Socioeconomic, environmental, and geographic factors and US lung cancer mortality, 1999–2009
2017-11-07MariaMejiadeGrubbBarbaraKilbourneKatyKilbourneMichaelLangstonLisaGittnerRogerZoorobRobertLevine
Maria C. Mejia de Grubb, Barbara Kilbourne, Katy Kilbourne, Michael Langston, Lisa Gittner, Roger J. Zoorob,Robert Levine
Socioeconomic, environmental, and geographic factors and US lung cancer mortality, 1999–2009
Maria C. Mejia de Grubb1, Barbara Kilbourne2, Katy Kilbourne3, Michael Langston4, Lisa Gittner5, Roger J. Zoorob1,Robert Levine1
Background:The American Cancer Society estimates that about 25% of all US cancer deaths will be due to lung cancer — more than from cancers of the colon, breast, and prostate combined.
Methods:We ascertained county-level age-adjusted and age-specific death rates and 95%confi dence intervals from the Centers for Disease Control and Prevention Compressed Mortality File. Multiple regression analyses were used to estimate the strength and direction of relationships between county poverty, smoking, fi ne particulate matter (PM2.5) air pollution, and US Census divisions and race- and sex-specific lung cancer deaths.
Results:Poverty, smoking, and particulate matter air pollution were positively and signifi -cantly related to lung cancer deaths among white men, but of these, only poverty and smoking were significantly associated with lung cancer deaths among white women. Residence in the South Atlantic, East South Central, and West South Central US Census divisions at the time of death was significantly associated with lung cancer deaths for both white men and white women. As with white men, poverty and smoking were associated with lung cancer deaths among black men, but of these, only adult smoking had a statistically significant association among black women.
Conclusions:The results support the need for further research, particularly in high-risk areas,to better differentiate factors specific to race and sex and to understand the impact of local risk factors.
Lung cancer; mortality; geographic; risk factors; environmental; hot spot
Introduction
Lung cancer is one of the most common cancers worldwide, accounting for about 20% of all cancer deaths [1]. In the United States, the American Cancer Society estimates that there will be about 222,500 new cases of lung cancer (116,990 among men and 105,510 among women) in 2017; it also notes that about 25% of all US cancer deaths will be due to lung cancer — more than from cancers of the colon, breast, and prostate combined [2].Among men, lung cancer incidence in the United States is highest among blacks, with white men ranking second; among US women,whites rank fi rst and blacks second [3]. The risk factors for lung cancer include personal and second-hand smoking, outdoor air pollution, radon exposure, and workplace exposures such as exposure to asbestos, arsenic, beryllium, cadmium, diesel engine exhaust, nickel,some forms of silica, and chromium [4—7].
Geographic variations may provide useful insights into high-risk areas and may generate hypotheses about possible risk factors [8]. Within the state of Kentucky, geospatial analysis suggested that coal mining might be a risk factor associated with increased risk, particularly in the eastern part of the state [9]. High rates of lung cancer have also been noted in northern Florida, possibly due to occupational exposures from paper and pulp manufacturing, shipbuilding, and/or petroleum distillation [10]. Regionally, a study of lung cancer in United States identifi ed clusters in the southeastern near Oak Ridge National Laboratory, in eastern Tennessee, for both sexes, and in counties with high concentrations of pig farms and paper mill industries for men (occupational exposure) and in the vicinity of Atlanta, Georgia for women [11]. National US studies are scarce, although changes in regional variation were noted between 1950 to 1994 [12]. Clusters began appearing among white women in the 1950s, with higher rates on the Atlantic and Pacific coasts. At that time, the rates among blacks were found to be higher in northern areas than in the south[12]. In this article, we update information on national variations in the geographic distribution of US lung cancer deaths from 1999 to 2009. We aim to explore correlations between lung cancer mortality and socioeconomic, environmental, and geographic factors at the county level in the United States.
Methods
We ascertained county-level age-adjusted and age-specific death rates and 95% confi dence intervals from the US Centers for Disease Control and Prevention Compressed Mortality File as provided on the WONDER public Internet site [13, 14].This website also provides county averages for the concentration of fi ne particulate matter (PM2.5) air pollution for 2003 to 2008 [15]. Measures of county socioeconomic characteristics were collected from the 2000 and 2010 United States Census of Population as compiled by GeoLytics (East Brunswick,New Jersey). GeoLytics bases its estimates on US Census Bureau reports and limited population estimates, then expands on those to provide multiple population-based variables [16].Additionally, county-level estimates of black residential isolation were obtained from the publicly available we site of the Arizona State University GeoDa Center [17]. Estimates of the percentage of smokers among persons aged 18 years or older were obtained from the Behavioral Risk Factors Surveillance Survey [18].
Zero-order correlations (Pearson) were used to assess the bivariate strength of the relationship between each independent variable and lung cancer deaths since relatively high correlations among many of the independent variables could mask the impact of any single variable in a multivariate regression.Analyses were performed to estimate the strength and direction of linear relationships between pairs of continuous variables, including the percentage of the county population with an annual income below the poverty level, the percentage of persons aged 18 years or older who are current smokers, the average concentration of PM2.5air pollution for 2003 to 2008,and US Census divisions, and race (black/white)- and sexspecific percentages of the county population [19]. To estimate the magnitude of the association between the aforementioned factors and race- and sex-specific, age-adjusted (25—85 years of age), and county-lung cancer deaths, we used ordinary least squares multiple regression analysis [20] after ensuring that assumptions for ordinary least squares were met. Values were transformed to natural log values for these analyses. Gedis-Ord G* analysis [21] was used to identify hot spots for lung cancer on the basis of county age-adjusted (25—85 years of age), race, sex, and ethnicity (non-Hispanic) lung cancer death rates.
Results
Table 1 presents the results for zero-order correlations between poverty, smoking, PM2.5air pollution, and US Census division and race- and sex-specific lung cancer deaths. Weak to moderate (r= 0.1 to 0.6) positive correlations were found for poverty and smoking regardless of race or sex. For PM2.5air pollution,however, statistically significant positive correlations were found among whites but not blacks. Geographic correlations were similar for white men and women, being generally negative or not significant in the northern and eastern United States and positive and statistically significant in the South Atlantic,East South Central, and West South Central US Census divisions. Dissimilarities were found between black men and black women. Correlations for the East North Central and West North Central US Census divisions were positive and statistically significant for women but not men, while correlationsfor the East South Central and West South Central US Census divisions were positive and statistically significant for men,and the correlation for the West South Central US Census division was less strong for women and not statistically significant for the East South Central US Census division.

Table 1. Zero-order correlations between lung cancer deaths (non-Hispanic, 25—85 and older years) and county characteristics, United States,1999—2009
Table 2 shows the results for multiple regression analyses.Poverty, smoking, and PM2.5air pollution were positively and significantly related to lung cancer deaths among white men,but of these, only poverty and smoking were significantly associated with lung cancer deaths among white women.Additionally, residence in the South Atlantic, East South Central, and West South Central US Census divisions at the time of death was significantly associated with lung cancer deaths for both white men and women. As with white men,poverty and smoking were associated with lung cancer deaths among black men, but of these, only adult smoking had a statistically significant association among black women. Finally,while residence in the East South Central and West South Central US Census divisions was positively associated with lung cancer deaths among black men, residence in these areas was significantly and negatively associated with lung cancer deaths among black women.
Figures 1 to 4 present hot spot analyses of county-level lung cancer deaths for white men (Fig. 1), white women (Fig. 2),black men (Fig. 3), and black women (Fig. 4). As ref l ected in the multiple regression analyses, the geographic hot spots are similar for both white men and white women, with both showing the highest occurrence in the South Atlantic, East South Central, and West South Central US Census divisions — especially Kentucky, Tennessee, West Virginia, and Virginia. An additional hot spot for men is centered in Georgia, with lesser extension to northern Florida and southern Alabama. White women also show moderate clustering in this area, but the hottest areas are located in northern Florida. Black men and black women present contrasting geographic patterns. For black men, the hottest spots are found along the Mississippi River basin, from the junction of Missouri, Kentucky, Tennessee,and Mississippi in the north parts of Louisiana and Arkansas(with extension to parts of Oklahoma and Texas) in the south.In contrast, these are relatively cool areas for black women,whose hottest spots are scattered throughout Ohio, Indiana,Illinois, Kentucky, and Missouri.
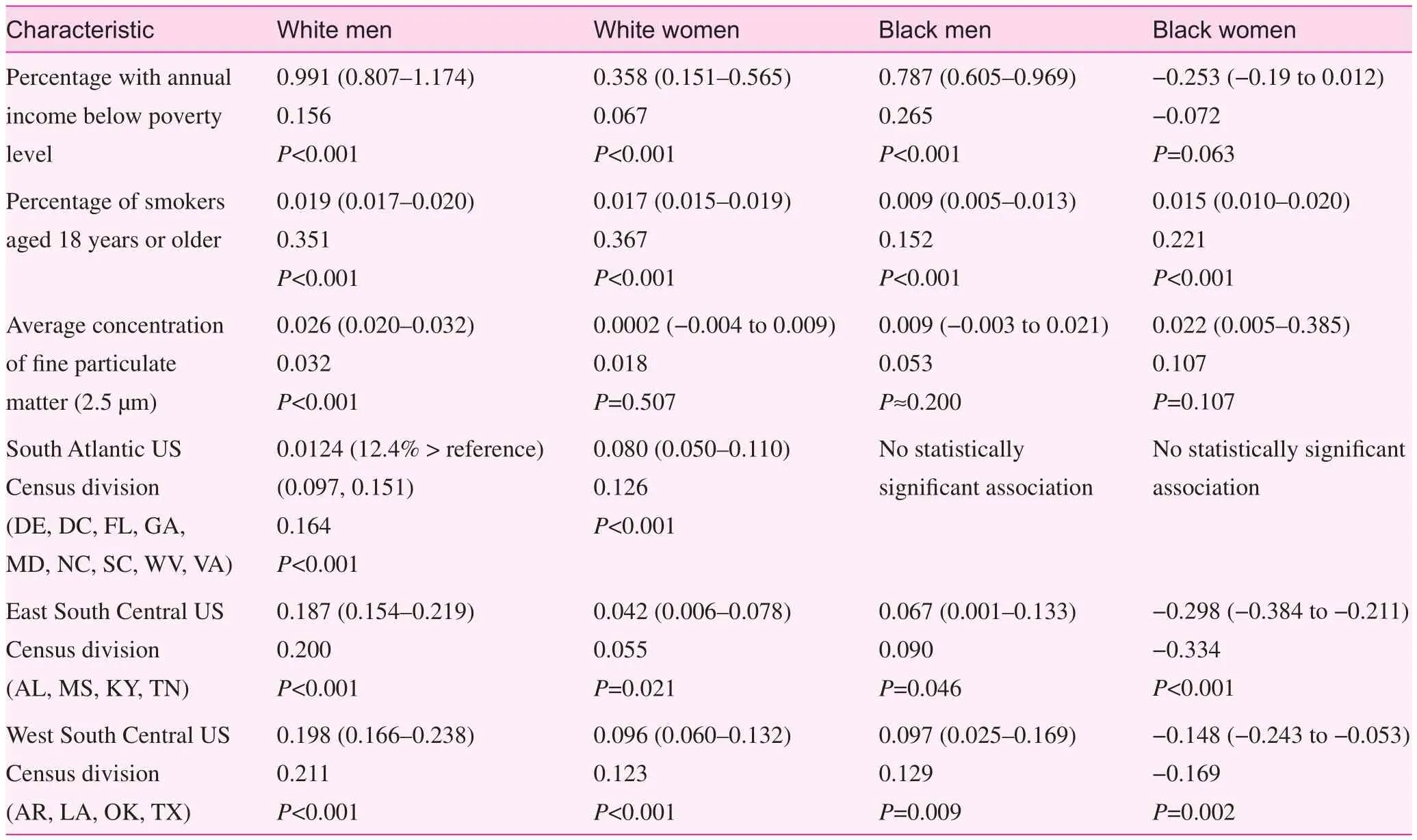
Table 2. Lung cancer deaths (natural log transformations): metric coefficients, 95% confi dence limits, standardized regression coefficients, and P-values
Discussion
This study confi rms the importance of such factors as poverty, smoking, and outdoor air pollution as important independent risk factors for lung cancer, although the patterns were not identical for each race or sex group. The data also show marked geographic variations in lung cancer death within the United States, some of which are detectable even after poverty, smoking, and outdoor air pollution have been accounted for. The geographic patterns were similar for white men and women, but different for black men and women. The high frequency of lung cancer death among black men along the Mississippi River and westward coupled with relatively low mortality among black women in the same area is consistent with the hypothesis that occupational exposures affecting men but not women may be key; an analytic epidemiologic study would be required to test this hypothesis.
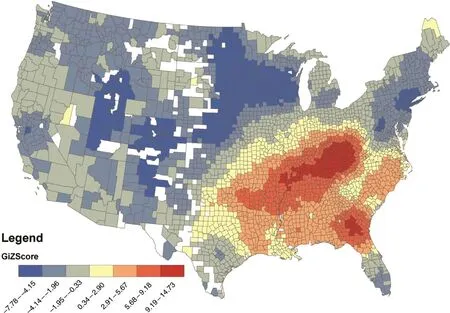
Fig. 1. Hot spot analysis of age-adjusted deaths form malignant neoplasm of the trachea, bronchus and lung among non-Hispanic white men ages 25 to 85+ years. USA. 1999—2009
The association between socioeconomic vulnerability and lung cancer has been documented in previous studies encompassing both the United States and other nations [8,22—30]. As in the present study, which shows positive correlations with the percentage of people living in poverty, those with lower socioeconomic status have been repeatedly found to be at high risk of lung cancer. In the United States, black patients have been found to constitute a significant portion of low-income patients with lung cancer, to have received a diagnosis at an earlier age, and to present with more advanced disease. Blacks are more susceptible to smoking-induced lung cancer and have less access to health care services compared with whites, both of which might contribute to the higher lung cancer incidence in the black population [31]. In addition, data show that even when lung cancer is diagnosed early,blacks are less likely than whites to have the option of surgical resection, the gold standard treatment, even after socioeconomic factors have been accounted for [32, 33]. However,in an equal-access health care system (the US military health system), where routine access to cancer care is comparable for blacks and whites, both groups were found to have similar risks of survival [34].
Smoking has long been identifi ed as a cause of lung cancer and many other illnesses [35]. Smoking may explain some of the observed geographic variation in these data; at least 28.6% of cancer deaths in the United States (in 2014)are attributable to cigarette smoking [35]. Specifically, the incidence of lung cancer has been found to be higher in tobacco-producing states such as Kentucky, where smoking is more common, and lower in states such as Utah, a nontobacco-producing state, where smoking is not permitted for observant Mormons, the predominant religious group [36].In the present data, associations with smoking prevalence are also stronger among whites and men. In men, approximately 40% of cancer deaths in the top-ranked states (Arkansas,Louisiana, Tennessee, West Virginia, and Kentucky, which are all southern tobacco-producing states) were explained by smoking. Conversely, smoking explains a quarter (>26%)of all cancer deaths in women (three southern states —Kentucky, Arkansas, and Tennessee — and two Western states— Alaska and Nevada) [37]. In part, this may reflect corresponding relationships between race, sex, and smoking in the US population [36].
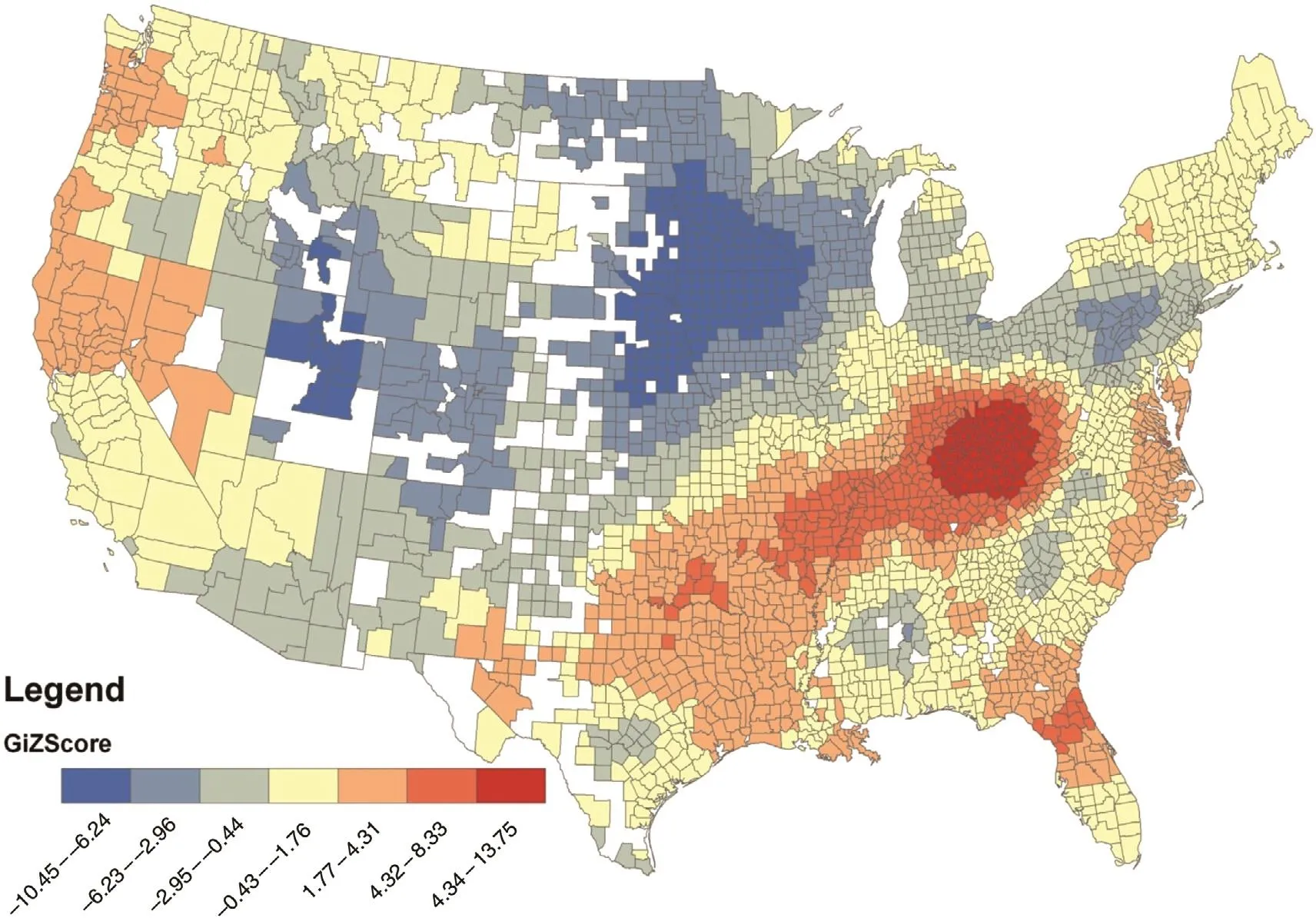
Fig. 2. Hot spot analysis of age-adjusted deaths form malignant neoplasm of the trachea, bronchus and lung among non-Hispanic white women ages 25 to 85+ years. USA. 1999—2009
After poverty, smoking, and geographic location have been accounted for, outdoor air pollution is associated with lung cancer death only among white men in the data. While outdoor air pollution has been associated with lung cancer death [38,39], race- and sex-specific data are sparse among US populations. An extended follow-up of the Harvard Six Cities Study found a statistically significant 37% increase in lung cancer death for each 10-µg/m3increase in PM2.5concentration [38].While these studies did not provide race- and sex-specific results, a descriptive study of nitrogen oxide emissions found that incidence rates of adenocarcinoma of the lung in black males was about 50% higher than that in white males and that this could be explained by differences in air quality related to site and size [39]. On the other hand, a study of fi ne particulate air pollution in relation to carotid artery intima-media thickness found that fi ne particulate matter air pollution was not related to intima-media thickness differences in blacks and Hispanics compared with whites [40]. Further research is important, in part, because of biologic plausibility. The lungs are the organs subject to the most direct effects of particulate air pollution. Fine particles may carry potentially carcinogenic toxic chemicals and can reach the lung alveoli, where clearance is slow. There they can induce sustained pulmonary and systemic inf l ammation [34].
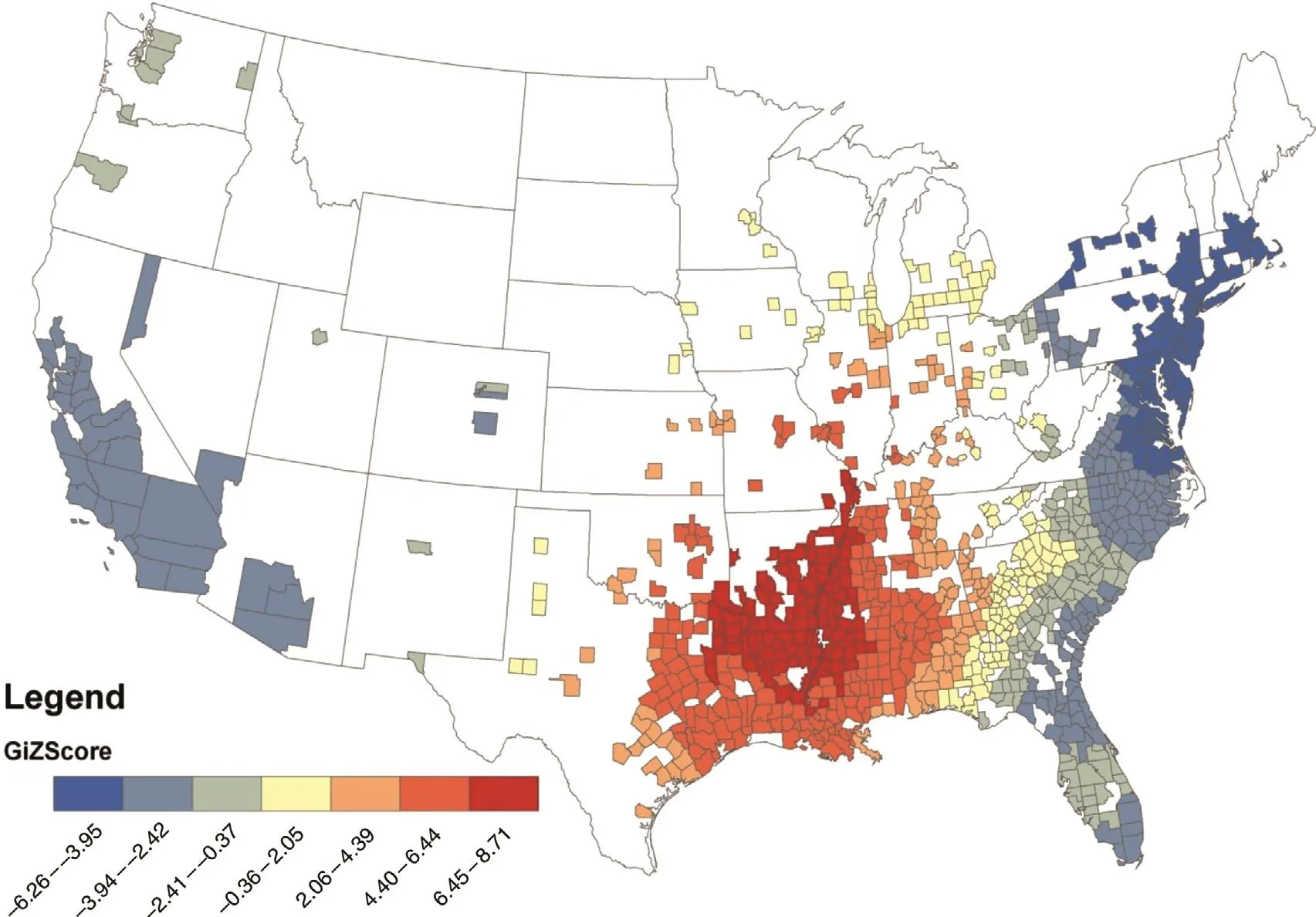
Fig. 3. Hot spot analysis of age-adjusted deaths form malignant neoplasm of the trachea, bronchus and lung among non-Hispanic black and African American men ages 25 to 85+ years. USA. 1999—2009
In addition to air pollution, the present data show statistically significant associations between lung cancer death and specific geographic areas, even after poverty, smoking, and PM2.5air pollution have been accounted for. The location of hot spots for black men but not black women extending along the Mississippi River and westward (Figs. 3 and 4) is similar to a pattern observed in Belgium for men living in subdistricts with a particular occupational exposure (i.e., mining) [8]. In these subdistricts, the incidence of lung cancer was significantly higher among men but not women. Since the hot spots along the Mississippi River and westward are highly agricultural, it is tempting to speculate that airborne pesticides or other potentially toxic agents used in agriculture may be responsible. Clear links between agricultural chemical exposure and lung cancer are difficult to establish because of the low number ofindividuals with lung cancer cases exposed to some pesticides, the changing agricultural chemical landscape, and the potential lags of 10—15 years between exposure and cancer development[41]. An analytic epidemiologic study with individual exposure information on occupational exposures in areas of high mortality would be needed to test such hypotheses.
Other geographic hot spots in these data confi rm previous observations ofincreased lung cancer deaths in the Appalachian region of the United States (which incorporates portions of the South Atlantic and East South Central US Census divisions, both of which were significantly associated with lung cancer deaths in these data). Mining operations in Appalachia create an unhealthy and stressful environment because of all the associated industries that create increased noise, diesel fuel emissions and particulates, dust, odors and truck traffic, and road congestion, which has previously been associated with increased cancer risk [42]. The present data also confi rm previous observations of lung cancer clustering in central Georgia [11] (although the present results are positive for men as well as women) and northern Florida [10]. By locating high-risk areas, both the present results and the results of previous studies help to locate places where an analytic epidemiologic investigation might be most effective for development of a better understanding of how factors such as race and sex may interact and what public health policies might be most effective in reducing risk.
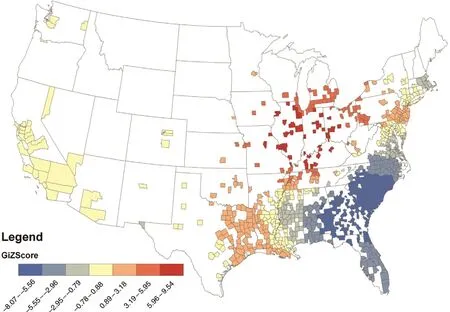
Fig. 4. Hot spot analysis of age-adjusted deaths form malignant neoplasm of the trachea, bronchus and lung among non-Hispanic black and African American women ages 25 to 85+ years. USA. 1999—2009
This study was based on death certificates and is both descriptive and, at least in part, ecological. Both the source of the data and the study design place limitations on the way the results may be interpreted. The limitations of death certificates are well known [43]. Nonetheless, death certificates may be generally more valid for cases in which cancers are listed as the underlying cause of death, and death certificates have been specifically found to be valid for cases of lung cancer [44]. Descriptive data are suitable for the generation but not the testing pf hypotheses, so any hypotheses generated by these descriptive data would require an analytic epidemiologic investigation designed a priori to do so. Contextual poverty and smoking information in these data are ecological and not specifically linked to cases of lung cancer death. The results suggest an independent effect for lung cancer in the countylevel context; however, because of privacy rules; the analysis lacks individual level socioeconomic data, which could have had at the very least independent or confounded impacts on lung cancer death. Confi dence in the validity of the present observations, however, is supported by their corroboration by the aforementioned studies based on individual information.Finally, there are limitations as to the types of data that are available. We used a broad age range for mapping in these data so as to maximize the number of counties with sufficient numbers of lung cancer deaths that had reliable data. This, however, meant that we could not focus on older age groups even though lung cancer death rates are highest among the elderly.Additionally, we did not have race-specific data pertaining to smoking prevalence.
In summary, the present data show statistically significant relationships between death from lung cancer and exposure to poverty, smoking, fi ne particulate matter, and place of residence at the time of death. They support the need for further research, particularly in high-risk areas, to better differentiate factors specific to race and sex and understand the impact of local risk factors.
Conflict ofinterest
The authors declare no conflict ofinterest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profi t sectors.
1. Cancer Research UK. Worldwide cancer statistics. 2016.[accessed 2016 Oct 18]. Available from: www.cancerresearchuk.org/health-professional/cancer-statistics/worldwidecancer#heading-Zero.
2. American Cancer Society. Cancer Facts & Figures. 2017.[accessed 2017 Apr 7]. Available from: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2017/cancer-facts-and-figures-2017.pdf.
3. US Centers for Disease Control and Prevention. Lung cancer rates by race and ethnicity. 2016. [accessed 2016 Oct 18]. Available from: www.cdc.gov/cancer/lung/statistics/race.htm.
4. US Centers for Disease Control and Prevention. What are the risk factors for lung cancer? 2016. [accessed 2016 Oct 18]. Available from: www.cdc.gov/cancer/lung/basic_info/risk_factors.htm.
5. Hamra GB, Guha N, Cohen A, Laden F, Raaschou-Nielsen O,Samet JM, et al. Outdoor particulate matter exposure and lung cancer: a systematic review and meta-analysis. Environ Health Perspect 2014;122(9):906—11.
6. Brown T, Darnton A, Fortunato L, Rushton L. Occupational cancer in Britain. Respiratory cancer sites: larynx, lung and mesothelioma. Br J Cancer 2012;107:S56—70.
7. Ahrens W, Merletti F. A standard tool for the analysis of occupational lung cancer in epidemiologic studies. Int J Occup Environ Health 1998;4:236—40.
8. Hagedoorn P, Vandenheede H, Willaert D, Vanthomme K,Gadeyne S. Regional inequalities in lung cancer mortality in belgium at the beginning of the 21st century: the contribution ofindividual and area-level socioeconomic status and industrial exposure. PLoS One 2016;11(1):e0147099.
9. Christian WJ, Huang B, Rinehart J, Hopenhayn C. Exploring geographic variation in lung cancer incidence in Kentucky using a spatial scan statistic: elevated risk in the Appalachian coal-mining region. Public Health Rep 2011;126(6):789—96.
10. Hennekens CH, Davies JE, Levine RS, Briese FW, Nordwall CW. Trends of lung cancer in northern Florida. South Med J 1981;74(5):566—8.
11. Goovaerts P. Geostatistical analysis of county-level lung cancer mortality rates in the southeastern United States. Geogr Anal 2010;42(1):32—52.
12. Devesa SS, Grauman DJ, Blot WJ, Fraumeni JF Jr. Cancer surveillance series: changing geographic patterns of lung cancer mortality in the United States, 1950 through 1994. J Natl Cancer Inst 1999;91(12):1040—50.
13. Centers for Disease Control and Prevention, National Center for Health Statistics. [Internet] Compressed mortality fi le 1999-2014 on CDC WONDER Online Database, released December 2015. Data are from the compressed mortality fi le 1999—2014 series 20 no. 2T, 2015, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. [accessed 2016 Oct 18]. Available from:http://wonder.cdc.gov/cmf-icd10.html.
14. Centers for Disease Control and Prevention, National Center for Health Statistics. [Internet] Compressed mortality fi le 1979—1998. CDC WONDER On-line Database, compiled from compressed mortality fi le CMF 1968—1988, series 20, no. 2A, 2000 and CMF 1989—1998, series 20, no. 2E, 2003. [accessed 2016 Oct 18]. Available from: http://wonder.cdc.gov/cmf-icd9.html.
15. Centers for Disease Control and Prevention. Daily Fine Particulate Matter (PM2.5) (µg/m³) Request for years 2003—2008 on CDC WONDER Online Database. [accessed 2016 Oct 18].Available from: http://wonder.cdc.gov/NASA-PM.html.
16. Geraghty EM, Balsbaugh T, Nuovo J, Tandon S. Using geographic information systems (GIS) to assess outcome disparities in patients with type 2 diabetes and hyperlipidemia. J Am Board Fam Med 2010;23(1):88—96.
17. Anselin L, Syabri I, Kho Y. GeoDa: an introduction to spatial data analysis. Geograph Anal 2006;38(1):5—22.
18. Health Indicators Warehouse. [Internet] Cigarette smoking adults: percent [Source: BRFSS]. National Center for Health Statistics. 2016. [accessed 2016 Oct 18]. Available from: www.healthindicators. gov/Indicators/Cigarette-smoking-adults-percent-Source-BRFSS_13/Profi le.
19. US Census Bureau. [Internet] Census regions and divisions of the United States. [accessed 2016 Oct 18]. Available from: https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf.
20. Rosner B. Fundamentals of biostatistics. 7th ed. Boston, MA:Cengage Learning; 2010.
21. ARC GIS. [Internet] Hot Spot Analysis (Getis-Ord Gi*) (Spatial Statistics) v. 9.3. [accessed 2016 Oct 30]. Available from: http://webhelp.esri.com/arcgisdesktop/9.3/index.cfm?TopicName=Hot_Spot_Analysis_(Getis-Ord_Gi*)_(Spatial_Statistics).
22. Van Loon AJ, Goldbohm RA, van den Brandt PA. Lung cancer:is there an association with socioeconomic status in the Netherlands? J Epidemiol Commun Health 1995;49:65—9.
23. Steenland K, Henley J, Calle E, Thun M. Individual- and area-level socioeconomic status variables as predictors of mortality in a cohort of 179,383 persons. Am J Epidemiol 2004;159:1047—56.
24. Bentley R, Kavanagh AM, Subramanian SV, Turrell G. Area disadvantage, individual socio-economic position, and premature cancer mortality in Australia 1998 to 2000: a multilevel analysis.Cancer Causes Control 2008;19:183—93.
25. Van der Heyden JH, Schaap MM, Kunst AE, Esnaola S, Borrell C,Cox B, et al. Socioeconomic inequalities in lung cancer mortality in 16 European populations. Lung Cancer 2009;63:322—30.
26. LaPar DJ, BhamidipaticM, Harris DA, Kozower BD, Jones DR,Kron IL, et al. Gender, race, and socioeconomic status affects outcomes after lung cancer resections in the United States. Ann Thorac Surg 2011;92(2):434—9.
27. Yang R, Cheung MC, Byrne MM, Huang Y, Nguyen D, Lally BE,et al. Do racial or socioeconomic disparities exist in lung cancer treatment? Cancer 2010;116(10):2437—47.
28. Hystad P, Carpiano RM, Demers PA, Johnson KC, Brauer M.Neighbourhood socioeconomic status and individual lung cancer risk: Evaluating long-term exposure measures and mediating mechanisms. Soc Sci Med 2013;97:95—103.
29. Hastert TA, Beresford SA, Sheppard L, White E. Disparities in cancer incidence and mortality by area-level socioeconomic status: a multilevel analysis. J Epidemiol Commun Health 2014;69:168—76.
30. Sharpe KH, McMahon AD, Raab GM, Brewster DH, Conway DI. Association between socioeconomic factors and cancer risk:a population cohort study in Scotland (1991—2006). PLoS One 2014;9:e89513.
31. Fairley TL, Tai E, Townsend JS, Stewart SL, Steele CB,Davis SP, et al. Racial/ethnic disparities and geographic differences in lung cancer incidence — 38 states and the District of Columbia, 1998—2006. MMWR Morb Mortal Wkly Rep 2010;59(44):1434—8.
32. Steele CB, Pisu M, Richardson LC. Urban/rural patterns in receipt of treatment for non-small cell lung cancer among black and white Medicare beneficiaries, 2000—2003. J Natl Med Assoc 2011;103:711—8.
33. Hardy D, Liu CC, Xia R, Cormier JN, Chan W, White A, et al.Racial disparities and treatment trends in a large cohort of elderly black and white patients with nonsmall cell lung cancer. Cancer 2009;115:2199—211.
34. Ganti AK, Subbiah SP, Kessinger A, Gonsalves WI, Silberstein PT, Loberiza FR Jr. Association between race and survival of patients with non-small-cell lung cancer in the United States veterans affairs population. Clin Lung Cancer 2014;15:152—8.
35. US Department of Health and Human Services. The health consequences of smoking — 50 years of progress: a report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention,National Center for Chronic Disease Prevention and Health Promotion, Office of Smoking and Health; 2014.
36. Slegel RL, Miller KD, Jemal A. Cancer Statistics. 2016. CA Cancer J Clin 2016;66(1):7—30.
37. Lortet-Tieulent J, Sauer AG, Siegel RL, Miller KD, Islami F,Fedewa SA, et al. State-level cancer mortality attributable to cigarette smoking in the United States. J Am Med Assoc Intern Med 2016;176(12):1792—8.
38. Lepeule J, Laden F, Dockery D, Schwartz J. Chronic exposure to fi ne particles and mortality: an extended follow-up of the Harvard Six Cities study from 1974 to 2009. Environ Health Perspect 2012;120(7):965—70.
39. Chen F, Cole P, Bina WF. Time trend and geographic patterns of lung adenocarcinoma in the United States, 1973—2002. Cancer Epidemiol Biomark Prev 2007;16(12):2724—9.
40. Jones MR, Diez-Roux AV, O’Neill MS, Guallar E, Sharrett AR, Post W, et al. Ambient air pollution and racial/ethnic differences in carotid intima-media thickness in the multi-ethnic study of atherosclerosis (MESA). J Epidemiol Commun Health 2015;69(12):1191—8.
41. Bonner MR, Freeman LE, Hoppin JA, Koutros S, Sandler DP,Lynch CF, et al. Occupational exposure to pesticides and the incidence of lung cancer in the agricultural health study. Environ Health Perspect 2017;125(4):544—51.
42. Crosby L, Tatu C, Charles K. Lung and bronchus cancer deaths in Boone County, WV before and after mountaintop removal mining. J Rare Dis Diagn Ther 2016;2:1—8.
43. Hennekens CH, Buring JE, Mayrent SL, editors. Epidemiology in medicine. 1st ed. Philadelphia, PA: Lippincott, Williams &Wilkins; 1987.
44. Doria-Rose VP, Marcus PM. Death certificates provide an adequate source of cause of death information when evaluating lung cancer mortality: an example from the Mayo Lung Project. Lung Cancer 2009;63(2):295—300.
1. Department of Family and Community Medicine, Baylor College of Medicine, Houston,TX, USA
2. Sociology Department,Tennessee State University,Nashville, TN, USA
3. Department of Family and Community Medicine, Meharry Medical College, Nashville, TN,USA
4. Department of Electrical Engineering and Computer Science, University of Tennessee, Knoxville, TN, USA 5. Department of Political Science, Texas Tech University College of Arts and Sciences,Lubbock, TX, USA
Maria C. Mejia de Grubb, MD,MPH
Department of Family and Community Medicine, Baylor College of Medicine, 3701 Kirby Drive, Houston, TX 77030-3411, USA
E-mail: maria.mejiadegrubb@bcm.edu
10 January 2017;Accepted 2 March 2017
杂志排行
Family Medicine and Community Health的其它文章
- The global burden of preventable cancer mortality
- Smoking, depression, and hospital costs of respiratory cancers:Examining race and sex variation
- Self-reported preferences for patient and provider roles in cancer treatment decision-making in the United States
- Student self-assessment versus preceptor assessment at the midpoint of a family medicine clerkshipa
- Characteristics of patients with erectile dysfunction in a family physician-led erectile dysfunction clinic: Retrospective case series
- Ten year risk assessment ofischemic cardiovascular disease and intervention analysis among middle-aged residents with moderate risk and above in a Shanghai-based community
