Distinguishing normal brain aging from the development of Alzheimer’s disease: inflammation, insulin signaling and cognition
2018-01-13PaulDenverPaulaMcClean
Paul Denver , Paula L. McClean
1 Greater Los Angeles Veterans Affairs Healthcare System, West Los Angeles Medical Center and Department of Neurology, University of
California, Los Angeles, CA, USA
2 Centre for Molecular Biosciences, University of Ulster, Coleraine, Northern Ireland, UK
3 Northern Ireland Centre for Stratified Medicine, Clinical, Translational and Research Innovation Centre (C-TRIC), University of Ulster, Derry/Londonderry, Northern Ireland, UK
Funding: This work was supported by the Department of Education and Learning, Northern Ireland, UK.
Abstract As populations age, prevalence of Alzheimer’s disease (AD) is rising. Over 100 years of research has provided valuable insights into the pathophysiology of the disease, for which age is the principal risk factor.However, in recent years, a multitude of clinical trial failures has led to pharmaceutical corporations becoming more and more unwilling to support drug development in AD. It is possible that dependence on the amyloid cascade hypothesis as a guide for preclinical research and drug discovery is part of the problem. Accumulating evidence suggests that amyloid plaques and tau tangles are evident in non-demented individuals and that reducing or clearing these lesions does not always result in clinical improvement. Normal aging is associated with pathologies and cognitive decline that are similar to those observed in AD, making differentiation of AD-related cognitive decline and neuropathology challenging. In this mini-review, we discuss the difficulties with discerning normal, age-related cognitive decline with that related to AD. We also discuss some neuropathological features of AD and aging, including amyloid and tau pathology, synapse loss, inflammation and insulin signaling in the brain, with a view to highlighting cognitive or neuropathological markers that distinguish AD from normal aging. It is hoped that this review will help to bolster future preclinical research and support the development of clinical tools and therapeutics for AD.
Key Words: Alzheimer’s disease; aging; inflammation; cognitive function; spatial learning; insulin signaling;synapses; cytokines
Introduction
Normal aging is associated with deterioration of cognitive function and accumulation of neuropathological lesions that can also occur in Alzheimer’s disease (AD). Distinguishing AD from normal aging, particularly in the earliest stages,allows for more thorough clinical characterization of abnormal cognitive decline and can also provide insights into AD pathophysiology that may ultimately support drug discovery,an element of the AD field that is currently lacking. Since its inception, the amyloid cascade hypothesis has bolstered AD research and helped progress the field immensely, however a fixation on this model may be hindering scientific advances and drug development. We will briefly describe some of the difficulties with defining abnormal cognitive deterioration,outline some issues associated with traditional AD neuropathology as correlates of cognitive dysfunction and discuss aspects of synapse loss, inflammation and insulin signaling in the brain as potentially distinct in AD versus normal aging.Consistent clinical trial failures for drugs aimed at treating AD based on the predictions of the amyloid cascade hypothesis have led several pharmaceutical companies to abandon their support for trials aimed at developing AD therapeutics, leading to a significant disparity between AD drug development and disease prevalence, which is predicted to continue rising as global populations age. This mini-review aims to summarize recent clinical and pre-clinical findings related to inflammation,insulin signaling and cognition in AD and aging. It is hoped that this will highlight gaps in knowledge and encourage progression of research aiming to distinguish the development of AD from normal aging.
Differentiating Abnormal from Normal Cognitive Decline
As the quality and availability of healthcare continues to improve around the world, average life expectancy is being extended (Timonin et al., 2016), such that prevalence of diseases associated with aging is growing (Murray et al., 2013). AD is a progressive neurodegenerative disease, for which advancing age is a major risk factor (Querfurth and LaFerla, 2010). It is the most common form of dementia (Barnes and Yaffe, 2011)and estimates suggest that as of 2015, there were 47 million people worldwide living with AD, a number that is projected to rise to 131 million by 2050 (Rizzi et al., 2014; Baumgart et al., 2015). Several clinical and neuropathological features of dementia and AD may also be evident with the normal progression of aging, making distinction of abnormal development of dementia from normal brain aging challenging. In AD, there is a long prodromal period during which the disease progresses sub-clinically for decades (Chertkow et al., 2013). When clinical symptoms eventually become apparent, pathology in the brain is well established and intervention is seldom effective and can only slow progression of the disease (Casey et al.,2010). The ability to identify AD as early as possible would provide patients and clinicians with opportunities to intervene prior to the establishment of irreversible neuropathology.The characterization of mild cognitive impairment (MCI) as a clinical entity, distinct from AD, but also considered abnormal(Petersen et al., 1999; Grundman et al., 2004) allowed for the definition of a pattern of decline that was similar to, but divergent from normal aging. After 60 years of age, impairments of some cognitive abilities such as processing speed, working memory and executive functions become apparent, while others, such as short-term memory, autobiographical knowledge and emotion processing remain relatively intact (Hedden and Gabrieli, 2004; Folstein and Folstein, 2010). Patients with MCI are said to have alterations in cognition with noticeable decline, while retaining functional independence (Winblad et al., 2004). A diagnosis of dementia due to AD is made when a patient’s cognitive decline is so severe that it diminishes independent living (Swerdlow, 2011). Generally, healthy aging is associated with moderate decline in some cognitive abilities, whilst AD is characterized by severe deterioration of the same cognitive domains, with additional progressive decline of further cognitive functions, such that the patient’s personal,professional and social life is adversely affected to a severe degree (McKhann et al., 2011; Swerdlow, 2011). The concept of “subjective cognitive decline” has been investigated in recent years as an even earlier indication of AD (Rabin et al.,2017) and evidence suggests that subjective cognitive decline may predict faster conversion to MCI and AD (Fernandez-Blazquez et al., 2016).
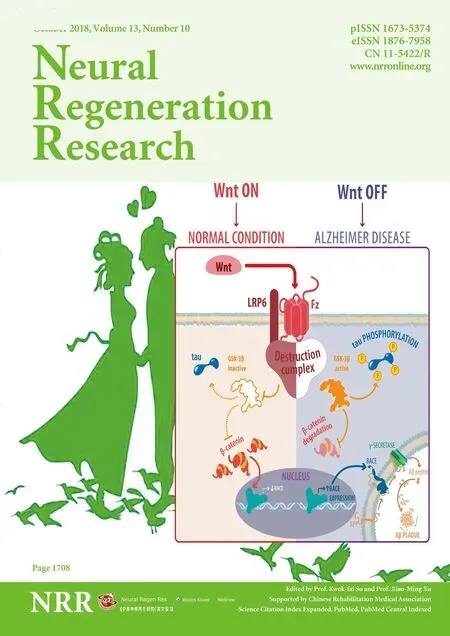
Plaques and Tangles Are Poor Correlates of Cognitive Decline in AD
Traditional neuropathological lesions in AD brain include senile plaques, consisting of aggregated amyloid-β (Aβ) and neurofibrillary tangles (NFT) of tau protein, which accumulate extracellularly and intraneuronally, respectively (De-Paula et al., 2012; Reitz and Mayeux, 2014). Enhanced neuroinflammation is also consistently observed in AD (McGeer and McGeer, 2013; Meraz-Rios et al., 2013) and evidence suggests that early hyperactivity of pro-inflammatory pathways in the brain precedes the development of plaques and tangles in AD(Tarkowski et al., 2003; Ferretti and Cuello, 2011; Wright et al., 2013). Muddying the waters, however, is the fact that aging itself is associated with similar aberrations in the brain, that may or may not lead to cognitive deterioration. Accumulating evidence suggests that Aβ plaques and neurofibrillary tau tangles are not uncommon in the brains of non-demented,cognitively healthy older people (Price and Morris, 1999; Savva et al., 2009; Malek-Ahmadi et al., 2016). Evidence has also shown that Aβ deposition correlates poorly with cognitive impairment in elderly cohorts (Terry et al., 1991; Aizenstein et al., 2008; Malek-Ahmadi et al., 2016), suggesting that Aβ per se does not directly influence cognitive function. Indeed, we recently found that although Aβ deposition was significant in brains of aged APP/PS1 mice, a model of AD, and virtually absent from age-matched controls, both groups of aged mice performed equally poorly on several cognitive tasks (Denver et al., 2018). Although the amyloid cascade hypothesis remains the dominant paradigm that attempts to explain the pathogenesis of AD (Hardy and Allsop, 1991; Hardy and Higgins, 1992;Hardy and Selkoe, 2002), consistent anti-amyloid drug trial failures have bolstered criticism of the model that considers misprocessing of amyloid the central pathological event in AD(Drachman, 2014; Herrup, 2015). Musiek and Holtzman (2015)reviewed recent evidence for and against the amyloid cascade hypothesis and concluded that Aβ was critical, but not sufficient for the development of AD. They proposed an updated model that incorporates the idea that a balance is maintained throughout life between production and clearance of Aβ in the brain. Factors that increase AD risk occurring in midlife then contribute to disruption of this homeostatic balance, which leads to overproduction and reduced clearance of Aβ and subsequent pathological cascades and clinical signs of the disease(Musiek and Holtzman, 2015). In any case, improvements in cognitive performance can occur independently of effects on Aβ (Kotilinek et al., 2002; Hock et al., 2003; Chen et al., 2007)and reductions of Aβ pathology don’t always correlate with improved cognition, nor does reducing amyloid burden always slow progression of neurodegeneration (Holmes et al., 2008;Kokjohn and Roher, 2009). It seems more and more likely that amyloid, particularly in the insoluble plaque form, is not the necessary and sufficient factor initially posited by Hardy and Allsop (1991), but rather a downstream event or byproduct of other known or unknown mechanisms in AD brain. Prefibrillar, soluble Aβ aggregates in the form of oligomers have recently been appreciated as specifically synaptotoxic and neurotoxic (Ferreira et al., 2015). In fact, it has been known for 20 years that the small, soluble aggregations of Aβ, described at the time as Aβ-derived diffusible ligands (ADDLs), are neurotoxic independent of larger Aβ fibrils and plaques and may mediate the progressive cognitive deterioration in AD (Lambert et al., 1998; Shi et al., 2016). Aβ oligomers (AβOs) have been included in more recent revisions of the amyloid cascade hypothesis (Klein et al., 2001; Hardy and Selkoe, 2002), suggesting that soluble AβOs, rather than larger fibrils or plaques,elicit synaptic toxicity and memory dysfunction (Ferreira and Klein, 2011; Gulisano et al., 2018). NFT of hyperphosphorylated tau protein in AD brain have been considered a more reliable correlate of cognitive decline in AD patients (Arriagada et al., 1992; Nelson et al., 2012). Tau is a microtubule-associated protein that supports and stabilizes the neuronal cytoskeleton (Brandt and Lee, 1993; Panda et al., 1995; Johnson and Stoothoff, 2004). In AD, aberrant hyperphosphorylation of tau reduces its ability to bind and stabilize microtubules (Lu and Wood, 1993) and promotes self-aggregation into paired helical filaments and subsequently, NFT (Garcia de Ancos et al., 1993; Johnson and Stoothoff, 2004). Hyperphosphorylated tau is also directly neurotoxic (Fath et al., 2002; Chun and Johnson, 2007) and neuronal apoptosis induced by tau aggregates is thought to at least partially underlie some of the degeneration and cognitive decline associated with AD (Ar-riagada et al., 1992; Johnson and Stoothoff, 2004). However,since tangles of hyperphosphorylated tau have frequently been observed in brains of non-demented individuals (Price et al.,1991; Price and Morris, 1999), it seems likely that while tau hyperphosphorylation may be involved with AD pathophysiology, tangle pathology may not be as reliably correlated with cognitive decline as previously thought. Several studies have shown that pre-tangle oligomeric tau species are elevated in neurons from AD brain (Tiernan et al., 2018), an effect that correlates negatively with cognitive function (Vana et al.,2011), suggesting that tau oligomers are toxic in AD brain and their levels may correlate more robustly with cognitive decline.
Classical pathological lesions in AD brain, amyloid and tau deposits are used as measures of disease progression and also as an indicator of therapeutic efficacy. However, given the paucity of consistent correlations between these markers and cognitive decline, future studies may wish to consider alternative pathological measures, including oligomeric amyloid and tau. Additionally, in pre-clinical studies, investigators should consider the possibility that non-transgenic control animals may also develop similar age-dependent pathologies in the brain. Future experimental designs should include additional groups of younger animals, such that age-dependent changes in cognitive function or brain pathologies in control animals can be identified.
Is Spatial Learning Particularly Susceptible to Alzheimer’s Pathology?
With advancing age, impairments of some cognitive abilities become increasingly apparent, while others remain relatively intact in otherwise healthy individuals (Folstein and Folstein,2010). Spatial learning impairments, using the Morris water maze, have been well-documented in the APP/PS1 mouse model of AD, at 12 (Harrison et al., 2009; Xiao et al., 2016),13–14 (Jia et al., 2013; Fol et al., 2016) and 22–24 (Harrison et al., 2009; Xiao et al., 2016) months of age, while learning has been found to be unimpaired in APP/PS1 mice aged 7 months (O’Reilly and Lynch, 2012). Recently, we demonstrated impaired spatial learning in 15–18 month-old APP/PS1 mice, compared to ‘healthy’, age-matched controls,while spatial memory retention and recognition memory were similarly impaired in both groups (Denver et al., 2018). This suggests that spatial learning is a cognitive process that is especially defective in AD. Reversal learning was notably impaired in APP/PS1 mice (Denver et al., 2018), similar to findings in younger APP/PS1 mice (O’Reilly and Lynch, 2012; Cheng et al., 2014), suggesting that cognitive flexibility is vulnerable to the effects of AD pathology. Given the memory impairments in aged wild-types, as well as transgenic mice, it seems reasonable to suggest that spatial and recognition memory are deleteriously affected with aging, while spatial learning is distinctly vulnerable to AD pathology (Denver et al., 2018). Interestingly, certain spatial cognitive domains are also known to be impaired in aged C57Bl/6 mice (Barreto et al., 2010; Shoji et al., 2016).
Other amyloidogenic mouse models of AD show similar alterations in cognitive function. Age-dependent deficits of
spatial learning have been detected in tg-ArcSwe mice, which express both Arctic and Swedish mutations of APP (Lord et al., 2009). Some (Wolf et al., 2016; Portbury et al., 2017), but not all (Bizon et al., 2007) have observed learning and memory impairments in aged adult Tg2576 mice, while early cognitive deficits have been detected in the 3xTg AD model (Stover et al., 2015). Most AD mouse models develop spatial learning and memory impairments, however AD is a complicated basket of interconnected pathologies, making identification of the precise cause of AD-related cognitive dysfunction challenging.Recent appreciation for impaired spatial navigation as a cognitive domain that can distinguish incipient AD or MCI from aging in humans (Lithfous et al., 2013; Coughlan et al., 2018)has spurred empirical investigation, results of which suggest that this may indeed be the case (Allison et al., 2016). These findings may inform future clinical and pre-clinical AD research and may support clinicians in identifying early patterns of cognitive decline that are divergent from normal aging.
Synaptic Loss in AD and Aging
Synapse loss consistently correlates with cognitive decline in AD (Terry et al., 1991; Shankar and Walsh, 2009; Robinson et al., 2014). Several studies have shown that synapse density is decreased in the brains of 5–8 month-old APP/PS1 mice(McClean et al., 2011; Zhang et al., 2014; Li et al., 2015; Liu et al., 2016), while others report reduced synapse density in brains of 18–24-month-old APP/PS1 mice, compared to age-matched wild-types (Ostapchenko et al., 2015; Zhang et al., 2016). However, one report showed that synaptophysin levels in the hippocampus of 7- and 17-month-old APP/PS1 mice were similar to age-matched wild-types (Minkeviciene et al., 2008). Our results suggest that hippocampal and cortical synapse density is comparable between 15–18 month-old wild-types and APP/PS1 mice (Denver et al., 2018), possibly reflecting age-related synapse loss. A number of the aforementioned studies identified reduced synaptophysin levels using western blot assay of hippocampal and cortical homogenates(Li et al., 2015; Liu et al., 2016; Zhang et al., 2016) or by quantitative analysis of synaptophysin immunofluorescence throughout the whole hippocampus (Li et al., 2015; Ostapchenko et al., 2015). Unlike methods utilized by Denver et al. (2018), neither of these methods considered the discrete cellular layers of the hippocampus and therefore may have overlooked subtle variation in synapse density between subregions in APP/PS1 and wild-type mice. It has been shown in Tg2576 mice that synaptophysin levels were no different from controls at 3, 9, 14 and 19 months of age (King and Arendash,2002). Additionally, evidence suggests that synaptophysin levels are unaffected in the hippocampus of human patients with AD (Tannenberg et al., 2006; Counts et al., 2012). In aged APP/PS1 mice, Malthankar-Phatak et al. (2012) failed to detect reduced synaptophysin staining in the hippocampal molecular layer or neocortical areas, even at 24–27 months of age, results that more closely align with our findings (Denver et al., 2018). We did, however, detect reduced synaptophysin staining in the polymorphic hilar layer of the dentate gyrus in aged APP/PS1 mice, compared to controls (Denver et al.,2018). Others have shown AD-related synapse loss in the inner (Scheff and Price, 1998) and outer (Scheff et al., 1996;Alonso-Nanclares et al., 2013) molecular layers of the dentate gyrus. Synapse loss in the outer molecular layer and layers II and III of the entorhinal cortex has also been demonstrated in Tg2576 mice by electron microscopy, while synaptophysin levels remained unchanged (Dong et al., 2007). There are several potential explanations for the variation in the findings from the aforementioned studies. First of all, markers typically utilized when measuring synapse density in the brain represent functional proteins in either the pre- or post-synaptic terminal. In AD and aging, reductions of synaptic marker levels may represent loss, dysfunction or mislocalisation of distinct synaptic proteins, rather than a general loss of synapses.Furthermore, there are a huge number of synaptic proteins that comprise synapses, the majority of which can be used as biomarkers of synapse density. This means that depending on a single or even several markers to assess synapse density may be problematic if there are selective alterations of distinct proteins, rather than simply synapse loss, as has been reported (Tannenberg et al., 2006). Secondly, AD and aging may be associated with a loss of pre- or post-synaptic terminals at different stages as the disease or age progresses. Counts et al.(2012) found that pre-synaptic synaptophysin and synaptotagmin were unaltered in the hippocampus of AD and MCI patients, whereas post-synaptic drebrin was reduced. Had the authors failed to include drebrin in their analysis, they may have erroneously concluded that MCI and early AD is not associated with synapse loss in the hippocampus (Counts et al.,2012). The third potential reason for the inconsistent findings is the regional heterogeneity of synapse loss in the brain with aging and in AD. There is a general consensus that synapse loss is primarily apparent in the hippocampus, as well as frontal and temporal cortices of AD patients (Clare et al., 2010),however these anatomical regions consist of a number of distinct subregions that are connected with other areas within complex neuronal circuits. Inconsistencies may arise in the literature simply as a result of investigators not looking in the correct place within the brain, or not looking closely enough.Where possible, studies that measure synapse density using antibody-mediated immunostaining or biochemical assays may also wish to examine synapse ultrastructure using electron microscopic techniques, with which functional synaptic contacts can be directly visualized (Dong et al., 2007; Neuman et al.,2015).
The polymorphic layer of the dentate gyrus contains several different types of neuron, the most abundant of which is the mossy cell neuron (Amaral et al., 2007). Mossy cells in the hilus provide inhibitory and excitatory input to neurons in the adjacent granule cell layer (Buckmaster et al., 1996). They also form synaptic connections with another polymorphic layer cell, the GABAergic inhibitory interneuron, which in turn can inhibit granule cell neurons (Scharfman, 1995). This complex network of inhibitory and excitatory activity is thought to underlie certain forms of associative memory and pattern separation (Myers and Scharfman, 2011; Scharfman and Myers, 2012). The decrease in synaptophysin levels in the polymorphic layer of aged APP/PS1 mice (Denver et al., 2018)could indicate a reduction in mossy cell synaptic contact with inhibitory interneurons, which would result in disinhibition of granule cell neurons and disruption of the fine balance of inhibitory and excitatory neuronal activity required for effective cognitive functioning. It has been shown that enhancing GABAergic innervation in the dentate gyrus improves reversal learning in mice (Morellini et al., 2010). The consequences of synaptic dysfunction within this discrete subregion of the hippocampus remain to be fully determined. Based on our results,one may speculate that hilar synapse loss is responsible for the observed impairment in spatial learning, particularly reversal learning, since the neural network associated with the hilus of the dentate gyrus is involved with pattern separation and reversal learning (Scharfman and Myers, 2012).
Aging in humans is also associated with reduced levels of synaptic proteins related to structural plasticity of axons and dendrites, while in human AD brain there is an additional reduction of postsynaptic drebrin (Hatanpaa et al., 1999).Age-related correlations between hippocampal synapse loss and cognitive decline are known to exist (Nicholson et al.,2004; Nyffeler et al., 2007; Long et al., 2009), although some report a lack of such a relationship (Geinisman et al., 2004).Age-related deficits in hippocampal long-term potentiation(LTP) have also been identified (Deupree et al., 1993; Barnes et al., 1997; Bouet et al., 2011), suggesting that a decline in synaptic function with age, rather than synapse density as such,is more closely linked with cognitive decline. Support for this proposal has been presented in several reports that demonstrated a reduction, as a consequence of aging, of pre- and post-synaptic components required for efficient functioning of synapses in the hippocampus (Canas et al., 2009; Long et al.,2009; VanGuilder et al., 2010). Conversely, increased expression of synaptic proteins is associated with superior learning in aged animals (Colombo and Gallagher, 2002; Menard and Quirion, 2012). These studies demonstrate the importance of intact, functional synapses, particularly in the hippocampus, in learning and memory. Deterioration of synaptic integrity and synapse loss in AD brain and with aging may explain at least some of the cognitive deficits apparent in animal models and humans. Comparing synapse loss in AD brain with that associated with aging will require delineation of regional vulnerability of synapses to aging or AD pathology and correlations with specific cognitive deficits. It should also be remembered that synaptic biomarkers represent functional proteins within the synapse and modulation of these proteins may reflect dysfunction of the protein itself, rather than loss of the entire synapse. Pre- and post-synaptic terminals and the proteins of which they are comprised likely respond differently to AD and aging pathologies. Inclusion of at least one pre-synaptic and one post-synaptic marker would provide more reliable insights into synaptic dysfunction associated with AD and aging.Where possible examining synaptic ultrastructure with electron microscopy would also greatly enhance the reliability of future research.
The Complexity of Neuroinflammation in AD and Agin
Microglia and astrocytes are able to initiate an inflammatory response to injury in the central nervous system (CNS) (Kreutzberg, 1996; Schilling et al., 2003; Rezai-Zadeh et al., 2009). Aβ rapidly activates microglia, such that their morphological and phenotypic characteristics are altered to promote phagocytosis and induce a focal inflammatory response, leading to recruitment of other immune cells (Koenigsknecht and Landreth,2004; Meraz-Rios et al., 2013). Activated microglia phagocytose Aβ and reduce amyloid burden (Bard et al., 2000; Lee and Landreth, 2010; El-Shimy et al., 2015; Fu et al., 2016). However, sustained microglial activation and unresolved inflammation in the brain is harmful to neurons and synapses and promotes a state of chronic dysregulation of glial cells and subsequent deterioration of brain structure and function (Frank-Cannon et al., 2009; Steardo et al., 2015; Leszek et al., 2016). Aβ42can induce microglial phagocytosis of viable neurons (Neniskyte et al., 2011, 2016; Fricker et al., 2012) and phagocytic microglia are thought to contribute to synapse loss early in AD (Hong et al.,2016). Microglia secrete an array of pro-inflammatory cytokines and chemokines, such as interleukin (IL)-6, IL-1β, tumor necrosis factor α (TNF-α), macrophage inflammatory protein-1α(MIP-1α) and monocyte chemotactic protein 1 (MCP-1), when exposed to Aβ (Rogers and Lue, 2001; Patel et al., 2005; Tuppo and Arias, 2005). This leads to recruitment and activation of astrocytes and peripheral immune cells (Rezai-Zadeh et al., 2009).Astrocytes are also recruited to Aβ plaques (Wyss-Coray et al.,2003) and are also capable of degrading Aβ (Nagele et al., 2003;Wyss-Coray et al., 2003; Koistinaho et al., 2004), albeit less efficiently than microglia (Mandrekar et al., 2009). Although it has been posited that astrocyte migration is induced by Aβ-mediated injury to adjacent neurons, as opposed to Aβ per se (Galea et al., 2015).
Inflammation in the brain increases with age (Lynch, 2010;Gabuzda and Yankner, 2013) and several studies report elevated levels of inflammatory cytokines in brains of aged rodents(Ye and Johnson, 1999; Maher et al., 2004; Godbout et al.,2005). Since aging is also associated with systemic augmentation of inflammation (Franceschi et al., 2007) it is thought that circulating inflammatory mediators prime microglia in the aging brain (Perry, 2004; Dilger and Johnson, 2008; Norden and Godbout, 2013; Matt and Johnson, 2016). Primed microglia are more pro-inflammatory at baseline, are more sensitive to secondary immune challenges and generate an exaggerated inflammatory response (Lull and Block, 2010; Norden et al.,2015; Wendeln et al., 2018). In the context of AD, primed microglia respond more readily to Aβ, producing enhanced levels of cytokines and exerting direct toxic effects on neurons and at synapses (Hong et al., 2016; Spangenberg et al., 2016).Therefore, dysregulation of the systemic and central immune system that accompanies aging can serve as a chronic priming stimulus for microglia (Godbout et al., 2005; Norden and Godbout, 2013; Wendeln et al., 2018); a mechanism that could mediate the increased risk of AD with age (Querfurth and LaFerla, 2010).
Polymorphisms in genes encoding several cytokines are strongly associated with increased risk of AD, including IL-1β,IL-6, interferon γ (IFNγ), IL-4 and IL-10 (Licastro et al., 2007;Zhang et al., 2011; Hua et al., 2013; Zheng et al., 2016; Dong et al., 2017), suggesting an association between cytokines and either protection against or propagation of AD pathogenesis.In our recent study we found comparable levels of inflammatory cytokines in the brain of aged wild-type and APP/PS1 mice, with the exception of IFNγ and IL-4, which were both elevated in APP/PS1 mice (Denver et al., 2018). The similarities in inflammatory profile in the brain of aged mice may be related to the general enhancement of neuroinflammation evident with aging. Elevated IFNγ has been shown previously in the brain of younger APP/PS1 mice, the cellular source of which was infiltrating Aβ-specific T cells (Browne et al., 2013).Interestingly, adoptive transfer of Th1-producing T cells to APP/PS1 mice resulted in microglial activation, increased Aβ deposition and cognitive dysfunction (Browne et al., 2013).Given the negative correlation, demonstrated in our study,between brain IFNγ levels and recognition memory (Denver et al., 2018), it may be that enhanced brain levels of IFNγ has a direct negative impact on cognitive function in AD. In any case, it appears that IFNγ and IL-4 were specifically increased in the brains of APP/PS1 mice, presumably as an effect of AD pathology. Increased brain levels of IFNγ has also been shown in APPswemice aged 3 and 19 months (Abbas et al.,2002), however brain IL-4 was down-regulated in this study,contrary to our findings. Th2 cytokine IL-4 plays a role in suppressing Th1 immune responses (Luzina et al., 2012), as such, our findings may represent protective upregulation of IL-4 in the brains of APP/PS1 mice as a response to elevated levels of IFNγ (Denver et al., 2018), while results of Abbas et al. (2002) might reflect a failure of this protective response in APPswemice. Important sources of IFNγ and IL-4 include T lymphocytes (Castro et al., 2018). It is possible that circulating or infiltrating T cells or macrophages in the CNS are responsible and may be involved in the pathophysiology of AD, a proposition that is increasingly under investigation (Browne et al., 2013). Microglia and astrocytes also produce IFNγ (Lau and Yu, 2001; Kawanokuchi et al., 2006; Wang and Suzuki,2007; Sa et al., 2015), while evidence suggests that although astrocytes may not produce IL-4, they do express the IL-4 receptor, through which they respond to IL-4 by suppressing inflammatory activation and augmenting growth factor production (Brodie et al., 1998; Liu et al., 2000). Sources of IL-4 in the brain include microglia and neurons (Zhao et al., 2015;Lee et al., 2016). Neuronal IL-4 has been shown to induce a restorative M2-like phenotype in microglia (Fernandes et al.,2014; Zhao et al., 2015), while Latta et al. (2015) also showed that IL-4 was involved in the induction of an M2a phenotype in microglial cells and in the brains of APP/PS1 mice. Together this suggests that IL-4, possibly derived from microglia,neurons or infiltrating T cells, exerts neuroprotective effects in models of brain injury, including AD. Intriguingly, IL-4 may also exert direct, beneficial effects on cognitive function(Gadani et al., 2012), suggesting that the clinical manifestation of AD or age-related cognitive decline may be associated with direct effects of cytokines, including IL-4 (McAfoose and Baune, 2009; Derecki et al., 2010).
Pro-inflammatory IL-1β has been consistently associated with AD (Mrak and Griffin, 2001; Shaftel et al., 2008). Several reports indicate that IL-1β is up-regulated in plasma from MCI and AD patients (De Luigi et al., 2002; Forlenza et al.,2009; Brosseron et al., 2014)and previous studies have detected increased levels of IL-1β in brains of APP/PS1 mice(Gallagher et al., 2013; Yan et al., 2013; Guo et al., 2015; Xuan et al., 2015). An inactive precursor of IL-1β (pro-IL-1β) is present in glial cells in the brain (Shaftel et al., 2008) and activation of IL-1β is dependent on caspase-1 cleavage of pro-IL-1β (Halle et al., 2008). Theinflammasome NLRP3 detects danger signals through toll-like receptor 4 (TLR4) signaling in astrocytes and microglia (Alfonso-Loeches et al., 2014, 2016).It has been demonstrated thatAβ stimulates IL-1β production and secretion via NLRP3-dependent cleavage of pro-IL-1β by caspase-1 (Halle et al., 2008; Salminen et al., 2008; Heneka et al., 2013; Parajuli et al., 2013), providing a reasonable mechanistic explanation for the elevated levels of IL-1β in AD brain.However, elevated levels of IL-1β have also been shown in brains of senescence-accelerated SAMP8 mice (Tha et al.,2000) and in aged rat brain (Gee et al., 2006; Campuzano et al.,2009). We also detected elevated IL-1β in brains of both aged C57Bl/6 and APP/PS1 mice, compared to young wild-type mice (Denver et al., 2018). In addition, IL-1β has been shown to suppress hippocampal LTP (Vereker et al., 2000; Griffin et al., 2006; Hoshino et al., 2017; Prieto et al., 2018), suggesting that IL-1β might partially mediate cognitive dysfunction in aging and AD.
Perturbed Insulin Signaling in AD Brain
A reciprocal relationship exists between AD risk and type 2 diabetes mellitus (T2DM), another disease associated with aging (Janson et al., 2004; Mittal and Katare, 2016). One of several similarities with AD, inflammation is also an important feature of T2DM pathophysiology (Lontchi-Yimagou et al.,2013). Resistance of systemic tissues, such as adipose tissue and pancreas, to the hormone insulin is another significant feature of T2DM (Taylor, 2012). Activation of the insulin receptor (IR) is followed by recruitment of insulin receptor substrate (IRS) proteins intracellularly, usually IRS-1 or IRS-2(White, 2003; Boura-Halfon and Zick, 2009). The insulin-mediated signaling cascade then continues via phosphatidylinositol 3-kinase (PI3K) and protein kinase B (Akt), among several others, eliciting downstream effects through phosphorylation and activation of other kinasesand effector molecules (Siddle,2011). Normal inhibition of IRS-1 is a means by which insulin signaling is regulated and is mediated by mitogen-activated protein kinases (MAPK), such as extracellular signal-regulated kinases (ERK), c-Jun N-terminal kinases (JNK) and inhibitor of nB kinase (IKK) (Gao et al.,2002, 2004; Boura-Halfon and Zick, 2009). This down-regulation of insulin signaling can occur through phosphorylation of serine residues on IRS-1, including those at positions 307 (Hirosumi et al., 2002), 312 (Gao et al., 2002) and 616 (Talbot et al., 2012). These intracellular kinases can be modulated by extracellular factors such as oxidative and nitrosative stress, inflammatory mediators and Aβ oligomers (Dineley et al., 2001; Andreozzi et al., 2007; Giordano et al., 2008; Bomfim et al., 2012), which, through activation of respective membrane-bound receptors, are able to influence inhibitory serine phosphorylation of IRS-1. Aging itself is associated with development of glucose intolerance and insulin resistance (Fink et al., 1983; Rowe et al., 1983; Paolisso et al.,1999; Barbieri et al., 2001). Park et al. (2013) identified numerous insulin signaling genes that were down-regulated in aged rodents and other reports suggest that insulin insensitivity and glucose intolerance also exists in aged animals (Catalano et al.,2005; Yamamoto and Otsuki, 2006; Romanatto et al., 2014),including C57Bl/6 mice (Houtkooper et al., 2011; Lipina et al.,2016). Insulin resistance has been demonstrated in postmortem brain tissue from AD and MCI patients, in the absence of diabetes and irrespective of apolipoprotein E (ApoE)-ε4 status(Talbot et al., 2012). Furthermore, IRS-1 pSer616and IRS-1 pSer636/639were identified as putative biomarkers of brain insulin resistance in AD and were found to correlate positively with Aβ oligomer levels and negatively with cognitive function(Talbot et al., 2012). Another study showed similar results in human AD brain tissue and also found that stimulation of primate hippocampus and hippocampal neuronal cultures with Aβ oligomers, increased levels of IRS-1 pSer636and activated JNK; a stress kinase that phosphorylates IRS-1 at serine residues (Bomfim et al., 2012). Other studies have also demonstrated impaired neuronal insulin signaling in AD brain and in response to Aβ oligomer challenge at the level of the IR and insulin-like growth factor-1 (IGF-1) receptor, IRS-1, IRS-2,PI3K and Akt (Zhao et al., 2008; Moloney et al., 2010; Liu et al., 2011). In the brain, insulin signaling encourages proliferation, differentiation, neurite growth and is anti-apoptotic and neuroprotective (Blazquez et al., 2014). Furthermore, insulin modulates the structure and function of synapses, neurons and neural circuits and has a well-established role in enhancing learning and memory (Blazquez et al., 2014). This suggests that insulin resistance in the brain can exist as a distinct phenomenon, independent of peripheral insulin resistance and glucose intolerance (Bomfim et al., 2012; Talbot et al., 2012).This also implies that diminished responsiveness to insulin in the brain has different consequences than in peripheral tissues.Our data shows that peripheral insulin and glucose tolerance were comparable between aged wild-type and APP/PS1 mice,while IRS-1 pSer616levels were increased in the brain of APP/PS1 mice (Denver et al., 2018). This provides some support for the suggestion that insulin resistance in brain may indeed exist as a distinct phenomenon, separate from insulin signaling in the periphery and one that can distinguish AD from normal aging.
Perspectives and Future Directions
The differentiation of normal brain aging from development of AD is necessary to allow for the categorization of risk of progression from MCI to AD. This will identify potential treatment windows and inform decisions regarding lifestyle interventions aimed at reducing the risk of developing AD. The role of inflammation in AD is complex, with dichotomous functions in the preservation or deterioration of brain structure and function. Clinical success for pharmacological inter-ventions in AD that either boost or suppress inflammatory responses in the brain have been relatively sparse, ie. amyloid immunization and NSAID trials. Glial cells function as active immune cells and protect the CNS from pathogenic insults,including Aβ, however, persistent immunological activation of these cells drives the development of a neurotoxic pro-inflammatory environment and reduces their ability to function as homeostatic regulators in brain. In addition to the direct toxic effects elicited by pro-inflammatory glial cells, future research should also consider the potential gaps in potassium buffering, lactate shuttling, glutamate recycling and synaptic stripping that may be evident within the inflammatory milieu of AD brain. Such studies would illuminate novel therapeutic potential aimed at maintaining or restoring homeostatic functions of multifunctional glial cells, rather than broad inhibition or stimulation. In addition to CNS-resident glial cells, future studies should address the contribution of peripheral immune cells, such as lymphocytes and neutrophils, to the neuroinflammatory environment in AD brain. This systemic immune response may be beneficial or harmful to the integrity of the CNS in AD and greater understanding may help to identify novel therapeutic targets for a disease in which effective treatment is notoriously difficult. Dysregulated insulin signaling in AD brain has been recently appreciated and our work supports the proposition that brain insulin resistance distinguishes AD from healthy aging. Further work is needed to clarify the precise molecular and cellular players in this story. Future investigations should determine changes in kinase and phosphatase activity that develop in AD brain, particularly those that interact with IRS-1. Moreover, what are the functional consequences of downregulated insulin signaling in the brain? Likely effects include increased neuronal apoptosis, tau hyperphosphorylation and cognitive dysfunction, however, the complexity of AD makes it difficult to delineate direct cause and effect pathways. Insulin-sensitizing drugs may prove efficacious in treating AD and early clinical trial data suggest that incretin hormone derivatives do indeed have several positive effects in brain. Finally, we identified spatial learning as a particularly defective cognitive domain specifically in AD mice. Although it is well-known that spatial learning and memory is impaired in AD, aged control mice performed equally poorly to AD mice on tasks that required memory recall, suggesting that while ‘normal’ aging is associated with decline of memory function, spatial learning is relatively retained compared to AD mice. This finding may inform future research aiming to develop diagnostic tools that will allow clinicians to more comprehensively and efficiently identify patterns of cognitive decline that precede dementia.
A diagnosis of AD is usually made late in the progression of the disease. The extended prodromal stages of AD are generally considered sub-clinical or asymptomatic and any noticeable alterations in cognitive functions or neuropsychiatric status are attributed to normal aging. Earlier identification of abnormal cognitive decline or biomarker irregularities would allow for earlier diagnosis, informing lifestyle changes or novel treatment approaches aimed at reducing risk of progression to AD or delaying the age of clinical onset of this devastating disease.
Author contributions: PD and PLMc both contributed equally to this work, including writing, researching and revising the manuscript.
Conflicts of interest: Some of the data from Denver et al. (2018) has been submitted, in abstract form, to the 2017 Southern California Alzheimer’s Disease Centers Research Symposium at the University of California, Beckman Center of the National Academies of Sciences &Engineering, Irvine, CA, USA.
Financial support: This work was supported by the Department of Education and Learning, Northern Ireland.
Copyright license agreement: The Copyright License Agreement has been signed by all authors before publication.
Plagiarism check: Checked twice by iThenticate.
Peer review: Externally peer reviewed.
Open access statement: This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-Non-Commercial-ShareAlike 4.0 License, which allows others to remix, tweak,and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Open peer reviewers: Nobuyuki Ishibashi, Children’s National Health System, USA; Olga Chechneva, University of California, USA.
Additional file: Open peer review reports 1 and 2.
杂志排行
中国神经再生研究(英文版)的其它文章
- Validity and reliability of the Ocular Motor Nerve Palsy Scale
- Mitogen-activated protein kinase phosphatase 1 protects PC12 cells from amyloid beta-induced neurotoxicity
- High-frequency (50 Hz) electroacupuncture ameliorates cognitive impairment in rats with amyloid beta 1–42-induced Alzheimer’s disease
- Kaempferol attenuates cognitive deficit via regulating oxidative stress and neuroinflammation in an ovariectomized rat model of sporadic dementia
- Combined VEGF/PDGF improves olfactory regeneration after unilateral bulbectomy in mice
- Comparison of morphological and functional outcomes of mouse sciatic nerve repair with three biodegradable polymer conduits containing poly(lactic acid)