, Schmid-Schönbein GW.Hypertension-induced venous valve remodeling.J Vasc Surg 2004;39(6):1329–34.
89.Takase S, Pascarella L, Lerond L,Bergan JJ, Schmid-Schönbein GW.Venous hypertension, inflammation and valve remodeling.Eur J Vasc Endovasc Surg 2004;28(5):484–93.
90.Anne P, Du W, Mattoo TK,Zilberman MV.Nephropathy in patients after Fontan palliation.Int J Cardiol 2009;132(2):244–7.
91.Dinneen SF, Gerstein HC.The association of microalbuminuria and mortality in non-insulin-dependent diabetes mellitus.A systematic overview of the literature.Arch Intern Med 1997;157(13):1413–8.
92.Rigden SP, Barratt TM, Dillon MJ,De Leval M, Stark J.Acute renal failure complicating cardiopulmonary bypass surgery.Arch Dis Child 1982;57(6):425–30.
93.Nelson DL, Blaese RM, Strober W, Bruce RM, Waldmann TA.Constrictive pericarditis, intestinal lymphangiectasia, and reversible immunologic deficiency.J Pediatr 1975;86(4):548–54.
94.Meijers BKI, Schalla S, Eerens F,Van Suylen RJ, Broers B, Cheriex EM, et al.Protein-losing enteropathy in association with constrictive pericarditis.Int J Cardiovasc Imaging 2006;22(3–4):389–92.
95.Mertens L, Hagler DJ, Sauer U,Somerville J, Gewillig M.Proteinlosing enteropathy after the Fontan operation: an international multicenter study.J Thorac Cardiovasc Surg 1998;115(5):1063–73.
96.Crupi G, Locatelli G, Tiraboschi R.Protein-losing enteropathy after Fontan operation for tricuspid atresia (imperforate tricuspid valve).Thorac Cardiovasc Surg 1980;28(5):354–63.
97.Thorne SA, Hooper J, Kemp M,Somerville J.Gastro-intestinal protein loss in late survivors of Fontan surgery and other congenital heart disease.Eur Heart J 1998;19(3):514–20.
98.Driscoll DJ, Offord KP, Feldt RH,Schaff HV, Puga FJ, Danielson GK.Five- to fi fteen-year follow-up after Fontan operation.Circulation 1992;85(2):469–96.
99.John AS, Johnson JA, Khan M,Driscoll DJ, Warnes CA, Cetta F.Clinical outcomes and improved survival in patients with proteinlosing enteropathy after the Fontan operation.J Am Coll Cardiol 2014;64(1):54–62.
100.John AS.Fontan repair of single ventricle physiology: consequences of a unique physiology and possible treatment options.Cardiol Clin 2015;33(4):559–69.
101.John AS, Driscoll DJ, Warnes CA, Phillips SD, Cetta F.The use of oral budesonide in adolescents and adults with protein-losing enteropathy after the Fontan operation.Ann Thorac Surg 2011;92(4):1451–6.
102.John AS, Phillips SD, Driscoll DJ, Warnes CA, Cetta F.The use of octreotide to successfully treat protein-losing enteropathy following the Fontan operation.Congenit Heart Dis 2011;6:653–6.
103.Mertens L, Dumoulin M, Gewillig M.Effect of percutaneous fenestration of the atrial septum on proteinlosing enteropathy after the Fontan operation.Heart 1994;72(6):591–2.
104.Gamba A, Merlo M, Fiocchi R,Terzi A, Mammana C, Sebastiani R, et al.Heart transplantation in patients with previous Fontan operations.J Thorac Cardiovasc Surg 2004;127(2):555–62.
105.Schumacher KR, Gossett J,Guleserian K, Naftel DC, Pruitt E,Dodd D, et al.Fontan associated protein losing enteropathy and heart transplant: a pediatric heart transplant study analysis.J Heart Lung Transplant 2015;34(9):1169–76.
106.Itkin M, Piccoli DA, Nadolski G, Rychik J, DeWitt A, Pinto E,et al.Protein-losing enteropathy in patients with congenital heart disease.J Am Coll Cardiol 2017;69(24):2929–37.
107.Book WM, Gerardin J, Saraf A,Marie Valente A, Rodriguez F.Clinical phenotypes of Fontan failure: implications for management.Congenit Heart Dis 2016;11:296–308.
108.Bernstein D, Naftel D, Chin C,Addonizio LJ, Gamberg P, Blume ED, et al.Outcome of listing for cardiac transplantation for failed Fontan: a multi-institutional study.Circulation 2006;114(4):273–80.
109.Kanter KR, Mahle WT, Vincent RN, Berg AM, Kogon BE,Kirshbom PM.Heart transplantation in children with a Fontan procedure.Ann Thorac Surg 2011;91(3):823–30.
110.Alshawabkeh LI, Hu N, Carter KD,Opotowsky AR, Light-McGroary K, Cavanaugh JE, et al.Wait-list outcomes for adults with congenital heart disease listed for heart transplantation in the U.S.J Am Coll Cardiol 2016;68(9):908–17.
111.Dichtl W, Vogel W, Dunst KM,Grander W, Alber HF, Frick M,et al.Cardiac hepatopathy before and after heart transplantation.Transpl Int 2005;18(6):697–702.
112.Shi WY, Yong MS, McGiffin DC,Jain P, Ruygrok PN, Marasco SF, et al.Heart transplantation in Fontan patients across Australia and New Zealand.Heart 2016;102(14):1120–6.
113.Pundi KN, Pundi K, Driscoll DJ, Dearani JA, Li Z, Dahl SH,et al.Heart transplantation after Fontan: results from a surgical Fontan cohort.Pediatr Transplant 2016;20(8):1087–92.
114.Derk G, Laks H, Biniwale R, Patel S, De LaCruz K, Mazor E, et al.Novel techniques of mechanical circulatory support for the right heart and Fontan circulation.Int J Cardiol 2014;176(3):828–32.
115.Sinha P, Deutsch N, Ratnayaka K,Lederman R, He D, Nuszkowski M, et al.Effect of mechanical assistance of the systemic ventricle in single ventricle circulation with cavopulmonary connection.J Thorac Cardiovasc Surg 2014;147(4):1271–5.
116.Gouton M, Nizard J, Patel M,Sassolas F, Jimenez M, Radojevic J, et al.Maternal and fetal outcomes of pregnancy with Fontan circulation: a multicentric observational study.Int J Cardiol 2015;187(1):84–9.
117.European Society of Gynecology(ESG), Association for European Paediatric Cardiology (AEPC),German Society for Gender Medicine (DGesGM), Regitz-Zagrosek V, Blomstrom Lundqvist C, Borghi C, Cifkova R, Ferreira R, et al.ESC guidelines on the management of cardiovascular diseases during pregnancy: the Task Force on the Management of Cardiovascular Diseases during Pregnancy of the European Society of Cardiology (ESC).Eur Heart J 2011;32(24):3147–97.
杂志排行
Cardiovascular Innovations and Applications的其它文章
- His Bundle Pacing: Rebirth of an lmportant Technique for Pacing the lntrinsic Conduction System
- Depression in Adults with Congenital Heart Disease: Prevalence, Prognosis,and lntervention
- Traditional Chinese Medicine ls Widely Used for Cardiovascular Disease
- D-Transposition of the Great Arteries: A New Era in Cardiology
- Heart Transplantation for Adult Congenital Heart Disease: Overview and Special Considerations
- Atrial Arrhythmias lncluding Atrial Fibrillation in Congenital Heart Disease: Mechanisms,Substrate ldentification and lnterventional Approaches