非酒精性脂肪性肝病患者早期肾损伤的潜在因素分析
2018-06-27
三峡大学人民医院消化内科,湖北 宜昌 443000
【Abstract】ObjectiveTo investigate the potential factors of early renal injury in adult non-alcoholic fatty liver disease (NAFLD) patients and improve the diagnosis rate of early renal injury.MethodsA total of 125 patients with NAFLD were collected in outpatient and inpatient, 78 cases of simple obesity (SO) group, routine liver biochemicaly, renal biochemical and early renal injury indicators were tested. The glomerular filtration rate (eGFR) and insulin resistance index (HOMA-IR) were calculated.ResultsNAFLD group was compared with SO group, the ALT, AST, FINS, Scr, urine trace albumin/creatinine (ACR), β2-microglobulin (β2-MG), eGFR and insulin resistance index (HOMA-IR) were statistically difference.Spearmancorrelation analysis showed that ACR was positively correlated with body mass index (BMI), waist circumference, fasting glucose (FBG), FINS, cholesterol (TC), triglyceride (TG), low density lipoprotein (LDL), HOMA-IR. HOMA-IR had the greatest influence of ACR.ConclusionACR and HOMA-IR are more sensitive than Scr, eGFR and β2-MG to detect early renal injury, and the combined analysis can improve the diagnostic rate of early renal injury.
【Keywords】 Non-alcoholic fatty liver disease; Simple obesity; Urine trace albumin/creatinine; Insulin resistance index
随着人们生活方式改变,非酒精性脂肪性肝病(non-alcoholic fatty liver disease,NAFLD)的患病率在逐渐升高。近年来,国外研究发现,NAFLD可增加患慢性肾病(chronic kidney disease,CKD)的发病风险[1-2]。CKD是一个全球健康问题,具有高发病率和高死亡率特点,该病的潜在危险因素包括高龄、肥胖、高血压、糖尿病,及时发现并治疗早期肾损伤至关重要,CKD被预防或被延迟将成为可能[3-4]。本研究主要分析NAFLD患者早期肾脏损伤状况及其影响因素,提高肾损伤的诊断率,为临床上更好地管理NAFLD患者,早期防治CKD的发生、发展提供理论依据。
1 资料与方法
1.1一般资料选取2016年1月至2017年6月三峡大学人民医院门诊就诊及住院的NAFLD患者125例,男103例,女22例,平均年龄55.4岁。选择同期体检的单纯性肥胖者(simple obesity,SO)78例为对照组(SO组),男62例,女16例,平均年龄48.6岁。两组在年龄、性别方面相比,差异无统计学意义(P>0.05),具有可比性。本次研究相关检查均得到研究对象的知情同意,并签署同意书;且经医院伦理委员会批准。
1.2纳入及排除标准NAFLD入选对象均符合2010年中华医学会肝脏病学分会脂肪肝和酒精性肝病学组修订的《非酒精性脂肪性肝病诊断标准》,排除标准:过量饮酒史,饮酒折合乙醇量男性>20 g/d,女性>10 g/d,无高血压病、糖尿病,慢性肾炎或慢性肾病史,恶性肿瘤史,血清HBsAg和/或抗-HCV阳性。影像学诊断具备以下3项腹部超声表现中的两项者为弥漫性脂肪肝:(1)肝脏近场回声弥漫性增强(“明亮肝”),回声强于肾脏;(2)肝内管道结构显示不清;(3)肝脏远场回声逐渐衰减。所有患者均为初次来我院就诊,未接受过任何治疗措施。
1.3 研究方法
1.3.1 标本采集:所有入选者清晨空腹抽取外周静脉血5 ml,分离血清待检。
1.3.2 观察指标:均记录人体学资料:性别、年龄、身高等。收集血清和晨尿检测:(1)肝脏生化指标:天冬氨酸氨基转移酶(AST)、丙氨酸氨基转移酶(ALT);(2)代谢指标:胆固醇(TC)、甘油三酯(TG)、高密度脂蛋白(HDL)、低密度脂蛋白(LDL)、空腹血糖(FBG);(3)肾脏生化及早期肾损指标:尿酸(UA)、血清肌酐(Scr)、尿微量白蛋白/肌酐(ACR)、β2-微球蛋白(β2-MG)、空腹胰岛素(FINS)。
1.3.3 工作定义:计算体质量指数(body mass index,BMI);采用肾脏病饮食改良(modification of diet in renal disease,MDRD)公式:男性GFR(ml/min per 1.73 m2)=186×(Scr)-1.154×(年龄)-0.203;女性GFR(ml/min per 1.73 m2)=186×(Scr)-1.154×(年龄)-0.203×0.742。其中GFR为肾小球滤过率,Scr为血清肌酐(mg/dl),年龄以岁为单位。肾损伤被定义为eGFR<90 ml/min per 1.73 m2。超重或肥胖诊断依据2005年国际糖尿病联盟标准[6],即:腰围>90 cm(男性)、>80 cm(女性),和(或)BMI>25 kg/m2。采用稳态模型评估计算法计算胰岛素抵抗指数(insulin resistance index,HOMA-IR),HOMA-IR=FBG(mmol/L)×FINS(μU/ml)/22.5。

2 结果
2.1NAFLD组和SO组患者的人体学资料比较两组患者性别、年龄、BMI、腰围相比,差异无统计学意义(P>0.05)(见表1)。
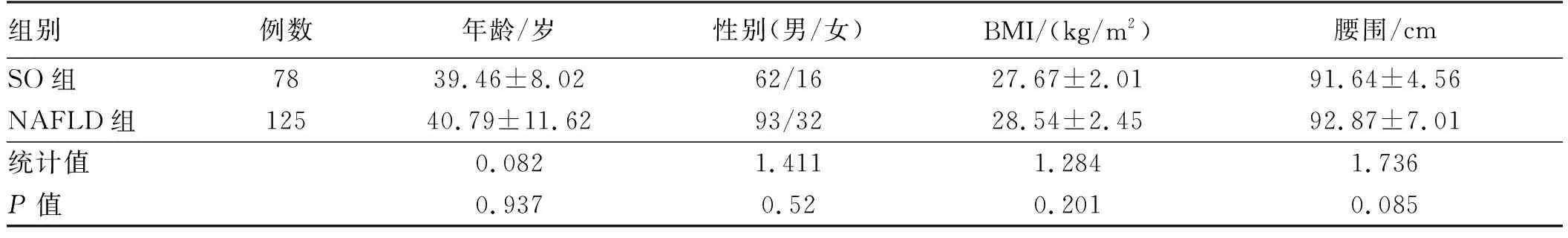
表1 NAFLD组和SO组人体学资料比较Tab 1 Comparison of human data between NAFLD group and SO group
2.2NAFLD组和SO组肝脏生化、代谢指标、肾脏指标比较两组的肾脏生化和早期肾脏损伤指标比较,总体NAFLD组的ALT、AST、FINS、HOMA-IR均升高(P<0.01),余指标差异无统计学意义(P>0.05)。总体NAFLD组的Scr、ACR、β2-MG均升高,eGFR则降低(P<0.05)。余指标差异无统计学意义(P>0.05)(见表2~3)。

表2 NAFLD组和SO组肝脏生化、代谢指标比较Tab 2 Comparison of liver biochemical and metabolic indexes between NAFLD group and SO group

表3 NAFLD组和SO组代谢指标、肾脏指标比较Tab 3 Comparison of metabolic indexes and renal indexes between NAFLD group and SO group
2.3NAFLD组中ACR与各指标相关分析ACR与BMI、腰围、FBG、FINS、TC、TG、LDL、HOMA-IR呈正相关(P<0.05),与HDL呈负相关(P<0.01),HOMA-IR对ACR的影响最大(见表4)。

表4 ACR同NAFLD各项指标的Spearman相关分析Tab 4 Spearman correlation analysis of ACR and NAFLD indicators
3 讨论
NAFLD与CKD经常合并存在,NAFLD与CKD的相互关系引人注目。2006年TARGHER等[7]最先指出在2型糖尿并NAFLD患者可增加CKD的发病率。2014年TARGHER等[8]又提出在1型糖尿病患者中NAFLD是CKD发生、发展的独立危险因素。前瞻性研究显示,NAFLD是CKD高发的危险因素,TARGHER等[9]对1 760例糖尿病患者随访6.5年,经过对大量的混杂因素进行校正分析后发现,脂肪肝与CKD发病率增加显著相关。
目前针对NAFLD与CKD的研究主要基于1型和2型糖尿病患者。本研究主要针对性别、年龄基线相同,同时排除糖尿病、高血压病及肾病史等,健康体检成人脂肪肝发生CKD的危险因素。本研究结果显示,NAFLD组和SO组在BMI、腰围、TC、TG、HDL、LDL、FBG差异均无统计学意义,但NAFLD组的ACR、β2-MG仍高于SO组,eGFR低于SO组,差异有统计学意义,提示NAFLD与早期肾脏损伤或CKD密切相关,NAFLD可能是早期肾脏损伤或CKD的危险因素。
eGFR、β2-MG是临床上常用的反映肾功能的良好指标,但当尿微量白蛋白出现异常时,患者eGFR还处于正常范围,且eGFR的计算复杂,不同情况下使用不同标准。研究[10-13]认为,CKD患者晨尿ACR和24 h尿微量白蛋白定量具有相关性,ACR替代24 h尿微量白蛋白定量来评估肾病患者尿微量白蛋白的排泄情况,预测早期肾脏损伤。本研究ACR与NAFLD相关指标的Spearman相关分析得出,ACR与BMI、腰围、FBG、FINS、TG、TC、LDL、HOMA-IR呈正相关,其中HOMA-IR对ACR的影响最大,提示伴有IR的NAFLD患者更易发生早期肾脏损伤或CKD。NAFLD慢性炎性反应可导致IR加重,考虑释放促炎性因子的释放,并发高胰岛素血症,脂联素的减少可进一步介导炎性反应及动脉粥样硬化[14-15]。同时胰岛素受体分布于所有肾单位细胞上,故IR可直接作用于肾组织,如内皮细胞、足细胞、系膜细胞等,导致蛋白尿、肾间质小管损伤及水钠代谢紊乱,最终诱导CKD的发生和发展[16-18]。由此可看出,ACR和HOMA-IR是较Scr、eGFR、β2-MG更敏感检测早期肾脏损伤的指标,对两者进行联合分析可提高早期肾损伤的诊断率。
对NAFLD进行早期干预,早期发现肾损伤的潜在危险因素至关重要,可降低CKD患病率,减轻社会产生的经济负担。 总之,CKD可能是NAFLD最重要的转归,未来可能需要更多的研究来阐述NAFLD与CKD的关系。
[1] AHN A L, CHOI J K, KIM M N, et al. Non-alcoholic fatty liver disease and chronic kidney disease in Koreans aged 50 years or older [J]. Korean J Fam Med, 2013, 34(3): 199-205. DOI: 10.4082/kjfm.2013.34.3.199.
[2] IX J H, SHARMA K. Mechanisms linking obsity, chronic kidney disease, and fatty live disease: the roles of fetuin-A, adiponectin, and AMPK [J]. J Am Soc Nephrol, 2010, 21(3): 406-412. DOI: 10.1681/ASN.2009080820.
[3] 舒泳翔, 吴鹏波, 郭芳. 非酒精性脂肪性肝病发病机制的研究进展[J]. 胃肠病学和肝病学杂志, 2015, 24(8): 901-903. DOI: 10.3969/j.issn.1006-5709.2015.08.001.
SHU Y X, WU P B, GUO F. Research progress of the pathogenesis of non-alcoholic fatty liver disease [J]. Chin J Gastroenterol Hepatol, 2015, 24(8): 901-903. DOI: 10.3969/j.issn.1006-5709.2015.08.001.
[4] 谢利芳, 王全楚. 非酒精性脂肪性肝病与代谢综合征关系的研究进展[J]. 胃肠病学和肝病学杂志, 2017, 26(10): 1110-1112. DOI: 10.3969 /j.issn.1006-5709.2017.10.010.
XIE L F, WANG Q C. The relationship between non-alcoholic fatty liver disease and metabolic syndrome [J]. Chin J Gastroenterol Hepatol, 2017, 26(10): 1110-1112. DOI: 10.3969 /j.issn.1006-5709.2017.10.010.
[5] 姚学敏, 叶必星, 林琳. 解读非酒精性脂肪性肝病诊治指南[J]. 胃肠病学和肝病学杂志, 2010, 19(6): 488-491. DOI: 10.3969/j.issn.1006-5709.2010.06.002.
YAO X M, YE B X, LIN L. Understanding and explanation on guidelines of the diagnosis and treatment in the non-alcoholic fatty liver disease [J]. Chin J Gastroenterol Hepatol, 2010, 19(6): 488-491. DOI: 10.3969/j.issn.1006-5709.2010.06.002.
[6] 杨文英. 国际糖尿病联盟2005糖尿病治疗指南要点解读[J]. 实用医院临床杂志, 2007, 4(5): 2-4. DOI: 10.3969/j.issn.1672-6170.2007.05.002.
YANG W Y. Highlights of the 2005 diabetes therapy guide of international diabetes federation [J]. Practical Journal of Clinical Medicine, 2007, 4(5): 2-4. DOI: 10.3969/j.issn.1672-6170.2007.05.002.
[7] TARGHER G, BERTOLINI L, PADOVANI R, et al. Non-alcoholic fatty liver disease is associated with carotid artery wall thickness in diet-controlled type 2 diabetic patients [J]. J Endocrinol Invest, 2006, 29(1): 55-60. DOI: 10.1007/bf03349177.
[8] TARGHER G, MANTOVANI A, PICHIRI I, et al. Nonalcoholic fatty liver disease is independently associated with an increased incidence of chronic kidney disease in patients with type 1 diabetes [J]. Diabetes Care, 2014, 37(6): 1729-1736. DOI: 10.2337/dc13-2704.
[9] TARGHER G, BERTOLINI L, RODELLA S, et al. Non-alcoholic fatty liver disease is independently associated with an increased prevalence of chronic kidney disease and proferative/laser-treated retinopathy in type 2 diabetic patients [J]. Diabetologia, 2008, 51(3): 444-450. DOI: 10.1007/s00125-007-0897-4.
[10] THOMAS G, SEHGAL A R, KASHYAP S R, et al. Metabolic syndrome and kidney disease: a systematic review and meta-analysis [J]. Clin J Am Soc Nephrol, 2011, 6(10): 2364-2373. DOI: 10.2215/cjn.02180311.
[11] SCHUPPAN D, SCHATTENBERG J M. Non-alcoholic steatohepatitis: pathogenesis and novel therapeutic approaches [J]. J Gastroenterol Hepatol, 2013, 28 Suppl 1: 68-76. DOI: 10.1111/jgh.12212.
[12] TARGHER G, BERTOLINI L, RODELLA S, et al. Relationship between kidney function and liver histology in subjects with nonalcoholic steatohepatitis [J]. Clin J Am Soc Nephrol, 2010, 5(12): 2166-2171. DOI: 10.2215/CJN.05050610.
[13] YILMAZ Y, ALAHDAB Y O, YONAL O, et al. Microalbuminuria in nondiabetic patients with nonalcoholic fatty liver disease: association with liver fibrosis [J]. Metabolism, 2010, 59(9): 1327-1330. DOI: 10.1016/j.metabol.2009.12.012.
[14] 宋新文, 申保生, 王宏伟. 非酒精性脂肪性肝病患者血清脂联素和瘦素水平变化[J]. 实用肝脏病杂志, 2013, 16(2): 141-143. DOI: 10.3969/j.issn.1672-5069.2013.02.016.
SONG X W, SHEN B S, WANG H W. Serum adiponectin and leptin levels in patients with non- alcoholic fatty liver disease [J]. J Clin Hepatol, 2013, 16(2): 141-143. DOI: 10.3969/j.issn.1672-5069.2013.02.016.
[15] KRONENBERG F. Emerging risk factors and markers of chronic kidney disease progression [J]. Nat Rev Nephrol, 2009, 5(12): 677-689. DOI: 10.1038/nrneph.2009.173.
[16] TARGHERR G, PICHIRI I, ZOPINI G, et al. Increased prevalence of chronic kidney disease in patients with type 1 diabetes and non-alcoholic fatty liver [J]. Diabet Med, 2012, 29(2): 220-226. DOI: 10.1111/j.1464-5491.2011.03427.x.
[17] BYRNE C D. Dorothy Hodgkin Lecture 2012: non-alcoholic fatty liver disease, insulin resistance and ectopic fat: a new problem in diabetes management [J]. Diabet Med, 2012, 29(9): 1098-1107. DOI: 10.1111/j.1464-5491.2012.03732.x.
[18] SABIO G, DAVIS R J. cJun NH2-terminal kinase 1 (JNK1): roles in metabolic regulation of insulin resistance [J]. Trends Biochem Sci, 2010, 35(9): 490-496. DOI: 10.1016/j.tibs.2010.04.004.
