Effect of acupuncture plus Tai Ji Quan on the recovery of neurological function and depression state in post-stroke depression patients
2018-04-28ZhangLin张林ZhaoJing赵静QuanShulin全淑林LiuYehui刘叶辉ShiXuehui石学慧LiZhenguang李振光WangJingjing王净净ZhongYan钟艳
Zhang Lin (张林), Zhao Jing (赵静), Quan Shu-lin (全淑林), Liu Ye-hui (刘叶辉), Shi Xue-hui (石学慧), Li Zhen-guang(李振光), Wang Jing-jing (王净净), Zhong Yan (钟艳)
1 Hunan University of Chinese Medicine, Changsha 410007, China
2 School of Medicine, Southeast University, Nanjing 210009, China
3 Second Affiliated Hospital of Hunan University of Chinese Medicine, Changsha 410005, China
4 Brain Hospital of Hunan Province, Changsha 410007, China
Post-stroke depression (PSD) is a common complication after stroke, with an incidence up to 30%-50%[1], mainly manifested by persistent low mood,loss of interest, and even abnormal behavior or suicide attempt[2]. PSD not only directly influences the rehabilitation, but also brings heavy burden to family and society. Intervention in early stage is significant in preventing and treating PSD. Our research group adopted acupuncture plus Tai Ji Quan in treating PSD,and the report is given as follows.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria of Western medicine
The diagnostic criteria of stroke referred toChinese Prevention and Treatment Guidance for Cerebrovascular Diseases[3]; the diagnostic criteria of depression referred to theChinese Classification and Diagnosis of Mental Diseases-3 (CCMD-3)[4].
1.1.2 Pattern differentiation criteria of traditional Chinese medicine (TCM)
The TCM pattern differentiation criteria were based on the differentiation criteria of depression syndrome in theCriteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine[5].
1.2 Inclusion criteria
Conforming to the above diagnostic criteria of both Western and Chinese medicine; head CT or MRI records available; the score of Hamilton depression rating scale(HAMD) ≥17; muscle strength of the affected limb ≥grade Ⅲ, and the grading of modified Ashworth scale ≤grade Ⅰ; age ≤75 years old; not on any psychotropic substances during the recent 2 weeks prior to the recruitment; approved of the treatment protocol and signed the informed consent form.
1.3 Exclusion criteria
Accompanied by systemic and primary diseases such as tumor, hematological and endocrine systems, or severe organic disorders involving heart, liver and kidney; those unable to cooperate due to severe mental retardation, speech dysfunction or mental disorders;with a history of psychosis.
1.4 Rejection criteria
Those with poor compliance, unable to strictly follow the treatment protocol; those lost to follow-up, quitted,or with incomplete information; those who used other medications during the research that may affect the study results.
1.5 Statistical method
The SPSS 21.0 version software was used for statistical analysis. The measurement data were expressed by mean ± standard deviation, and analyzed byt-test if the data conformed to normal distribution and homogeneity of variance;nonparametric test was used when the data were of abnormal distribution and heterogeneity of variance.The enumeration data were analyzed by Chi-square test;the ranked data by rank-sum test.P<0.05 was considered to indicate a statistical significance.
1.6 General data
The patients were all diagnosed with post-stroke depression and recruited from the Stroke Department,the Second Affiliated Hospital of Hunan University of Chinese Medicine between September of 2014 and June of 2016. Initially, there were 200 subjects enrolled,but only 105 conformed to the inclusion criteria and were then randomized into a group of acupuncture plus Tai Ji (53 cases) and a control group (52 cases) based on the visiting sequence. However, at the end of the intervention, only 90 subjects completed the study and were recruited for statistical analysis, 45 cases in each group. The flow chart of the whole study is shown in Figure 1.
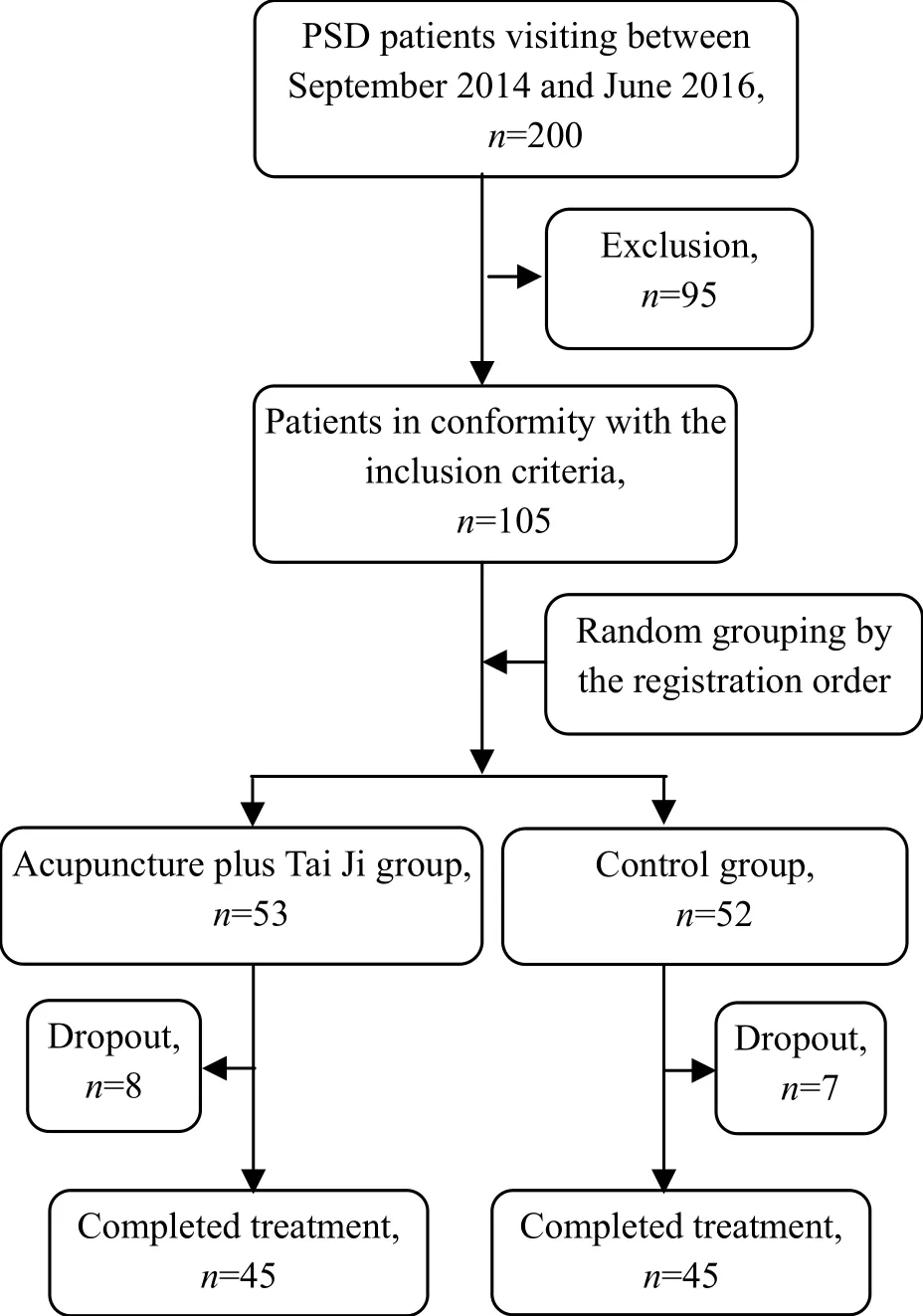
Figure 1. Study flow chart
There were no significant differences in the data of age, gender, disease duration and stroke type between the two groups (P>0.05), indicating the comparability(Table 1).
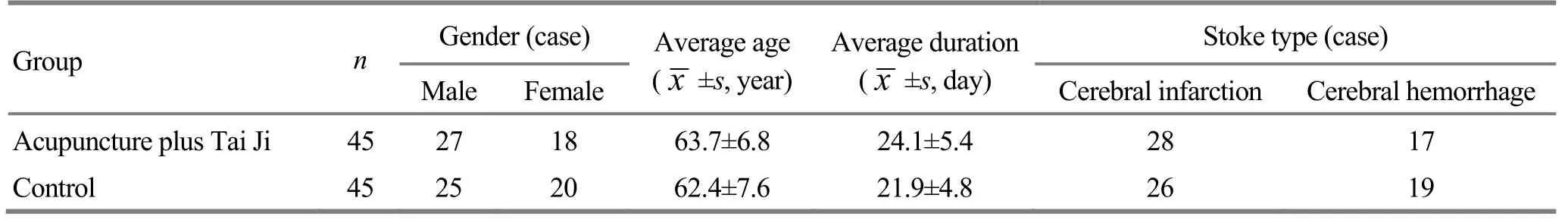
Table 1. Comparison of the general data
2 Treatment Methods
All the subjects were given routine and basic treatment for stroke by following theChinese Prevention and Treatment Guidance for Cerebrovascular Diseases[3], together with rehabilitation if necessary and possible.
2.1 Acupuncture plus Tai Ji group
2.1.1 Acupuncture treatment
The acupuncture treatment was conducted on the purpose of awakening the brain and opening the orifices.
Points or areas on the head: Middle Line of Forehead(MS 1), Anterior Oblique Line of Vertex- temporal (MS 6),Baihui (GV 20), Sishencong (EX-HN 1), Shenting (GV 24)and Yintang (GV 29).
Body points: Bilateral Shenmen (HT 7), Neiguan(PC 6), Taichong (LR 3) and Hegu (LI 4); Chize (LU 5),Quchi (LI 11), Shousanli (LI 10), Fengshi (GB 31), Xuehai(SP 10), Yanglingquan (GB 34) and Qiuxu (GB 40), all on the affected side.
Adjunct points based on pattern differentiation:Fenglong (ST 40) was added for pattern of wind-phlegm obstructing collaterals; Zusanli (ST 36) for pattern of qi deficiency and blood stagnation.
Method: The points were located according to theNomenclature and Location of Acupuncture Points(GB/T12345-2006)[6]. Patient took a supine position.After proper sterilization for the to-be-treated areas,disposable filiform needles of 0.35 mm in diameter and 25 mm or 40 mm in length were used for acupuncture.For points on the head, needles were inserted horizontally by 5-15 mm; for body points, needles were punctured perpendicularly by 10-15 mm, according to the thickness of muscles in the area. When needling qi was obtained, even reinforcing-reducing manipulation(twirling manipulation for points on the head;lifting-thrusting and twirling manipulations for points on limbs) were performed for 1-3 min. The needles were then retained for 30 min. Five successive sessions of acupuncture treatment were given every week followed by a 2-day interval. One-month treatment was taken as a course, and the patients were given 1 course of treatment in total.
2.1.2 Tai Ji Quan practice
The patients were taught and guided to practice Yang’s 24-form simplified Tai Ji Quan (Figure 2-Figure 25)by professional teachers during hospitalization. They were also supervised and guided via telephone after discharged from hospital. The Tai Ji Quan practice was performed 5 times a week, 40 min each time, for 12 months in total.
Figure 2. Beginning form

Figure 3. Part wild horse’s mane

Figure 4. A white crane spreads its wings

Figure 5. Brush knee and step forward

Figure 6. Play the lute

Figure 7. Reverse reeling forearm

Figure 8. Left grasp sparrow’s tail

Figure 9. Right grasp sparrow’s tail

Figure 10. Single whip

Figure 11. Wave hands like clouds

Figure 12. Single whip

Figure 13. High pat on horse

Figure 14. Right heel kick
Figure 15. Strike to ears with both fists

Figure 16. Turn body and left heel kick

Figure 17. Left lower body and stand on one leg

Figure 18. Right lower body and stand on one leg

Figure 19. Shuttle back and forth

Figure 20. Needle at sea bottom

Figure 21. Fan through the back

Figure 22. Turn body, deflect,parry and punch
Figure 23. Appears closed

Figure 24. Cross hands

Figure 25. Closing form
2.2 Control group
Patients in the control group were asked to orally take citalopram hydrobromide tablets (lot No.H20120457, Xi’an Janssen Pharmaceutical Co. Ltd.,China), at 20 mg/d but tailored by 10 mg each week according to the patient’s condition (no more than 40 mg/d). One-month treatment was taken as a course,and a total of 3 courses were observed. If the treatment was satisfactory, the dosage of the medication would be reduced by 10 mg per week till termination. A 1-year follow-up study was conducted.
3 Therapeutic Observation
3.1 Observation items
Each observation item was scored prior to the treatment, after 1-month treatment, and 12 months later, respectively.
3.1.1 National Institutes of Health stroke scale(NIHSS)[7]
NIHSS is composed of 11 items including level of consciousness, horizontal eye movement, visual field test, facial palsy, motor arm, motor leg, limb ataxia, and sensory, etc. Each item scores a specific ability. The total score ranges from 0 to 42. A higher score is indicative of a severer neurologic deficit. A score from 0-1: no stroke symptoms; 1-4: minor stroke; 5-15: moderate stroke;16-20: moderate to severe stroke; 21-42: severe stroke.
3.1.2 Barthel index (BI)[7]
BI consists of 10 variables, which are feeding, bathing,grooming, dressing, presence or absence of fecal incontinence, presence or absence of urinary incontinence, walking, and climbing stairs, etc. Each item is scored according to the level of accomplishment in order to evaluate the activities of daily living (ADL).The maximum total BI score is 100, and a higher score indicates a higher level of independence. Total BI score >60 points: mild dysfunction; 60-41 points:moderate dysfunction; ≤40 points: severe dysfunction.
3.1.3 HAMD[4]
HAMD contains 24 items, such as depressed mood,feelings of guilt, difficulty in falling asleep,anxiety-psychic, insight and feelings of despair, to estimate the severity of depression. A higher total HAMD score is indicative of severer depression. Total HAMD score <8 points: no depression; ≥8 points but<20 points: possible existence of depression; ≥20 points but <35 points: mild or moderate depression; ≥35 points: severe depression.
3.2 Criteria of therapeutic efficacy
The evaluation of clinical efficacy in improving neurological function referred to the criteria of therapeutic efficacy for stroke recommended by the World Health Organization (WHO)[7], i.e. by taking the reduction rate of NIHSS score as the evaluation index.Reduction rate of NIHSS score = (Pre-treatment total NIHSS score – Post-treatment total NIHSS score) ÷ Pretreatment total NIHSS score × 100%.
Basically recovered: Reduction rate of NIHSS score≥91%.
Markedly effective: Reduction rate of NIHSS score≥46% but <91%.
Effective: Reduction rate of NIHSS score ≥18% but<46%.
Failure: Reduction rate of NIHSS score <18%, or NIHSS score increased rather than dropped.
The evaluation of efficacy in treating depression was based on the reduction rate of HAMD score[4].Reduction rate of HAMD score = (Pre-treatment total HAMD score – Post-treatment total HAMD score) ÷ Pretreatment total HAMD score × 100%.
Recovered: Reduction rate of HAMD score ≥75%.
Markedly effective: Reduction rate of HAMD score≥50% but <75%.
Effective: Reduction rate of HAMD score ≥25% but<50%.
Failure: Reduction rate of HAMD score <25%.
3.3 Results
3.3.1 Comparison of NIHSS score
NIHSS score decreased after 1-month treatment as well as in the 12-month follow-up in both groups compared to the score before the intervention, with statistical significances (allP<0.01). Before the treatment, there was no significant difference in NIHSS score between the two groups (P>0.05); after 1-month treatment, the between-group difference in the score was statistically significant (P<0.05); the 1-year followup showed that there was a significant difference in NIHSS score between the two groups (P<0.01),(Table 2).
3.3.2 Comparison of the clinical efficacy in treating stroke
The 12-month follow-up study showed that the total effective rate in treating stroke was 84.4% in the acupuncture plus Tai Ji group, versus 68.9% in the control group, and the between-group difference was statistically significant (Z=–2.418,P=0.016), suggesting that the acupuncture plus Tai Ji group should be superior to the control group in comparing the therapeutic efficacy (Table 3).3.3.3 Comparison of BI score
BI score was found increased in both groups after 1-month treatment and in the 12-month follow-up study compared with the score before the treatment,with statistical significances (allP<0.01). Before the treatment, there was no significant difference in BI score between the two groups (P>0.05); the betweengroup difference in BI score was statistically significant after 1-month treatment and in the follow-up study(bothP<0.01), (Table 4).
Table 2. Comparison of NIHSS score
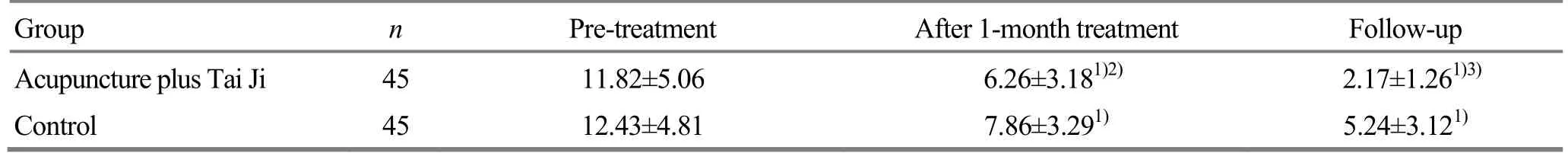
Table 2. Comparison of NIHSS score
Note: Ⅰntra-group comparison, 1) P<0.01; compared with the control group at the same time point, 2) P<0.05, 3) P<0.01
Group n Pre-treatment After 1-month treatment Follow-up Acupuncture plus Tai Ji 45 11.82±5.06 6.26±3.181)2) 2.17±1.261)3)Control 45 12.43±4.81 7.86±3.291) 5.24±3.121)

Table 3. Comparison of the clinical efficacy in treating stroke (case)
Table 4. Comparison of BI score
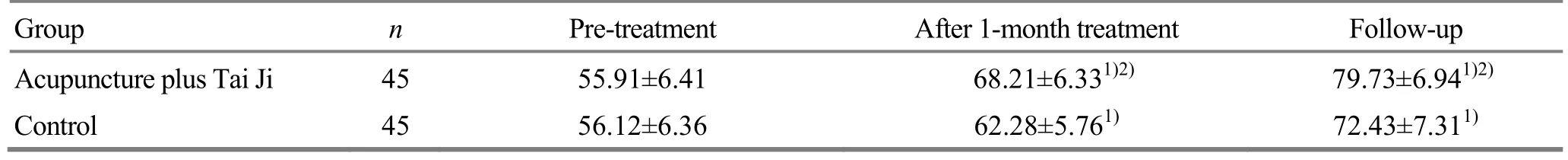
Table 4. Comparison of BI score
Note: Ⅰntra-group comparison, 1) P<0.01; compared with the control group at the same time point, 2) P<0.01
Group n Pre-treatment After 1-month treatment Follow-up Acupuncture plus Tai Ji 45 55.91±6.41 68.21±6.331)2) 79.73±6.941)2)Control 45 56.12±6.36 62.28±5.761) 72.43±7.311)
3.3.4 Comparison of HAMD score
HAMD score was found decreased after 1-month treatment as well as in the 12-month follow-up in both groups compared to the score before the intervention,with statistical significances (allP<0.01). Before the treatment, there was no significant difference in HAMD score between the two groups (P>0.05); the betweengroup difference in HAMD score was statistically significant after 1-month treatment and in the follow-up study (bothP<0.01), (Table 5).
3.3.5 Comparison of therapeutic efficacy in treating depression
The 12-month follow-up showed that the toal effective rate in treating depression was 86.7% in the acupuncture plus Tai Ji group, versus 77.8% in the control group, and the between-group difference was statistically significant (Z=–2.056,P=0.040), indicating that the acupuncture plus Tai Ji group should be superior to the control group in treating depression(Table 6).
Table 5. Comparison of HAMD score

Table 5. Comparison of HAMD score
Note: Ⅰntra-group comparison, 1) P<0.01; compared with the control group at the same time point, 2) P<0.01
Group n Pre-treatment After 1-month treatment Follow-up Acupuncture plus Tai Ji 45 25.60±4.44 12.33±4.721)2) 6.31±3.211)2)Control 45 24.44±4.58 15.68±4.591) 8.26±3.321)

Table 6. Comparison of the therapeutic efficacy in treating depression
4 Discussion
Patients after stroke may experience emotional dysfunctions, such as PSD and anxiety. The pathogenesis of PSD is not completely clear yet, though it possibly involves brain injuries, neurologic deficit[8-10],stress response, and irregular secretion of neurotransmitters including norepinephrine (NE),5-hydroxytryptamine (5-HT) and dopamine (DA)[11].
Treatment for PSD mainly includes medication,psychotherapy, and behavioral therapy. Medication is the most popular treatment, and selective serotonin reuptake inhibitors (SSRIs) are often used, though it may cause side effects or adverse events, such as mouth dryness, poor appetite, dizziness, and insomnia[12]. PSD belongs to the scope of depression syndrome in TCM,and phlegm and stasis obstructing meridians and collaterals, and yin-yang and qi-blood imbalance are considered to be the basic pathogenesis. PSD affects the brain, with wind-phlegm obstructing collaterals and disharmonious qi-blood as the root cause and liver-qi stagnation as the superficial cause. Therefore, the treatment should focus on soothing liver and relieving depression, calming mind and opening orifices,regulating qi and activating blood circulation to unblock collaterals. Acupuncture has been extensively used in rehabilitation for stroke[13-16]. It’s known that acupuncture-moxibustion is effective for PSD, with minor adverse reactions. It can boost the recovery of neurological function and improve depression symptoms, which has been well verified at home and abroad[13-16]. Waiguan (TE 5), Hegu (LI 4), Baihui (GV 20),Quchi (LI 11) plus Chize (LU 5) can produce a significant efficacy in improving the limb function in stroke[17-18].Modern mechanism research has found that acupuncture can protect brain neurons, inhibit cell apoptosis[19], promote the establishment of compensatory circulation[20], increase blood supply to brain, and modulate blood lipids[21]. Meanwhile, as a safe effective treatment for PSD[22-23], acupuncture may play its role via regulating neurotransmitters such as NE,5-HT and DA[24-25].
In this study, points on the head were selected according to the function zones of brain and the routes of meridians: Middle Line of Forehead (MS 1) governs emotions; Anterior Oblique Line of Vertex-temporal(MS 6) is in charge of motor function; Baihui (GV 20), a point of Governor Vessel, acts to open orifices and awaken brain; Sishencong (EX-HN 1), Shenting (GV 24)and Yintang (GV 29) can calm the mind and open orifices, regulate and unblock meridians and collaterals.Of the selected body points, Neiguan (PC 6), the Luo-Connecting point of the Pericardium Meridian, and Shenmen (HT 7), the Yuan-Primary point of the Heart Meridian, can soothe the heart and calm the mind;Taichong (LR 3) can soothe the liver, resolve depression and regulate qi. Among all the body points, the points of Yangming meridians were mostly selected since these meridians are rich in qi and blood. Points around the affected joints were also used, including Chize (LU 5),Quchi (LI 11) and Shousanli (LI 10) on the upper limb,and Fengshi (GB 31), Xuehai (SP 10), Yanglingquan(GB 34) and Qiuxu (GB 40) on the lower limb, to regulate qi, activate blood flow and unblock collaterals.These points were used together to soothe the liver and resolve depression, calm the mind and open orifices,regulate qi and activate blood flow to unblock collaterals.
Tai Ji Quan originates in China and has a long history.It’s composed of three factors, physical practice, mind practice and qi practice, which integrate both mental regulation and physiological regulation, and conform to the holism theory in TCM. During the practice of Tai Ji Quan, practitioners always have a high subjectivity, and such an active exercise can boost the activity of the motor center in cerebral cortex, increase the nerve excitability and promote the recovery of limb function[26]. Hart J,et al[26]found that Chen’s Tai Ji can help recover the balance function. McGibbon CA,et al[27]discovered that Yang’s Tai Ji can regulate the pattern of nerve and muscle movement, promote the restoration of patient’s function, and improve depression and anxiety. Wang W,et al[28]found that Yang’s Tai Ji can help the recovery of cognition after stroke, and improve sleep quality and depressive symptoms. Li Y,et al[29]and Rosenbaum S,et al[30]revealed that Tai Ji Quan in community sports can regulate neurotransmitters such as NE, 5-HT and DA,and a long-term practice can achieve an even better result. Therefore, the current study aimed to observe the short-term (1 month) and long-term (12 months)effects of acupuncture plus Tai Ji Quan in recovering neurological function and mental health in PSD, for achieving an aggregate treatment, merging the rehabilitation of hospital, community and family, and displaying the advantage of TCM.
Subjects recruited in this trial were majorly in sub-acute and remission stages with moderate-severe depression. During the study, we found that the rhythm,consistency and even speed of Tai Ji Quan enabled the patients to better control the muscles of upper and lower limbs. In clinic, patients with high muscle tension,spasm and low muscle strength can start from easy forms and practice gradually, to promote the disengaging movement and reduce spasm. The results after 1-month treatment and the 12-month follow-up all showed that acupuncture plus Tai Ji Quan is effective in restoring the limb function and improving depression in PSD patients, and thus it’s worthy of further promotion.
Conflict of Interest
The authors declared that there was no potential conflict of interest in this article.
This work was supported by Wang Jing-jing’s Ⅰnheritance Studio of National Famous Traditional Chinese Medicine Experts (王净净全国名老中医药专家传承工作室);Graduate Student Research Ⅰnnovation Project of Hunan Province (湖南省研究生科研创新项目, No.CX2016B354); Open Fund for National Key Discipline of Diagnostics of Traditional Chinese Medicine (中医诊断学国家重点学科开放基金资助项目, No. 2015ZYZD27).
Statement of Informed Consent
Ⅰnformed consent was obtained from all individual participants or their relatives included in this study.
[1] Hackett ML, Yapa C, Parag V, Anderson CS. Frequency of depression after stroke: a systematic review of observational studies. Stroke, 2005, 36(6): 1330-1340.
[2] Neurological Rehabilitation Group, Neurology Association of Chinese Medical Association; Cerebrovascular Diseases Group, Neurology Association of Chinese Medical Association; Committee Office of Screening, Preventing and Treating Stroke, Ministry of Health; Zhang T. Chinese prevention and treatment guidance for cerebrovascular diseases (2011 complete version). Zhongguo Kangfu Lilun Yu Shijian, 2012, 18(4): 301-318.
[3] Rao ML, Editorial Committee of Chinese Prevention and Treatment Guidance for Cerebrovascular Diseases.Chinese Prevention and Treatment Guidance for Cerebrovascular Diseases (Pilot Edition). Beijing: People’s Medical Publishing House, 2007: 21-67.
[4] Chinese Society of Psychiatry. Chinese Classification and Diagnostic Criteria of Mental Disorders. 3rd Edition. Jinan:Shandong Science & Technology Press, 2001: 87-88.
[5] State Administration of Traditional Chinese Medicine.Criteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine. Nanjing:Nanjing University Press, 1994: 33-34.
[6] General Administration of Quality Supervision, Ⅰnspection and Quarantine of the People’s Republic of China,Standardization Administration of the People’s Republic of China. Nomenclature and Location of Acupuncture Points(GB/T 12346-2006). Beijing: Standards Press of China,2006.
[7] Goldstein LB, Bertels C, Davis JN. Ⅰnterrater reliability of the NⅠH stroke scale. Arch Neurol, 1989, 46(6): 660-662.
[8] Zhang CQ, Fang XH, Liu HJ, Wang WH, Zhang XQ, Li NY. The relationship between poststroke depression and stroke lesions. Zhongguo Shenjing Jingshen Jibing Zazhi,2009, 35(3): 148-151.
[9] Ford CE, Malley D, Bateman A, Clare ⅠC, Wagner AP,Gracey F. Selection and visualisation of outcome measures for complex post-acute acquired brain injury rehabilitation interventions. NeuroRehabilitation, 2016, 39(1): 65-79.
[10] Schöttke H, Giabbiconi CM. Post-stroke depression and post-stroke anxiety: prevalence and predictors. Ⅰnt Psychogeriatr, 2015, 27(11): 1805-1812.
[11] Chun HY, Whiteley WN, Carson A, Dennis M, Mead GE.Anxiety after stroke: time for an intervention. Ⅰnt J Stroke,2015, 10(5): 655-656.
[12] Fruehwald S, Gatterbauer E, Rehak P, Baumhackl U. Early fluoxetine treatment of post-stroke depression: a threemonth double-blind placebo-controlled study with an openlabel long-term follow up. J Neurol, 2003, 250(3): 347-351.
[13] Nie RR, Huang CH. Post-stroke depression treated with acupuncture and moxibustion: an evaluation of therapeutic effect and safety. Zhongguo Zhen Jiu, 2013, 33(6):490-494.
[14] Xiong J, Du YH, Liu JL, Lin XM, Sun P, Xiao L, Gao X,Chen YW. Comparison of the therapeutic efficacy between acupuncture-moxibustion and Western medication for post-stroke depression: a systematic review. Xunzheng Yixue, 2010, 10(3): 179-185, 192.
[15] Fan L, Fu WB, Chen Z, Xu NG, Liu JH, Lü AP, Su SY, Wu TX, Ou AH. Curative effect of acupuncture on quality of life in patient with depression: a clinical randomized single-blind placebo-controlled study. J Tradit Chin Med,2016, 36(2): 151-159.
[16] Ding N, Li R, Tian HH. Effect of acupuncture and moxibustion interventions on ethological changes and 5-HT/5-HⅠAA levels in prefrontal cortex in depression rats.Zhen Ci Yan Jiu, 2016, 41(1): 45-50.
[17] Li LX, Tian G, Meng ZH, Fan XN, Zhang CH, Shi XM.Different stimulation intensities of acupuncture at Hegu(LⅠ 4) for central facial nerve paralysis after ischemic stroke: a randomized controlled trial. Zhongguo Zhen Jiu,2014, 34(7): 669-674.
[18] Lin Q, Chen AL, Cheng K, Yu CJ, Zhou YG, Wang XJ,Yang T, Yuan B, Li XP. Effects of acupuncture on motor function, balance function and activities of daily living of patients with stroke. Zhongguo Kangfu Yixue Zazhi, 2015,30(9): 898-901, 906.
[19] Luo ZD, Luo ZK, Xu NG, Lai XS, Yin LH. Ⅰnfluence of electroacupuncture on apoptosis and nerve growth factor of focal cerebral ischemia of rats. Zhongguo Linchuang Kangfu, 2004, 8(7): 1382-1383.
[20] Luo KT, Zhu JH, Xu YM, Fan DH, Ni CC. Effects of acupuncture treatment on collateral circulation and Rehabilitation of limb function in patients with acute cerebral infarction caused by middle cerebral artery occlusion. Zhonghua Quanke Yixue, 2016, 14(5): 841-843.
[21] Xue JM, Liu LQ, Li YL, Li MY. Experiences of application of acupuncture in stroke rehabilitation with integrated traditional Chinese and Western medicine.Zhongguo Kangfu Lilun Yu Shijian, 2016, 22(2): 245-248.
[22] Cui QQ, Cai SC, Cao YY, Yuan WH. Research progress of acupuncture treatment for post-stroke depression. Zhenjiu Linchuang Zazhi, 2013, 29(6): 82-85.
[23] Tong X, Liu DD, Wei Y, Kou JY, Yang TS, Qiao LD.Ⅰntervening effect of mind-regulating and liver-soothing acupuncture therapy on post-stroke depression. Zhongguo Yiyao Kexue, 2012, 2(3): 127-128.
[24] Zhang XB, Wang Y, Wang Z, Liang FJ, Guo XL, Xiao W.Effect of acupuncture on protein expression of 5-HTT,5-HT1AR, NEα2R of post-stroke depression rats. Beijing Zhongyiyao Daxue Xuebao, 2016, 39(9): 783-788.
[25] Cai L, Liu Y. Experimental study on the effect of acupuncture on the behavior and monoamine neurotransmitter in post-stroke depression rats. Jiangsu Zhongyiyao, 2013, 45(10): 71-73.
[26] Hart J, Kanner H, Gilboa-Mayo R, Haroeh-Peer O,Rozenthul-Sorokin N, Eldar R. Tai Chi Chuan practice in community-dwelling persons after stroke. Ⅰnt J Rehabil Res,2004, 27(4): 303-304.
[27] McGibbon CA, Krebs DE, Parker SW, Scarborough DM,Wayne PM, Wolf SL. Tai Chi and vestibular rehabilitation improve vestibulopathic gait via different neuromuscular mechanisms: preliminary report. BMC Neurol, 2005, 5(1):3.
[28] Wang W, Sawada M, Noriyama Y, Arita K, Ota T,Sadamatsu M, Kiyotou R, Hirai M, Kishimoto T. Tai Chi exercise versus rehabilitation for the elderly with cerebral vascular disorder: a single-blinded randomized controlled trial. Psychogeriatrics, 2010, 10(3): 160-166.
[29] Li Y, Su Q, Guo H, Wu H, Du H, Yang G, Meng G, Li C,Nagatomi R, Niu K. Long-term Tai Chi training is related to depressive symptoms among Tai Chi practitioners. J Affect Disord, 2014, 169: 36-39.
[30] Rosenbaum S, Tiedemann A, Sherrington C, Curtis J, Ward PB. Physical activity interventions for people with mental illness: a systematic review and meta-analysis. J Clin Psychiatry, 2014, 75(9): 964-974.
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Analysis of point-selection pattern in acupuncture-moxibustion treatment of amblyopia
- Clinical observation on cervical chiropractic for cervical spondylosis of vertebral artery type
- Observation on clinical effect of tuina plus Western medication for functional dyspepsia due to liver qi stagnation and spleen deficiency
- Yi Jin Jing (Sinew-transforming Qigong Exercises) for primary osteoporosis in the elderly: a clinical trial
- Effect of An-pressing manipulation on the serum levels of T-AOC and CK-MM in volunteers with delayed onset muscle soreness in biceps brachii
- Effect of acupuncture in intervening heroin-induced brain damage via regulating ubiquitin-proteasome pathway