WIC评分预测心肺复苏后自主循环恢复患者预后的价值
2017-11-16徐伟干姜骏符岳罗银秋霍健杨黄祖华
徐伟干,姜骏,符岳,罗银秋,霍健杨,黄祖华
(佛山市第一人民医院,广东佛山528000)
WIC评分预测心肺复苏后自主循环恢复患者预后的价值
徐伟干,姜骏,符岳,罗银秋,霍健杨,黄祖华
(佛山市第一人民医院,广东佛山528000)
目的探讨查尔森合并症指数(WIC)评分预测心肺复苏后自主循环恢复患者预后的价值。方法选择实施心肺复苏后自主循环恢复的成年心脏骤停患者182例,入院72 h死亡139例(死亡组)、存活43例(存活组)。收集两组临床资料,包括一般资料(性别、年龄)、基础疾病(心肌梗死、充血性心力衰竭、周围血管疾病、脑血管意外、痴呆、慢性肺部疾病、结缔组织病、溃疡病、轻度肝损害、糖尿病、偏瘫、中重度肾脏疾病、糖尿病伴器官损害、肿瘤、中重度肝脏疾病)、并发症[脓毒症、多器官功能衰竭(MODS)]以及WIC评分、急性生理与慢性健康状况评分Ⅱ(APACHE Ⅱ评分)。采用单因素和多因素Logistic回归分析分析患者预后的影响因素。绘制受试者工作特征(ROC)曲线,评估WIC评分预测患者预后的效能。结果单因素分析显示,年龄、并发症(脓毒症、MODS)、WIC评分、APACHE Ⅱ评分可能与患者预后有关(P均<0.05),性别、基础疾病与患者预后无关(P均>0.05)。多因素Logistic回归分析显示,年龄(OR=1.050,95%CI:1.008~1.094)、WIC评分(OR=1.544,95%CI:1.058~2.254)、APACHE Ⅱ评分(OR=1.471,95%CI:1.204~1.796)、合并MODS(OR=3.207,95%CI:1.321~7.789)是患者预后的独立影响因素(P均<0.05)。ROC曲线分析显示,WIC评分、APACHE Ⅱ评分及二者联合对患者预后预测概率的曲线下面积分别为0.723(95%CI:0.648~0.817)、0.806(95%CI:0.727~0.885)、0.822(95%CI:0.749~0.895);二者联合和单独APACHE Ⅱ评分预测患者预后的ROC曲线下面积明显大于单独WIC评分(Z分别为2.659、2.125,P均<0.05),但二者联合与单独APACHE Ⅱ评分预测患者预后的ROC曲线下面积比较P>0.05。结论WIC评分可用于预测心肺复苏后自主循环恢复患者预后,联合APACHE Ⅱ评分效果更佳。
心肺复苏;自主循环恢复;查尔森合并症指数评分;急性生理与慢性健康状况Ⅱ评分;预后
目前,心肺复苏后自主循环恢复患者病死率仍较高[1,2]。急性生理与慢性健康状况评分Ⅱ(APACHE Ⅱ评分 )是心肺复苏后自主循环恢复患者病情程度和预后评估的常用指标[3],但需根据患者入院24 h内各项指标的最差值综合计算,项目多且计算繁锁。查尔森合并症指数(WIC)评分是基于19种基础疾病的评分系统,简单实用[4],可用于评价ICU危重患者预后[5,6]。但其能否用于预测心肺复苏后自主循环恢复患者预后尚不清楚。为此,我们于2012年1月~2016年1月进行了相关研究。
1 资料与方法
1.1 临床资料 选择同期在佛山市第一人民医院实施心肺复苏后自主循环恢复的成年心脏骤停患者182例。纳入标准:①年龄≥18岁;②实施心肺复苏后自主循环恢复≥24 h;③临床资料完整。排除标准:①外伤所致心脏停搏或有心脏手术史者;②入ICU时间≤24 h者;③中途放弃治疗者。患者入院72 h死亡139例(死亡组),存活43例(存活组)。
1.2 研究方法 收集两组临床资料,包括一般资料(性别、年龄)、基础疾病(心肌梗死、充血性心力衰竭、周围血管疾病、脑血管意外、痴呆、慢性肺部疾病、结缔组织病、溃疡病、轻度肝损害、糖尿病、偏瘫、中重度肾脏疾病、糖尿病伴器官损害、肿瘤、中重度肝脏疾病)、并发症(包括脓毒症、多器官功能衰竭(MODS)]。入院24 h内,按WIC评分表计算WIC评分;根据APACHE Ⅱ评分量表,计算APACHE Ⅱ评分。

2 结果
2.1 两组临床资料比较 一般资料:死亡组男84例、女55例,年龄(67.1±12.2)岁;存活组男30例、女13例,年龄(59.1±9.03)岁;两组性别比例比较P>0.05,年龄比较P<0.05。基础疾病:死亡组心肌梗死23例、充血性心力衰竭31例、周围血管疾病4例、脑血管意外46例、痴呆5例、慢性肺部疾病63例、结缔组织病7例、溃疡病8例、轻度肝损害25例、糖尿病29例、偏瘫8例、中重度肾脏疾病32例、糖尿病伴器官损害5例、肿瘤14例、中重度肝脏疾病11例,存活组分别为5、7、2、11、2、18、4、4、10、13、4、5、3、3、5例,两组比较P>0.05。并发症:死亡组并发脓毒症42例、MODS 87例,存活组分别6、12例,两组比较P均<0.05。死亡组及存活组WIC评分分别为(2.81±1.4)、(1.72±1.0)分,APACHE Ⅱ评分分别为(20.06±2.6)、(17.05±2.4)分,两组比较P均<0.05。
2.2 心肺复苏后自主循环恢复患者预后的影响因素分析 以心肺复苏后自主循环恢复患者预后作为因变量,单因素分析筛选出有统计学意义的变量作为自变量,进行多因素Logistic回归分析。结果显示,年龄、APACHE Ⅱ评分、WIC评分、合并MODS是心肺复苏后自主循环恢复患者预后的独立影响因素(P均<0.05)。见表1。
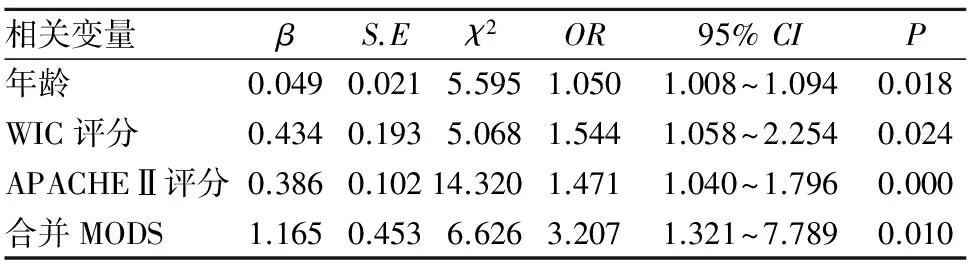
表1 心肺复苏后自主循环恢复患者预后的 多因素Logistic回归分析
2.3 WIC评分预测心肺复苏后自主循环恢复患者预后的效能 ROC曲线分析显示,WIC评分、APACHE Ⅱ评分及二者联合预测心肺复苏后自主循环恢复患者72 h存活概率的曲线下面积分别为0.723(95%CI:0.648~0.817)、0.806(95%CI:0.727~0.885)、0.822(95%CI:0.749~0.895)。二者联合或单独APACHE Ⅱ评分预测患者预后的ROC曲线下面积明显大于单独WIC评分(Z分别为2.659、2.125,P均<0.05),但二者联合与单独APACHE Ⅱ评分预测患者预后的ROC曲线下面积比较P>0.05。见插页Ⅰ图2。
3 讨论
国外研究发现,尽管部分心搏骤停患者行心肺复苏后可恢复自主循环,但昏迷者存活率仅30.4%[7]。随着患者年龄增大,其存活率逐渐降低,甚至降至4%[8]。目前,评价危重患者病情程度、预测死亡概率主要通过APACHE Ⅱ评分、简化急性生理评分等[9,10]。这些评分系统不能充分评估患者基础疾病状态,继而影响预测患者预后的准确性。
WIC评分是一种快速评价患者基础疾病严重程度的评分系统,可用于评价患者生存率及预后。目前已证实,WIC评分可判断许多疾病的不良预后,如恶性种瘤、冠心病、脑卒中等[11,12]。心脏骤停患者常存在高血压、冠心病、糖尿病等多种基础疾病,WIC评分可对其基础疾病进行量化评分,可能有助于评估患者预后。有报道显示,心脏骤停患者心肺复苏自主循环恢复后出现MODS可能是患者早期死亡的重要原因之一[13]。心脏骤停患者心肺复苏自主循环恢复后,机体处于多器官功能紊乱状态,多数患者死亡发生在自主循环恢复24 h内[14]。本研究结果显示,心肺复苏后自主循环恢复患者预后与患者年龄、是否并发MODS有关。因此,决定患者预后的因素,不仅是疾病本身,医疗干预也是重要因素。本研究单因素分析显示,年龄、并发症(脓毒症、MODS)、WIC评分、APACHE Ⅱ评分可能与患者预后有关;而性别、基础疾病与患者预后无关。多因素Logistic回归分析显示,年龄、WIC评分、APACHE Ⅱ评分、合并MODS是患者预后的独立影响因素。ROC曲线分析显示,APACHE Ⅱ评分及WIC评分联合APACHE Ⅱ评分预测患者预后的价值高于WIC评分,与Innocenti等[15]报道一致。但WIC评分所需数据易获得,且计算简便,因而其应用价值更大。
综上所述,WIC评分应用便捷,易于在临床开展,在心肺复苏后自主循环恢复患者临床情况难以判断以及实难室数据不完善时,WIC评分的优势比较明显。
[1] Kohler M, Thomas A, Geyer H, et al. Cardiopulmonary resuscitation in the elderly: analysis of the events in the emergency department[J]. Emerg Care J, 2013,9(1):18- 19.
[2] Chan PS, Krumholz HM, Spertus JA, et al. Automated external defibrillators and survival after in- hospital cardiac arrest[J]. JAMA, 2011,304(19):2129- 2136.
[3] Sathianathan K, Tiruvoipati R, Vij S. Prognostic factors associated with hospital survival in comatose survivors of cardiac arrest[J]. World J Crit Care Med, 2016,5(1):103- 106.
[4] SØholm H, Hassager C, Lippert F, et al. Factors associated with successful resuscitation after out- of- hospital cardiac arrest and temporal trends in survival and comorbidity[J]. Ann Emerg Med, 2015,65(5):523- 531.
[5] Cui Y, Wang T, Bao J, et al. Comparison of charlson′s weighted index of comorbidities with the chronic health score for the prediction of mortality in septic patients[J]. Chin Med J (Engl), 2014,127(14):2623- 2627.
[6] Song SE, Lee SH, Jo EJ, et al. The Prognostic value of the charlson′s comorbidity index in patients with prolonged acute mechanical ventilation: a single center experience[J]. Tuberc Respir Dis (Seoul), 2016,79(4):289- 294.
[7] Mallikethi- Reddy S, Briasoulis A, Akintoye E, et al. Incidence and survival after in- hospital cardiopulmonary resuscitation in nonelderly adults: US experience, 2007 to 2012[J]. Circ Cardiovasc Qual Outcomes, 2017,10(2):e003194.
[8] van de Glind EM, van Munster BC, van de Wetering FT, et al. Pre- arrest predictors of survival after resuscitation from out- of- hospital cardiac arrest in the elderly a systematic review[J]. BMC Geriatr, 2013(13):68.
[9] Aminiahidashti H, Bozorgi F, Montazer SH, et al. Comparison of APACHE Ⅱ and SAPS Ⅱ scoring systems in prediction of critically Ⅲ patients′ outcome[J]. Emerg (Tehran), 2017,5(1):e4.
[10] Godinjak A, Iglica A, Rama A, et al. Predictive value of SAPS Ⅱ and APACHE Ⅱ scoring systems for patient outcome in a medical intensive care unit[J]. Acta Med Acad, 2016,45(2):97- 103.
[11] Radovanovic D, Seifert B, Urban P, et al. Validity of charlson comorbidity index in patients hospitalised with acute coronary syndrome. Insights from the nationwide AMIS Plus registry 2002- 2012[J]. Heart, 2014,100(4):288- 294.
[12] Jimenez Caballero PE, Lopez Espuela F, Portilla Cuenca JC, et al. Charlson comorbidity index in ischemic stroke and intracerebral hemorrhage as predictor of mortality and functional outcome after 6 months[J]. J Stroke Cerebrovasc Dis, 2013,22(7):e214- e218.
[13] 李南,张东,王育珊,等.心肺复苏后多器官功能障碍综合征的临床分析[J].中华急诊医学杂志,2010,19(7):680- 683.
[14] Xue JK, Leng QY, Gao YZ, et al. Factors influencing outcomes after cardiopulmonary resuscitation in emergency department[J]. World J Emerg Med, 2013,4(3):183- 189.
[15] Innocenti F, Tozzi C, Donnini C, et al. SOFA score in septic patients: incremental prognostic value over age, comorbidities, and parameters of sepsis severity[J]. Inter Emerg Med, 2017(10):1- 8.
PredictivevalueofWICinprognosisofpatientswithrestorationofspontaneouscirculationaftercardiopulmonaryresuscitation
XUWeigan,JIANGJun,FUYue,LUOYinqiu,HUOJianyang,HUANGZuhua
(TheFirstPeople′sHospitalofFoshan,Foshan528000,China)
ObjectiveTo explore the predictive value of Charlson′s weighted index of comorbidities (WIC) in predicting the prognosis of patients with restoration of spontaneous circulation (ROSC) after cardiopulmonary resuscitation (CPR).MethodsA retrospective review was performed for the patients with ROSC after CPR. In 182 enrolled patients, 139 patients died and 43 patients survived. The clinical data were recorded including general information (gender, age), original diseases (myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular accident, dementia, chronic lung diseases, connective tissue disease, ulcers, mild liver damage, diabetes, hemiplegia, moderately severe kidney disease, diabetes accompanied with organ damage, tumors, and moderately severe liver diseases, etc.), complications [sepsis and multiple organ failure (MODS)] and WIC score, acute physiology and chronic health evaluation Ⅱ (APACHE Ⅱ) score. The logistic regression was used and the receiver operating characteristic curve (ROC curve) was drawn to calculate the prognosis of ROSC patients.ResultsUnivariate analysis showed that age, complications (sepsis and MODS), WIC score and APACHE Ⅱ score were independently associated with the prognosis of patients with CRP after ROSC (allP<0.05); gender and original diseases had nothing to do with the prognosis of ROSC patients (allP>0.05). Multivariate logistic regression analysis showed that age (OR=1.050, 95%CI:1.008- 1.094), WIC score (OR=0.544, 95%CI:1.058- 2.254), APACHE Ⅱ score (OR=1.471, 95%CI:1.204- 1.796) and having MODS or not (OR=3.207, 95%CI:1.321- 7.789) were independently associated with the prognosis of ROSC patients (allP<0.05). ROC curve areas of WIC score, APACHE II score and the combination of the two in predicting the prognosis of patients were 0.723 (95%CI:0.648- 0.817), 0.806 (95%CI:0.727- 0.885), 0.822 (95%CI:0.749- 0.895). The predictive value of the combination of the two and APACHE II score were greater than that of WIC score in predicting prognosis (Z=2.659, 2.125, allP<0.05). But there was no significant difference between the combination of the two and APACHE Ⅱ score (P>0.05).ConclusionWCI score can be used for predicting the prognosis of patients with ROSC after CPR, which is more convenient and easy to carry out.
cardiopulmonary resuscitation; return of spontaneous circulation; Charlson′s weighted index of comorbidities; Acute physiology and chronic health Ⅱ score; prognosis
佛山市科技创新项目(2016AG100511)。
徐伟干(1985- ),男,主治医师,主要研究方向为心肺脑复苏、中毒及急危重症。E- mail: 113101993@qq.com
姜骏(1972- ),男,副主任医师,主要研究方向为脑复苏后病理生理变化及其机制。E- mail: jiangjungd@163.com
10.3969/j.issn.1002- 266X.2017.36.007
R654.1
A
1002- 266X(2017)36- 0025- 03
2017- 03- 08)
