干骺端LCP前侧微创与外侧切开治疗肱骨中下段骨折的临床疗效分析
2017-11-06周金华戴峰刘杰郑志良袁霆
周金华 戴峰 刘杰 郑志良 袁霆
干骺端LCP前侧微创与外侧切开治疗肱骨中下段骨折的临床疗效分析
周金华1戴峰1刘杰1郑志良1袁霆2
目的探讨干骺端锁定加压钢板(locking compression plates,LCP)前侧微创与外侧切开治疗肱骨中下段骨折的临床疗效。方法回顾性分析溧阳市人民医院2009年1月至2015年1月收治的肱骨中下段骨折患者30例,其中男17例,女13例,年龄22~80岁,平均51.2岁。分别采用干骺端LCP前侧微创经肱肌中外1/3入路(A组)和外侧经肱桡肌与肱肌间隙解剖桡神经入路(B组)治疗,两组各15例。记录手术时间、术中失血量、术后平均住院时间、平均骨折愈合时间、医源性桡神经麻痹发生率、切口感染的发生率、Mayo肘关节功能评分及臂、肩、手功能障碍功能评分。结果所有患者术后均获随访,随访时间为12~18个月,平均15.3个月。两组患者在术后平均骨折愈合时间、术后切口感染的发生率上差异无统计学意义(P>0.05)。A组手术时间、术中失血量、医源性桡神经麻痹发生率、平均住院时间低于B组(P <0.05);A组Mayo肘关节功能评分及臂、肩、手功能障碍功能评分优于B组(P <0.05)。结论采用干骺端LCP前侧微创治疗肱骨中下段骨折临床疗效优于外侧切开。
锁定加压钢板; 肱骨中下段; 微创
肱骨中下段骨折的治疗方法较多,效果也各不相同。保守治疗骨折愈合率高,但易畸形愈合,且因外固定时间长而导致关节功能障碍,传统外侧切开手术需解剖桡神经,手术时间较长、出血多、二期取内固定可能更易损伤桡神经。近年来,微创钢板内固定术因具有创伤小、骨折愈合率高的优点,在临床上应用逐步增多。本院2009年1月至2015年1月共收治的肱骨中下段骨折患者30例,分别采用干骺端锁定加压钢板(locking compression plates,LCP)前侧微创经肱肌中外1/3入路和外侧经肱桡肌与肱肌间隙解剖桡神经入路治疗,治疗结果报道如下。
资料与方法
一、一般资料
按手术入路的不同将所有患者分为A组(1~15号)、B组(16~30号),两组各15例。A组:男8例,女7例;年龄22~78岁,平均年龄55.5岁;骨折AO骨折分型:A型8例,B型4例,C型3例。B组:男9例,女6例;年龄27~80岁,平均年龄58.5岁;骨折AO骨折分型:A型7例,B型4例,C型4例。所有患者均为闭合型骨折,且术前均无桡神经损伤症状。
二、手术方法
(一)术前准备
常规行各项术前检查,先行排除及治疗内科疾病;检查有无桡神经损伤症状,有症状者行肌电图检查,肌电图显示有神经损伤者排除在本研究外。
(二)影像学观察
所有患者术前均拍肱骨正侧位片,行CT及三维重建检查,以求明确骨折类型。
(三)手术方法
1. A组:颈丛加臂丛麻醉下,沙滩位,上臂外展90°,前臂旋后位,置可透视手术桌上。首先在骨折端处前外侧作3 cm辅助小切口,将肱二头肌牵向内侧并显露肱肌,沿肱肌中外1/3纵向钝性劈开,暴露骨折端,骨膜下剥离,手法复位后克氏针或拉力螺钉固定;然后于上臂近端前方,三角肌与肱二头肌交界处作3 cm的纵向切口,骨膜下剥离并连通骨折端切口;最后于肘横纹近端前侧作约3 cm切口,较骨折端辅助切口偏内侧,纵向钝性劈开肱二头肌肌腹及肱肌,插入骨膜剥离器,向近端行骨膜下剥离,直至骨折端切口。从上向下插入尽量长的干骺端LCP。在此过程中,助手协助屈肘,以放松前臂屈肌便于操作。于钢板两端的钉孔各打入1枚2.0克氏针,临时固定。透视机确认钢板远端位于冠状窝上缘,钢板与肱骨干长轴一致,骨折断端无分离和短缩。在钢板两端(肱骨中1/3以外)各打入3~4枚锁定螺钉。
2. B组:颈丛加臂丛麻醉下,沙滩位,常规消毒铺单,取肱骨中下段外侧切口,约12 cm,逐层切开皮肤、皮下筋膜,从肱二头肌和肱三头肌间隙进入暴露骨折端,从肱肌和肱桡肌间隙中暴露桡神经,见桡神经无明显挫伤,牵开予以保护,牵引复位肱骨,清除骨折端软组织及血凝块,复位,置入肱骨干锁定钢板,远、近端各3~4枚锁定钉固定。
三、术后处理
术后24 h内应用抗生素,术后48 h拔除引流管,术后2周拆线。术后患肢颈腕带保护,术后第1天即嘱患者进行肩关节和肘关节的主动活动。术后 1、2、3、6、9、12、18个月复诊,拍摄肱骨正侧位片,见图1,2。
四、评价指标
记录手术时间、术中失血量、术后平均住院时间、平均骨折愈合时间、医源性桡神经麻痹发生率、切口感染的发生率、Mayo肘关节功能评分及臂、肩、手功能障碍(disabilites of the arm,shoulder and hand,DASH)功能评分。
五、统计学分析
采用SPSS 22.0统计软件进行统计学分析。计量资料以 x-±s表示,组间比较采用两独立样本均数t检验,P <0.05认为差异有统计学意义。
结 果
所有患者术后均获随访,随访时间为12~18个月,平均(15.3±1.3)个月。术后平均骨折愈合时间A组患者为(13.7±0.7)周,B组为(14.0±0.7)周,两者差异无统计学意义(P>0.05)。两组患者术后均无手术切口感染发生。平均手术时间A组为100.5 min,B组为129.3 min,两者差异有统计学意义(P <0.05)。平均术中失血量A 组为(96.3±9.7)ml,B 组为(238.7±60.2)ml,两者差异有统计学意义(P <0.05)。B组术后出现2例桡神经麻痹症状,经保守治疗后4个月左右恢复,考虑术中牵拉所致。平均住院时间A 组 为(7.3±1.0)d,B组 为(13.5±1.2)d, 两者差异有统计学意义(P <0.05)。末次随访平均Mayo肘关节功能评分A组为(95.0±1.4)分,B组为(81.2±4.8)分,两者差异有统计学意义(P <0.05)。平均DASH上肢功能评分A组为(12.1±1.1)分,B组为(24.3±1.9)分,两者差异有统计学意义(P <0.05)。患者基本资料见表1。
讨 论
一、肱骨中下段骨折治疗方法
肱骨干骨折约占全身骨折的1%,是一种常见的上肢创伤。肱骨周围解剖结构复杂,其近段前侧有肌皮神经,内侧有正中神经、尺神经、肱动脉和肱静脉通过,中1/3段后侧有桡神经通过,行走于肱骨干下1/3外侧。肱骨干本身形态也较复杂,中段以上为圆形且较粗,至下1/3段逐渐变成扁三角形,并稍向前倾,故肱骨干中下段骨折在临床上较常见[1]。肱骨干中下段骨折目前的治疗方法尚无定论。非手术治疗愈合率较高,但易发生畸形愈合,且因长时间制动而导致肩、肘关节功能障碍[2-3]。髓内钉固定对于肱骨干中下段骨折没有优势[4],顺行髓内钉的工作距离太长,骨折线距离远端锁钉太近,稳定性差;逆行髓内钉易造成医源性肱骨髁上骨折[5]。外固定支架也是一种方法,但容易并发钉道感染、松动,影响生活和肘关节的功能[6]。切开复位钢板固定是目前治疗肱骨干中下段骨折最主要的方法,其优点在于骨折可获解剖复位,肩、肘关节功能影响较小,缺点在于软组织剥离较多,易发生医源性桡神经损伤,同时切开复位导致骨折断端血供受损加重,骨不连发生率增高。近年来微创技术的发展,闭合复位内固定术的兴起,避免了解剖桡神经,缩短了手术时间。
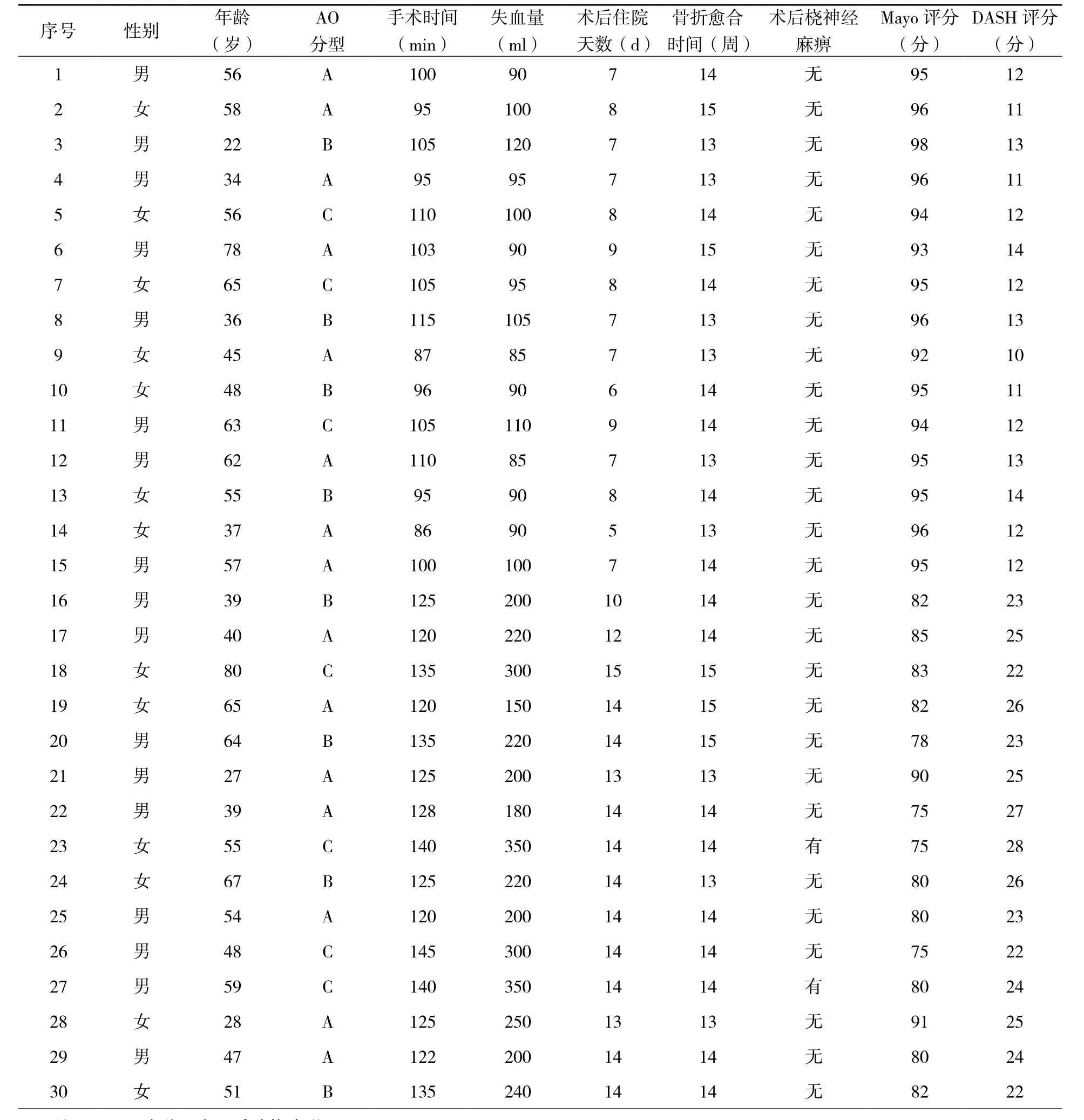
表1 所有患者基本资料
二、外侧切开解剖桡神经治疗肱骨中下段骨折
通常认为外侧切开复位钢板内固定是最可靠的治疗方法[7-8],但存在创伤大,骨不连发生率高的缺点[9-10]。外侧入路切开复位者,需要游离桡神经,并用橡皮条轻轻加以保护,以免术中将其误切。骨折复位固定后,要将桡神经置于健康组织内,切忌将桡神经直接置于钢板或骨质的表面,避免损伤组织形成瘢痕压迫桡神经,或者钢板及骨质对桡神经形成硬性压迫。本研究B组15例患者术前均无桡神经损伤,术后有2例患者出现一过性桡神经麻痹症状,考虑术中牵拉损伤所致,2例患者术后3个月内均恢复正常。术中对桡神经的解剖及内固定置入后的妥善处理至关重要,二期取内固定时因组织粘连更应谨慎。

图1 患者男性,36岁,跌伤致右肱骨中下段骨折,术前拍正侧位X线片(A,B)示B1型骨折;采用干骺端LCP微创前侧治疗(C),术后3 d(D、E)、6个月(F、G)复查正侧位X线;术后12个月取内固定时功能位照片(H),术后患者对治疗效果满意
三、干骺端LCP微创前侧治疗肱骨中下段骨折
肱骨干前侧骨面平整,表面覆盖肱肌和肱二头肌,没有重要的血管和神经通过,适合钢板内固定的放置。但如果前方行传统的切开复位,需要全程切开前方覆盖的肱肌,创伤较大[11]。针对于此,仅切开肱肌的两端、在其下方插入钢板固定的微创方法,被一些学者开始应用。安智全等[12]解剖学研究证明前侧钢板固定肱骨中下段的骨折时,钢板绝大部分被肱肌肌腹覆盖,钢板与桡神经在穿过外侧肌间隔的部位与钢板之间的距离>1.0 cm。在距离最近的冠状窝上缘水平,钢板外侧缘和桡神经之间的距离也>5.0 mm。因此在上臂前侧经皮、肌下的微创插入钢板固定肱骨中下段的骨折不会影响桡神经功能,本研究A组15例患者术后无一例出现桡神经损伤,也表明干骺端LCP微创前侧治疗肱骨中下段骨折是安全的。与安智全等介绍的全程微创不暴露骨折端的操作不同的是,本研究加用了骨折端前外侧小切口辅助复位。因为,作者发现在全程微创操作过程中,如果不暴露骨折端,通过间接复位的方法往往难以有效纠正骨折端的错位。通过辅助小切口,可以直视下复位骨折端,获得解剖或近似解剖的复位,节省手术时间。此外,采用骨折端小切口辅助复位的微创方式,对于某些螺旋型骨折(复位时可能将桡神经夹在骨折端),较全程微创有着明显优势,可以直视下确保骨折端中无软组组,减少了术中损伤桡神经的可能。国外学者提出桡神经肱肌支存在率为81.6%,其中从肱肌外侧面下面进入肱肌的为83%,从肱肌中1/3处进入的为17%[13]。陈琳等[14]对国人桡神经肱肌支研究后发现,桡神经肱肌支存在率达51.4%。故为了保存肱肌的屈肌功能,作辅助小切口时向内侧牵开肱二头肌肌腹,肱肌中外1/3纵形钝性劈开。作远端小切口时同样钝性分离无法内侧牵拉的肱二头肌和下方的肱肌,同时尽量偏内侧,避免损伤前臂外侧皮神经。
综上所述,认为采用干骺端LCP微创前侧治疗肱骨中下段骨折是一种安全、有效的方法,可以减轻手术创伤、缩短住院天数、降低医源性桡神经损伤以及更好的关节功能恢复。

图2 患者男性,27岁,跌伤致左肱骨中段骨折,术前拍正位X线片(A)示A1型骨折;采用外侧入路解剖桡神经内固定治疗,术后3 d(B、C)、6个月(D、E)复查正侧位X线片;术后12个月功能位照片(F),术后患者对治疗效果满意
[1]Eldaolm R, Adami J, Tidermark J, et al. Fractures of the shaft of the humerus. An epidemiological study of 401 fractures[J]. J Bone Joint Surg Br, 2006, 88(11): 1469-1473.
[2]Koch PP, Gross DF, Gerber C. The results of functional(Sarmiento) bracing of humeral shaft fractures[J]. J Shoulder Elbow Surg, 2002, 11(2): 143-150.
[3]Pehlivan 0. Functional treatment of the distal third humeral shaftfractures[J]. Arch Orthop Trauma Surg, 2002, 122(7):390-395.
[4]Blyth MJ, Macleod CM, Asante DK, et al. Iatrogenic nerve injury with the Russell-Taylor humeral nail[J]. Injury, 2003,34(3): 227-228.
[5]Lin J, Shen PW, Hou SM. Complications of locked nailing in humeral shaft fractures[J]. J Trauma, 2003, 54(5):943-949.
[6]Li ZZ, Hou SX, Wu KJ,et al. Unilateral external fixator in the treatment of lower third humeral shaft fractures [J]. Chin J Traumatol, 2005, 8(4): 230-235.
[7]Niall DM, O'Mahony J, McElwain JP. Plating of humeral shaft Fractures-has the pendulum swung back?[J]. Injury, 2004,35(6):580-586.
[8]Bhandari M, Devereaux PJ, Mckee MD, et al. Compression plating versus intramedullary nailing of humeral shaft fractures-a meta-analysis[J]. Acta Orthop, 2006, 77(2):279-284.
[9]Meekers FS, Broos PL. Operative treatment ofhumeral shaft fractures. The Leuven experience[J]. Acta Orthop Belg,2002, 68(5): 462-470.
[10]Levy JC, Kalandiak SP, Hutson JJ, et al. An alternative method of osteosynthesis for distal humeral shaft fractures[J]. J Orthop Trauma, 2005, 19(1): 43-47.
[11]谢小平, 叶蜀新, 林海, 等. 钢板前置固定治疗肱骨中下段骨折[J]. 中国修复重建外科杂志, 2005, 19(3): 195-197.
[12]安智全, 曾炳芳, 王烨明, 等. 用MIPO技术治疗肱骨干下段骨折的解剖及初步临床报告[J]. 中华手外科杂志,2006, 22(6): 336-338.
[13]Mahakkanukrauh P, Somsarp V. Dual innervation of the brachialis muscle[J]. Clin Anat, 2002, 15(3): 206-209.
[14]陈琳, 尹望平. 桡神经肱肌支的解剖学研究[J]. 中国临床解剖学杂志, 1999, (1): 27-28.
Yuan Ting, Email: terrenceyuan@gmail.com
Clinical efficacy analysis of minimally invasive plate osteosynthesis via anterior approach versus conventional fixation technique via lateral approach in the treatment of middle-inferior fracture of humeral shaft
Zhou Jinhua1, Dai Feng1, Liu Jie1, Zheng Zhiliang1, Yuan Ting2.1Department of Orthopaedics,Liyang People's Hospital, Liyang 213300, China;2Department of Orthopaedics, The 6th Affiliated People's Hospital of Shanghai Jiaotong University,Shanghai 200233,China
BackgroundThe treatment for the middle-inferior fracture of humeral shaft is numerous, and the effect is variant. Conservative treatment has high rate of fracture healing. Because of malunion and long duration of external fixation, however, this type of treatment leads to joint dysfunction easily. Traditional lateral incision requires the anatomy of radial nerve, long operation time and more bleeding. Furthermore, the removal of internal fixator during the secondary procedure may cause radical nerve injury more easily. In recent years, minimally invasive plate osteosynthesis(MIPO) has been widely used on clinic due to its advantages of small trauma and high rate of bone healing. From January 2009 to January 2015, 30 patients with middle-inferior humeral shaft fractures were treated respectively with locking compression plates (LCP) in minimally invasive anterior approach (via the medial and lateral 1/3 of brachialis) and lateral approach (via the intermuscular space between radial muscle and brachial muscle for radial nerve anatomy) in our hospital. This study provides a retrospective analysis of treatment result.MethodsI. General Information.All patients had closed fractures, and none of them showed symptoms of radial nerve injury. According to the difference between surgical approaches, the patients were divided into group A (No. 1-15) and group B (No. 16-30). The fracture patterns were classified based on AO classification. Group A: 8 males and 7 females; age range: 22-78 years with an average of 55.5 years; AO classification: 8 cases of type A, 4 cases of type B and 3 cases of type C. Group B: 9 males and 6 females; age range: 27-80 years with an average of 58.5 years; AO classification: 7 cases of type A, 4 cases of type B and 4 cases of type C. II. Operative methods. (1)Preoperative preparation: Preoperative examinations were performed routinely to exclude and treat internal disease firstly. The symptoms of radial nerve injury were checked, and EMG examination was performed on the symptomatic patients. The patients with nerve injury showed by the EMG were excluded from this study.(2)Imaging observation: To define the type of fracture, all patients were carried out with the X-ray films of humeral shaft in anteroposterior and lateral views and the CT scan with 3 dimensional reconstruction preoperatively.(3)Operative methods: Group A: Under cervical plexus and brachial plexus blocks, the patient was in beach chair position with the affected upper arm abducted in 90° and the forearm supinated on the operation table. Firstly, a 3 cm small assisted incision was made at the anterolateral side of fracture end, and the biceps was retracted medially to expose brachial muscle. The brachial muscle was bluntly and longitudinally split along the mediolateral 1/3 part to expose fracture end. After subperiosteal dissection and manual reduction, the fracture was temporarily fixed with Kirschner wire or lag screw;then, a 3 cm longitudinal incision was made at the juncture of deltoid and biceps, which was anterior to the proximal end of upper arm. The subperiosteum was dissected to connect the incision of fracture end; finally, an incision of approximately 3 cm was made before the proximal end of cubital crease,which was medial to the assisted incision of fracture end. The biceps and brachialis were split bluntly and longitudinally to insert periosteum detacher, and the subperiosteum was dissected proximally till the incision of fracture end. The metaphysis LCP of the largest possible length was inserted from the top down. During this process, the assistant assisted elbow flexion to relax the forearm flexors for easy operation. The nail holes on both ends of plate were inserted with a 2.0 kirschner wire respectively for temporary fixation. With the confirmation under fluoroscopy, the distal end of plate was located at the upper margin of coronary fossa, and the plate was in accordance with the long axis of humeral shaft without the separation and shortening of fracture end. Both ends of the plate (apart from the 1/3 of humerus) were inserted with 3-4 locking screws respectively.Group B: Under cervical plexus and brachial plexus blocks, the patient was in beach chair position with conventional disinfection and draping. An incision of approximately 12 cm was made at the middle - lower segment of lateral humerus, and the skin and subcutaneous fascia were cut layer by layer. The fracture end was exposed via the gap between biceps and triceps, and the radial nerve was exposed through the gap between brachialis and brachioradialis. Being confirmed with no obvious damage, the radial nerve was retracted for protection. After the soft tissue and blood clots at fracture end were debrided, the humerus was reduced by traction. The locking plate of humeral shaft was inserted, which was fixed with 3-4 locking screws on the distal and proximal ends respectively. III. Postoperative treatment:Antibiotic was applied within 24 hours after operation. After surgery, the drainage tube and stich were removed 48 hours and 2 weeks later respectively. The affected limb was in neck-wrist sling for protection after operation, and active movements of shoulder and elbow joints were performed on the 1st postoperative day. Further consultation was carried out in the 1st, 2nd, 3rd, 6th, 12th and 18th postoperative months, and the X-ray films of humeral shaft were taken in anteroposterior and lateral views every time.IV. Evaluation index:The operation time, intraoperative blood loss, postoperative hospitalization time, mean time of fracture healing, incidence of iatrogenic radial nerve palsy, incidence of incision infection, Mayo elbow function score and DASH score of upper limb function were recorded.V. Statistical analysis:The SPSS 22.0 statistical software was used for statistical analysis. The measurement data were expressed asx-±s , and the t tests of two independent sample means were used for comparison between groups.P<0.05 was considered as statistical difference.ResultsAll patients were followed up for 12-18 months with an average of (15.3±1.3) months. The mean healing times for patients in group A and group B were (13.7±0.7) weeks and (14±0.7) weeks respectively, and there was no significant statistical difference between the two groups (P>0.05). No incision infection occurred in both the groups after operation. The mean operation times for group A and group B were 100.5 min and 129.3 min respectively, and there was significant statistical difference between the two groups (P<0.05). The average intraoperative blood losses for group A and group B were (96.3±9.7) ml and (238.7±60.2)ml respectively, and there was significant statistical difference between the two groups (P<0.05). Due to the intraoperative nerve traction, 2 cases of radial nerve paralysis occurred after operation in group B and recovered after approximately 4 months of conservative treatment. The average hospitalization durations for group A and group B were (7.3±1.0) days and (13.5±1.2) days respectively, and there was significant statistical difference between the two groups (P<0.05). During the last follow up, the average Mayo elbow function scores for group A and group B were (95.0±1.4) points and (81.2±4.8)points respectively, and there was significant statistical difference between the two groups (P<0.05).The average DASH upper limb function scores for group A and group B were (12.1±1.1) points and(24.3±1.9) points respectively, and there was significant statistical difference between the two groups(P<0.05)ConclusionsMinimally invasive anterior approach in combined with metaphyseal LCP is a safe and effective method to treat the middle-inferior fracture of humeral shaft. This strategy reduces surgical trauma, shortens hospital stay, reduces iatrogenic radial nerve injury and facilitates better joint function recovery.
Locking compression plate; Humeral middle-inferior fracture of shaft;Minimally invasive plate osteosynthesis
10.3877/cma.j.issn.2095-5790.2017.03.006
213300 溧阳市人民医院骨科1; 200233 上海交通大学附属第六人民医院骨科2
袁霆,Email:terrenceyuan@gmail.com
2017-02-12)
(本文编辑:李静;英文编辑:陈建海、张晓萌、张立佳)
周金华,戴峰,刘杰,等. 干骺端LCP前侧微创与外侧切开治疗肱骨中下段骨折的临床疗效分析[J/CD].中华肩肘外科电子杂志,2017,5(3):186-193.
