Central post-stroke pain due to injury of the spinothalamic tract in patients with cerebral infarction: a diffusion tensor tractography imaging study
2018-01-05SungHoJangJunLeeSangSeokYeo
Sung Ho Jang, Jun Lee, Sang Seok Yeo
1 Department of Physical Medicine and Rehabilitation, College of Medicine, Yeungnam University, Namku, Daegu, Republic of Korea
2 Department of Neurology, College of Medicine, Yeungnam University, Namku, Daegu, Republic of Korea
3 Department of Physical Therapy, College of Health Sciences, Dankook University, Chungnam, Republic of Korea
Central post-stroke pain due to injury of the spinothalamic tract in patients with cerebral infarction: a diffusion tensor tractography imaging study
Sung Ho Jang1, Jun Lee2, Sang Seok Yeo3,*
1 Department of Physical Medicine and Rehabilitation, College of Medicine, Yeungnam University, Namku, Daegu, Republic of Korea
2 Department of Neurology, College of Medicine, Yeungnam University, Namku, Daegu, Republic of Korea
3 Department of Physical Therapy, College of Health Sciences, Dankook University, Chungnam, Republic of Korea
Many studies using diffusion tensor tractography (DTT) have demonstrated that injury of the spinothalamic tract (STT) is the pathogenetic mechanism of central post-stroke pain (CPSP) in intracerebral hemorrhage; however, there is no DTT study reporting the pathogenetic mechanism of CPSP in cerebral infarction. In this study, we investigated injury of the STT in patients with CPSP following cerebral infarction,using DTT. Five patients with CPSP following cerebral infarction and eight age- and sex-matched healthy control subjects were recruited for this study. STT was examined using DTT. Among DTT parameters of the affected STT, fractional anisotropy and tract volume were decreased by more than two standard deviations in two patients (patients 1 and 2) and three patients (patients 3, 4, and 5), respectively, compared with those of the control subjects, while mean diffusivity value was increased by more than two standard deviations in one patient (patient 2). Regarding DTT con figuration, all affected STTs passed through adjacent part of the infarct and three STTs showed narrowing. These findings suggest that injury of the STT might be a pathogenetic etiology of CPSP in patients with cerebral infarction.
nerve regeneration; central post-stroke pain; cerebral infarction; spinothalamic tract; diffusion tensor imaging; neural regeneration
Introduction
Central post-stroke pain (CPSP) is a neuropathic pain syndrome occurring after stroke, characterized by stimulation-independent pain; shooting, lancinating, burning and electric shock-like sensation; and paresthesia (Devulder et al.,2002; Ofek and Defrin, 2007; Klit et al., 2009). Approximately, 8–14% of stroke patients have symptoms of CPSP (Kumar et al., 2009). There have been several theories for the pathogenesis of CPSP including central sensitization, neuronal excitability changes by disinhibition, alteration in spinothalamic tract function, thalamic changes, and in flammation of an involved neural tract (Cesaro et al., 1991; Wasner et al.,2008; Klit et al., 2009; Latremoliere and Woolf, 2009; Wang et al., 2017). In addition, many brain regions or structures including the cingulate gyrus, somatosensory cortex, inferior parietal lobe, lateral thalamus, spinothalamic tract (STT), and medial lemniscus have been suggested as being responsible for the pathogenesis of CPSP (Boivie et al., 1989; Vestergaard et al., 1995; Klit et al., 2009; Kumar et al., 2009; Hong et al.,2010b). However, it has not been fully elucidated so far.
Diffusion tensor tractography (DTT), derived from diffusion tensor imaging (DTI), provides three-dimensional visualization and estimation of the STT (Hong et al., 2010a; Jang and Kwon, 2016a, b). Many studies using DTT have demonstrated that injury of the STT is the pathogenetic mechanism of CPSP in some brain pathologies including intracerebral hemorrhage and traumatic brain injury (Seghier et al., 2005;Goto et al., 2008; Hong et al., 2010b, 2012; Seo and Jang, 2013,2014; Jang and Kwon, 2016a, b). However, no DTT study on patients with cerebral infarction has been reported so far.
In this study, we used DTT to investigate injury of the STT in patients with CPSP following cerebral infarction.
Subjects and Methods
Subjects
Five patients with cerebral infarct (two males, three females;mean age 61.6 years; range 59 to 65 years) and eight ageand sex-matched control subjects (four males; mean age 58 years; range 52 to 64 years) with no history of neurologic or psychiatric disease were randomly recruited for this study(Table 1). The inclusion criteria were as follows: (1) first-ever stroke, (2) central pain presenting the characteristics of neuropathic pain: stimulation-independent pain: shooting,lancinating, burning, electric shock-like sensation, and paraesthesia (crawling, itching, tingling sensation); stimulus evoked pain: hyperalgesia or allodynia by environmentalstimuli (Woolf and Mannion, 1999; Dworkin et al., 2003;Klit et al., 2009), and (3) no radiculopathy or peripheral neuropathy as confirmed by electromyography and nerve conduction study. The study protocol was approved by the Institutional Review Board of Yeungnam University (YUH 14-01-425) and the study was conducted retrospectively.

Table 1 Demographic and clinical characteristics of the patients
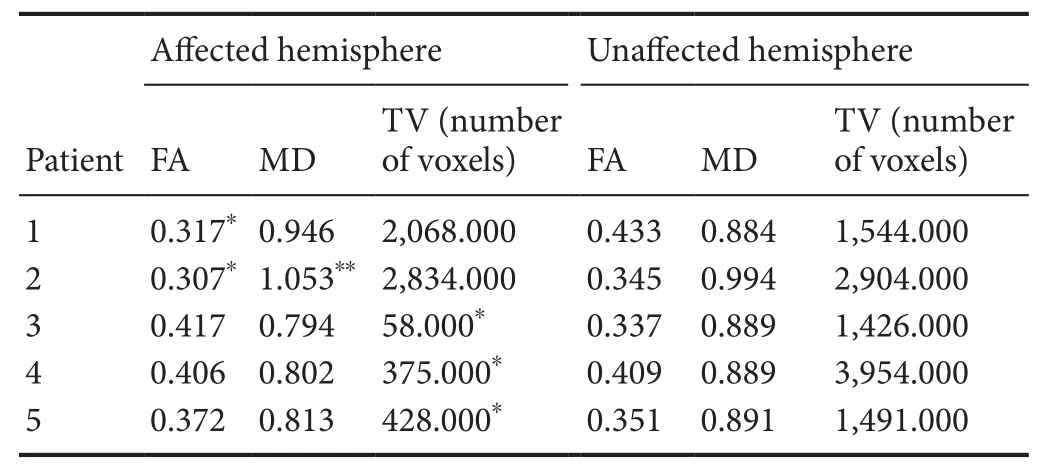
Table 2 Comparison of each parameter of diffusion tensor tractography in the spinothalamic tract between patients and control subjects
Diffusion tensor image
Acquisition of DTI data was performed at 11 days on average (range: 10–13 days) after stroke onset using a 6-channel head coil on a 1.5 T Philips Gyro scan Intera (Philips, Best,The Netherlands) and single-shot echo-planar imaging. For each of the 32 non-collinear diffusion sensitizing gradients,67 contiguous slices were acquired parallel to the anterior commissure-posterior commissure line. Imaging parameters were as follows: acquisition matrix = 96 × 96; reconstructed matrix = 192 × 192; field of view = 240 × 240 mm2; repetition time = 10,726 ms; echo time = 76 ms; parallel imaging reduction factor (SENSE factor) = 2; echo planar imaging(EPI) factor = 49;b= 1,000 s/mm2; number of excitations = 1;and a slice thickness of 2.5 mm with no gap (acquired voxel size 1.3 × 1.3 × 2.5 mm3).
Probabilistic fiber tracking
The Oxford Centre for Functional Magnetic Resonance Imaging of the Brain (FMRIB) Software Library (FSL; www.fmrib.ox.ac.uk/fsl) was used for analysis of diffusion-weighted imaging data, and affine multi-scale 2-dimensional registration was used for correction of head motion effects and image distortions due to eddy currents. Fiber tracking was performed using a probabilistic tractography method based on a multi- fiber model, and applied using tractography routines implemented in FMRIB Diffusion (5,000 streamline samples, 0.5 mm step length, curvature threshold = 0.2).
The STTs were identified by selecting fibers passing through both regions of interest (ROIs). A seed ROI was placed in the posterolateral medulla on an axial slice and a target ROI was placed at the primary somatosensory cortex(S1) on an axial slice (Hong et al., 2010a). DTI parameters(fractional anisotropy (FA) and mean diffusivity (MD)) of the whole STT were measured. DTI parameters showing a deviation of more than 2 standard deviations (SD) of that of normal control values were defined as abnormal based on confidence interval. Out of 5,000 samples generated from each seed voxel, results for each contact were visualized threshold and weightings of tract probability at a minimum of one streamline through each voxel for analysis. Values of FA, MD, and tract volume of the STTs were measured.
Results
Patient 1
A 62-year-old female was diagnosed with an infarct in the right corona radiata (Table 1). The patient showed severe numbness sensation on the left leg immediately after onset.The characteristics and severity of pain were as follows: constant tingling and pricking sensation without allodynia or hyperalgesia (visual analogue scale [VAS] score: 7)(Flaherty,1996). According to findings on 11-day DTT, FA value of the right STT was decreased by more than two standard deviations of those of control subjects. However, MD value and tract volume were within two standard deviations of those of control subjects (Table 2). The right STT ascended through the lateral portion of the infarct in the corona radiata (Figure 1).
Patient 2

Figure 1 T2-weighted MRI and diffusion tensor tractography of patients with CPSP following cerebral infarction.
A 59-year-old male underwent conservative management for an infarct in the right thalamus (Table 1). The patient complained of numbness sensation on the left arm immediately after onset. The characteristics and severity of pain were as follows: constant tingling sensation without allodynia or hyperalgesia (VAS score: 3). On 11-day DTT,FA and MD values of the right STT showed decrement and increment by more than two standard deviations of those of control subjects, respectively, while tract volume was within two standard deviations of that of control subjects (Table 2). The right STT passed through the anterior portion of the thalamic infarct (Figure 1)
Patient 3
A 59-year-old male was diagnosed as having an infarct in the right pre- and postcentral gyrus centered on the precentral knob and parieto-occipital lobe (Table 1). Since the day of the onset of infarct, the patient complained of stiffness sensation on the left arm. The characteristics and severity of pain were as follows: constant electric shock-like sensation without allodynia or hyperalgesia (VAS score: 3). On 11-day DTT, the right STT showed narrowing and decrement of tract volume by more than two standard deviations of those of control subjects. However, FA and MD value were within two standard deviations of those of control subjects (Table 2 and Figure 1).
Patient 4
A 65-year-old female underwent conservative management for an infarct in the right corona radiata (Table 1). The patient reported numbness sensation on the left finger and toe immediately after onset. The characteristics and severity of pain were as follows: constant tingling sensation without allodynia or hyperalgesia (VAS score: 2). On 13-day DTT, the right STT showed narrowing and tract volume was decreased by more than two standard deviations of that of control subjects, while FA and MD values were within two standard deviations of those of control subjects (Table 2 and Figure 1).
Patient 5
A 63-year-old female was diagnosed as having an infarct in the left thalamus (Table 1). Three days after onset, the patient began to complain of numbness sensation on the right hand and foot. The characteristics and severity of pain were as follows: constant tingling sensation with allodynia (VAS score: 3). On 10-day DTT, the left STT showed narrowing and decrement of tract volume by more than two standard deviations of that of control subjects, while FA and MD values were within two standard deviations of those of control subjects (Table 2 and Figure 1).
Discussion
In this study, injury of the STT in terms of DTT configuration and parameters was investigated in patients who showed CPSP following cerebral infarction. Regarding DTT con figuration, all affected STTs passed through the adjacent part of the infarct and three STTs showed narrowing, and signi ficant differences in DTT parameters of the affected STT were observed in patients with CPSP compared to the normal controls. The FA value represents the white matter organization, while the MD value indicates the magnitude of water diffusion, which can increase in some pathological forms(Assaf and Pasternak, 2008). The tract volume is determined by counting the number of voxels contained within a neural tract (Jang et al., 2013). Therefore, these changes of DTT parameters of the affected STT appeared to indicate an injury of the STT. These findings on DTT parameters appeared to be consistent with the finding of injury of affected STT on DTT con figuration. As a result, the present data suggest that injury of the STT induces CPSP following cerebral infarction.
Since introduction of DTI, several previous studies have reported on pathogenesis of CPSP in patients with intracerebral hemorrhage (Seghier et al., 2005; Goto et al., 2008; Hong et al., 2010b, 2012). In 2005, using DTI, Seghier et al. reported CPSP in a patient with intracerebral hemorrhage; the patient showed selective loss of the lateral thalamo-parietal fibers without injury of medial reticulo-thalamo-cortical fibers and spinothalamic pathway below the thalamus. In 2008, Goto et al. reported that only 24% of patients with CPSP showed interruption of the pathway of the STT, while 76% of patients showed preservation of intact integrity of the STT even with symptoms of CPSP. In 2010, Hong et al. demonstrated close association of development of CPSP in patients with intracerebral hemorrhage with the decrement of tract volume of STT in the affected hemisphere (Hong et al., 2010b). Subsequently, Hong et al. (2012) reported that prevalence of CPSP in patients with intracerebral hemorrhage was more common in partial injury of the STT, compared with complete injury of the STT. Consequently, to the best of our knowledge, this is the first study to demonstrate injury of the STT in patients with CPSP following cerebral infarction. However, limitations of this study should be considered. First, DTT analysis is operator dependent and may underestimate the fiber tracts due to fiber complexity and crossing fiber effect (Yamada et al., 2009). Second, the study included a small number of patients. Conduct of further studies involving large numbers of patients should be encouraged, and further studies comparing other brain pathologies with central pain, especially intracerebral hemorrhage, would also be necessary.
In conclusion, we found injury of the STT in the affected hemisphere in five patients who showed CPSP following cerebral infarction. Injury of the STT might be a pathogenetic etiology of CPSP in patients with cerebral infarction. Our results help to diagnose CPSP in patients with cerebral infarction and investigate the related pathogenetic mechanism.
Author contributions:SHJ and SSY designed this study, collected and analyzed data, wrote and revised the paper. SHJ and JL participated in study design and data collection. All authors approved the final version of this paper.
Con flicts of interest:None declared.
Research ethics:The study was approved by the Institutional Review Board of Yeungnam University Hospital (YUH 14-01-425). This study followed the principles of the Declaration of Helsinki.
Declaration of participant consent:The authors certify that they have obtained all appropriate participant consent forms. In the form, the participants have given their consent for their images and other clinical information to be reported in the journal. The participants understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Data sharing statement:Datasets analyzed during the current study are available from the corresponding author on reasonable request.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under identical terms.
Assaf Y, Pasternak O (2008) Diffusion tensor imaging (DTI)-based white matter mapping in brain research: a review. J Mol Neurosci 34:51-61.
Boivie J, Leijon G, Johansson I (1989) Central post-stroke pain--a study of the mechanisms through analyses of the sensory abnormalities. Pain 37:173-185.
Cesaro P, Mann MW, Moretti JL, Defer G, Roualdes B, Nguyen JP, Degos JD(1991) Central pain and thalamic hyperactivity: a single photon emission computerized tomographic study. Pain 47:329-336.
Devulder J, Crombez E, Mortier E (2002) Central pain: an overview. Acta Neurol Belg 102:97-103.
Dworkin RH, Backonja M, Rowbotham MC, Allen RR, Argoff CR, Bennett GJ, Bushnell MC, Farrar JT, Galer BS, Haythornthwaite JA, Hewitt DJ,Loeser JD, Max MB, Saltarelli M, Schmader KE, Stein C, Thompson D,Turk DC, Wallace MS, Watkins LR, Weinstein SM, et al. (2003) Advances in neuropathic pain: diagnosis, mechanisms, and treatment recommendations. Arch Neurol 60:1524-1534.
Flaherty SA (1996) Pain measurement tools for clinical practice and research. AANA J 64:133-140.
Goto T, Saitoh Y, Hashimoto N, Hirata M, Kishima H, Oshino S, Tani N,Hosomi K, Kakigi R, Yoshimine T (2008) Diffusion tensor fiber tracking in patients with central post-stroke pain; correlation with efficacy of repetitive transcranial magnetic stimulation. Pain 140:509-518.
Hong JH, Son SM, Jang SH (2010a) Identi fication of spinothalamic tract and its related thalamocortical fibers in human brain. Neurosci Lett 468:102-105.
Hong JH, Bai DS, Jeong JY, Choi BY, Chang CH, Kim SH, Ahn SH, Jang SH (2010b) Injury of the spino-thalamo-cortical pathway is necessary for central post-stroke pain. Eur Neurol 64:163-168.
Hong JH, Choi BY, Chang CH, Kim SH, Jung YJ, Lee DG, Kwon YH, Jang SH (2012) The prevalence of central poststroke pain according to the integrity of the spino-thalamo-cortical pathway. Eur Neurol 67:12-17.
Jang SH, Kwon HG (2016a) Traumatic axonal injury of the medial lemniscus pathway in a patient with traumatic brain injury: validation by diffusion tensor tractography. Neural Regen Res 11:130-131.
Jang SH, Kwon HG (2016b) Degeneration of an injured spinothalamic tract in a patient with mild traumatic brain injury. Brain Inj 30:1026-1028.
Jang SH, Chang CH, Lee J, Kim CS, Seo JP, Yeo SS (2013) Functional role of the corticoreticular pathway in chronic stroke patients. Stroke 44:1099-1104.
Klit H, Finnerup NB, Jensen TS (2009) Central post-stroke pain: clinical characteristics, pathophysiology, and management. Lancet Neurol 8:857-868.
Kumar B, Kalita J, Kumar G, Misra UK (2009) Central poststroke pain: a review of pathophysiology and treatment. Anesth Analg 108:1645-1657.
Latremoliere A, Woolf CJ (2009) Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J Pain 10:895-926.
Ofek H, Defrin R (2007) The characteristics of chronic central pain after traumatic brain injury. Pain 131:330-340.
Seghier ML, Lazeyras F, Vuilleumier P, Schnider A, Carota A (2005) Functional magnetic resonance imaging and diffusion tensor imaging in a case of central poststroke pain. J Pain 6:208-212.
Seo JP, Jang SH (2013) Traumatic thalamic injury demonstrated by diffusion tensor tractography of the spinothalamic pathway. Brain Inj 27:749-753.
Seo JP, Jang SH (2014) Injury of the spinothalamic tract in a patient with mild traumatic brain injury: diffusion tensor tractography study. J Rehabil Med 46:374-377.
Vestergaard K, Nielsen J, Andersen G, Ingeman-Nielsen M, Arendt-Nielsen L, Jensen TS (1995) Sensory abnormalities in consecutive, unselected patients with central post-stroke pain. Pain 61:177-186.
Wang CC, Shih HC, Shyu BC, Huang AC (2017) Effects of thalamic hemorrhagic lesions on explicit and implicit learning during the acquisition and retrieval phases in an animal model of central post-stroke pain. Behav Brain Res 317:251-262.
Wasner G, Lee BB, Engel S, McLachlan E (2008) Residual spinothalamic tract pathways predict development of central pain after spinal cord injury. Brain 131:2387-2400.
Woolf CJ, Mannion RJ (1999) Neuropathic pain: aetiology, symptoms,mechanisms, and management. Lancet 353:1959-1964.
Yamada K, Sakai K, Akazawa K, Yuen S, Nishimura T (2009) MR tractography: a review of its clinical applications. Magn Reson Med Sci 8:165-174.
How to cite this article:Jang SH, Lee J, Yeo SS (2017) Central post-stroke pain due to injury of the spinothalamic tract in patients with cerebral infarction: a diffusion tensor tractography imaging study. Neural Regen Res 12(12):2021-2024.
Funding: This work was supported by the National Research Foundation (NRF) of Korea Grant funded by the Korean Government (MSIP),No. NRF-2015R1D1A1A01060314.
*Correspondence to:Sang Seok Yeo, Ph.D.,eangbul@hanmail.net.
orcid:0000-0003-3873-9516(Sang Seok Yeo)
10.4103/1673-5374.221159
2017-04-10
Copyedited by Li CH, Song LP, Zhao M
杂志排行
中国神经再生研究(英文版)的其它文章
- Roles of neural stem cells in the repair of peripheral nerve injury
- Advanced diffusion-weighted magnetic resonance imaging in the evaluation of white matter axons in patients with idiopathic normal pressure hydrocephalus
- The contribution of oligodendrocytes and oligodendrocyte progenitor cells to central nervous system repair in multiple sclerosis: perspectives for remyelination therapeutic strategies
- MicroRNAs in Parkinson’s disease and emerging therapeutic targets
- Surgical reconstruction of spinal cord circuit provides functional return in humans
- Environmental cues determine the fate of astrocytes after spinal cord injury
