经尿道Peel-away鞘输尿管镜与经尿道输尿管镜治疗膀胱结石的疗效比较
2017-11-04郭亮段俊锋李东杰谷杰蒲安明欧阳健张晓波
郭亮,段俊锋,李东杰,谷杰,蒲安明,欧阳健,张晓波
(1.中南大学湘雅医院 国际医疗部,湖南 长沙 410008;2.湖南省株洲市三三一医院 泌尿外科,湖南 株洲 412008)
经尿道Peel-away鞘输尿管镜与经尿道输尿管镜治疗膀胱结石的疗效比较
郭亮1,段俊锋2,李东杰1,谷杰1,蒲安明2,欧阳健2,张晓波1
(1.中南大学湘雅医院 国际医疗部,湖南 长沙 410008;2.湖南省株洲市三三一医院 泌尿外科,湖南 株洲 412008)
目的 比较经尿道Peel-away鞘输尿管镜与经尿道输尿管镜治疗膀胱结石的效果。方法 将该科2013年1月-2015年12月76例膀胱结石按随机原则分为:A组(经尿道Peel-away鞘输尿管镜膀胱碎石术)45例;B组(经尿道输尿管镜膀胱碎石术)31例。结果 76例膀胱结石均获一次性碎石取石成功。碎石时间:A 组(17.8±5.9)min,B 组(22.7±8.3)min,差异有统计学意义(t =2.96,P =0.004);清石时间:A 组(12.6±4.9)min,B 组(24.5±5.3)min,差异有统计学意义(t =9.90,P =0.000);术中尿道黏膜损伤:A组(1.0±0.5)分,B 组(2.1±0.4)分,差异有统计学意义(t =9.47,P =0.000);VAS评分:A组(1.9±0.6)分,B组(2.6±0.6)分,差异有统计学意义(t =4.72,P =0.000);留置导尿管时间:A组(1.0±0.2)d,B组(1.4±0.9)d,差异有统计学意义(t =2.59,P =0.012);住院费用:A组(7 437.4±356.7)元,B组(7 296.8±333.8)元,差异无统计学意义(t =-1.73,P =0.087)。两组术中无膀胱大出血、穿孔和破裂等并发症,无中转开放手术。术后并发症:B组发生术后泌尿系感染1例,经口服抗生素治疗后痊愈;A组发生术后尿潴留1例,B组5例,差异有统计学意义(χ2=6.43,P =0.011)。随访情况:失访13例,余63例随访6~12个月,两组各有1例老年男性患者因前列腺增生导致尿潴留;余患者均无再发结石,无尿道狭窄。通过统计分析结果,发现A组在碎石时间、清石时间、尿道黏膜损伤、术后疼痛和术后留置导尿管时间等方面较B组具有明显优势。结论 经尿道Peel-away鞘输尿管镜与经尿道输尿管镜治疗膀胱结石疗效无明显差异。经尿道Peel-away鞘输尿管镜在碎石时间、清石时间及避免术中损伤尿道黏膜方面更优,两组手术费用无明显差异。经尿道Peel-away鞘输尿管镜是一种值得推广的内镜膀胱碎石手术方法。
膀胱结石;Peel-away鞘;经尿道;输尿管镜
治疗膀胱结石的方法主要包括内镜手术、开放性手术和体外冲击波碎石(extracorporeal shockwave lithotripsy,ESWL),内镜手术是目前治疗膀胱结石的主要方法[1-2]。经过微创外科技术的发展,越来越多的患者愿意选择微创的手术方式。经尿道Peel-away鞘输尿管镜和经尿道输尿管镜均为可行的治疗膀胱结石的术式[3]。为比较经尿道Peel-away鞘输尿管镜与经尿道输尿管镜治疗膀胱结石的效果,现将株洲市三三一医院泌尿外科(笔者原工作单位为株洲市三三一医院且数据采集于该医院,于2016年9月进入湘雅医院攻读泌尿外科硕士学位并撰写本文)2013年1月-2015年12月76例膀胱结石按手术方式分为A组(经尿道Peel-away鞘输尿管镜)和B组(经尿道输尿管镜)进行回顾性比较分析。现报道如下:
1 资料与方法
1.1 一般资料
76例术前均经B超,腹部X线(kidney ureter bladder,KUB)或CT检查确诊膀胱结石,临床表现主要为尿频、尿急、尿痛、间歇性肉眼血尿、尿流中断和排尿困难等。术前检查无全身情况不良,无严重心肺肝肾疾病。A组(经尿道Peel-away鞘输尿管镜术)45例,B组(经尿道输尿管镜术)31例,两组性别、年龄、结石长径和住院费用差异无统计学意义(P >0.05),具有可比性,见表1。病例选择标准:除外前列腺增生合并膀胱结石,需行前列腺手术及有重要器官器质性功能障碍的老年患者,排除膀胱内肿块考虑膀胱恶性肿瘤患者。符合手术适应证,有手术意愿的患者。

表1 两组患者一般资料比较Table 1 Comparisons of general data between the two groups
1.2 方法
1.2.1 A组经尿道Peel-away鞘输尿管镜膀胱碎石手术 经蛛网膜下腔阻滞或联合硬膜外麻醉后,取截石位,常规消毒铺巾,取Storz 8.0/9.8F输尿管镜行尿道、男性前列腺、膀胱镜检,了解尿道、前列腺一般情况、膀胱内结石大小数目和有无膀胱憩室等。退出输尿管镜,笔者选择Peel-away鞘(16F),适用于绝大部份患者,将鞘套入输尿管镜前端,直视下随输尿管镜进入膀胱,液压灌注泵冲洗下找到膀胱结石,输尿管镜退入鞘内,鞘前端固定结石,使用Storz气压弹道碎石机,碎石手柄接1.4 mm碎石针,顺输尿管镜操作通道进入膀胱,直视下视野中心连续击发碎石,将结石击碎至小于鞘直径,退出碎石杆,液压灌注泵开启脉冲模式,输尿管镜直视下经鞘注冲洗液入膀胱,Peelaway鞘置于膀胱最低位结石碎片附近,利用膀胱内外水压差于灌注泵脉冲工作间歇时段退出输尿管镜,随水流经鞘冲洗出结石碎片,检查膀胱内有无残留结石、出血、破裂和穿孔等。术后常规预防性使用抗生素48 h,术后1~5 d拔除导尿管。
1.2.2 B组经尿道输尿管镜膀胱碎石手术 经蛛网膜下腔阻滞或联合硬膜外麻醉后,取截石位,常规消毒铺巾,留置6.0~8.0 F小儿胃管入膀胱以引流,取Storz 8.0/9.8 F输尿管镜行尿道、男性前列腺、膀胱镜检,了解尿道、前列腺一般情况、膀胱内结石大小数目和有无膀胱憩室等。液压灌注泵冲洗下找到膀胱结石,使用Storz气压弹道碎石机,碎石手柄接1.4 mm碎石针,顺输尿管镜操作通道进入膀胱,直视下视野中心连续击发碎石,尽量将结石击碎,退镜,Elick灌洗器灌洗出结石碎片。输尿管镜再次进入膀胱检查有无残留结石、出血、破裂和穿孔等。术后常规预防性使用抗生素48 h,术后1~5 d拔除导尿管。
1.3 观察指标
①碎石时间:从气压弹道开始激发碎石至碎石结束;②清石时间:从碎石结束至清除结石碎片<2.0 mm为止;③尿道黏膜损伤:术毕退出鞘及输尿管镜时同时观察尿道黏膜损伤情况,包括无损伤0分,轻度损伤(黏膜局部擦伤)1分,中度损伤(擦伤黏膜长度>50.0 mm)2分,重度损伤(黏膜明显撕脱)3分(此为自定标准,为两个高年资医师共同观察判定损伤程度并评分);④疼痛评分:术后24 h进行疼痛评估,采用视觉模拟评估法[4](visual analog scores,VAS);⑤留置导尿管:以拔除尿管后排尿通畅、无排尿功能障碍为准;⑥住院费用:包括术前检查、麻醉、手术、药品、床位和护理等各项费用;⑦随访:6~12个月后患者有无结石再发,有无尿道狭窄。
1.4 统计学方法
采用SPSS 23.0统计学软件,计数资料采用χ2检验,正态分布的计量资料以均数±标准差(±s)表示,采用独立样本t检验,P <0.05为差异有统计学意义。
2 结果
2.1 术中情况
76例均一次性经尿道膀胱碎石成功,无中转开放,无术中大出血,无膀胱穿孔破裂。碎石时间为A组(17.8±5.9)min,B组(22.7±8.3)min,差异有统计学意义(t =2.96,P =0.004);清石时间为A组(12.6±4.9)min,B组(24.5±5.3)min,差异有统计学意义(t =9.90,P =0.000);术中尿道黏膜损伤为A组(1.0±0.5)分,B组(2.1±0.4)分,差异有统计学意义(t =9.47,P =0.000);A组碎石时间、清石时间和术中对尿道黏膜损伤均优于B组(P <0.05)。见表2。
表 2 两组术中情况比较 (±s)Table 2 Comparisons of the condition during operation between the two groups (±s)

表 2 两组术中情况比较 (±s)Table 2 Comparisons of the condition during operation between the two groups (±s)
组别 碎石时间/min 清石时间/min尿道黏膜损伤/分A组(n =45) 17.8±5.9 12.6±4.9 1.0±0.5 B 组(n =31) 22.7±8.3 24.5±5.3 2.1±0.4 t值 2.96 9.90 9.47 P值 0.004 0.000 0.000
2.2 术后情况
术后两组病例复查无残余结石。VAS评分为A组(1.9±0.6)分,B组(2.6±0.6)分,差异有统计学意义(t =4.72,P =0.000);留置导尿管时间为A组(1.0±0.2)d,B组(1.4±0.9)d,差异有统计学意义(t =2.59,P =0.012),A组VAS疼痛评分和留置导尿管时间均优于B组。术后泌尿系感染B组发生1例;术后尿潴留A组发生1例,B组5例,差异有统计学意义(P <0.05)。见表 3。
2.3 随访情况
两组患者失访13例,A组8例,B组5例,余63例随访6~12个月,两组各有1例老年男性患者因前列腺增生导致尿潴留;余患者均无再发结石,无尿道狭窄。
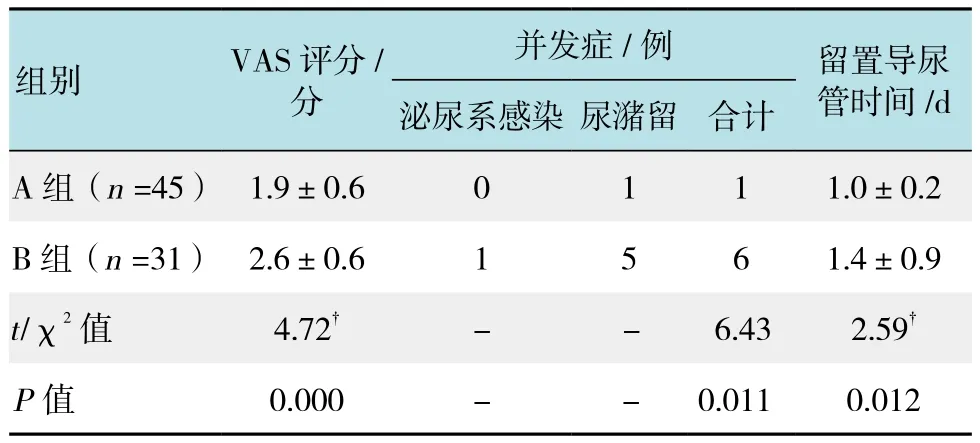
表3 两组术后情况比较Table 3 Comparisons of the postoperative situation between the two groups
3 讨论
膀胱结石治疗方法包括从化学溶解到开放手术,可以采用震波碎石术、膀胱碎石取石术,以及机械、液电、超声或激光膀胱碎石术、经皮膀胱结石取出术或开放性膀胱切开取石术等外科治疗。气压弹道碎石术是利用机械能粉碎结石,这个方法几乎总能成功粉碎结石,产生多个小碎片。对于体积大或特别坚硬的结石,气压弹道碎石比超声碎石或液电碎石效率更高[5]。目前临床上常用于内镜治疗膀胱结石的方法有经尿道钬激光碎石、经尿道气压弹道碎石和经尿道机械碎石等。激光碎石设备昂贵,在基层医院开展有一定困难;而大力钳碎石易造成膀胱及尿道损伤,对于多发或者较大结石处理受限。气压弹道碎石的工作原理是利用压缩的气体驱动碎石机手柄弹道内的子弹体,子弹体高速运动再冲击碎石杆,碎石杆撞击结石,使其碎裂,从而达到碎石的目的[6];临床中发现坚硬结石,尤其CT值大于1 200,钬激光较气压弹道碎石成功率高[7];但由于气压弹道碎石设备相对成本低,操作要求较激光碎石低,不易引起前列腺损伤及尿道狭窄,且较硬膀胱结石通常较小,在总体碎石清石过程中两种方法差异不明显,故笔者仍然选择气压弹道碎石。
两组手术均顺利完成经尿道内镜下膀胱碎石且未发生严重并发症,证实经尿道Peel-away鞘输尿管镜与经尿道输尿管镜均为可行的膀胱结石微创手术。传统经尿道输尿管镜气压弹道膀胱碎石,因膀胱充盈,结石不固定,碎石时结石跳动,不利于碎石,且为避免膀胱过度充盈,需定期排空膀胱或经尿道留置引流管,增加手术时间;碎石后需退镜后使用Elick灌洗器(22F)经尿道进入膀胱冲洗,灌洗器通道尺寸较大,无可避免损伤尿道黏膜[8];术后常规留置导尿管,笔者发现结石长径越大,术中操作时间越长,尿道黏膜损伤情况则越重,此情况B组病例中尤为明显,而发生严重尿道黏膜损伤患者,导尿管往往需留置5~7 d,延长了患者住院天数,且患者术后疼痛症状明显。使用Peel-away鞘作为通道,很好地解决了上述方面的不足:①选择Peel-away鞘(16F),适用于绝大部分患者,在进鞘方面,笔者曾尝试多种进鞘方式,如盲进、经超滑导丝引导下进、鞘套入输尿管镜摄像端待镜子进入膀胱后再旋转将鞘推入膀胱[9]、以及鞘套入输尿管镜前端,直视下随镜子一同进入膀胱[10],发现直视下鞘随镜子一同进入膀胱的进鞘方式在进入过程中,能随时调整鞘的方向及位置,最大程度地减少进鞘过程中对尿道黏膜的损伤;②碎石过程中,利用鞘将结石固定,碎石过程极少发生结石偏移,大大提高了碎石效率;③清除结石碎片过程中,整个操作过程将输尿管镜与尿道黏膜隔离,起到保护尿道黏膜作用;④同时在结石清除过程中,借鉴经皮肾碎石冲洗结石碎片原理,将液压灌注泵调至脉冲模式即可将膀胱内结石碎片冲洗干净,大大提高了清除结石效率,节省了手术时间;⑤因Peel-away鞘与输尿管镜之间有足够的空隙,避免了碎石过程中膀胱过度充盈而导致逆行感染和机体吸收导致水中毒等风险;⑥鞘的成本低廉,对此术在基层医院的推广非常有利。
综上所述,A组在术中碎石、清石时间、保护尿道黏膜及术后住院时间上的优势明显,且Peel-away鞘的成本不高,两组手术住院费用差异无统计学意义。故经尿道Peel-away鞘输尿管镜膀胱碎石术是一种值得在基层医院推广的改良内镜膀胱碎石手术方法。
[1]那彦群, 叶章群, 孙颖浩, 等. 中国泌尿外科疾病诊断治疗指南(2014版)[M]. 北京: 人民卫生出版社, 2014: 150-151.
[1]NA Y Q, YE Z Q, SUN Y H, et al. Guideline for the diagnosis and treatment of urological in China (2014 Edition)[M]. Beijing:People’s Medical Publishing House, 2014: 150-151. Chinese
[2]吴阶平. 吴阶平泌尿外科学[M]. 济南: 山东科学技术出版社,2009: 792-793.
[2]WU J P. Wujieping urolocical surgery[M]. Jinan: Shandong Science and Technology Press, 2009: 792-793. Chinese
[3]管德佳. 经尿道Peel-away鞘输尿管镜气压弹道碎石治疗膀胱结石的临床研究[J]. 中国当代医药, 2016, 23(1): 80-82.
[3]GUAN D J. Clinical study of ureteroscopic pneumatic ballistic galet via urethral Peel-away sheath on treating cystolith[J]. China Modern Medicine, 2016, 23(1): 80-82. Chinese
[4]金重睿, 撒应龙, 张炯, 等. 膀胱软镜在骨盆骨折后尿道狭窄患者中的应用及疼痛耐受性研究[J]. 中国内镜杂志, 2017, 23(1):15-19.
[4]JIN C R, SA Y L, ZHANG J, et al. Clinical application and pain tolerance of flexible cystoscopy in pelvic fracture urethral distraction defects stricture[J]. China Journal of Endoscopy, 2017,23(1): 15-19. Chinese
[5]郭应禄, 周利群, 主译. 坎贝尔-沃尔什泌尿外科学[M]. 第9版.北京:北京大学医学出版社, 2009: 2802-2803.
[5]GUO Y L, ZHOU L Q. Campbell-Walsh urological surgery[M]. 9th Edition. Beijing: Peking University Medical Press, 2009: 2802-2803. Chinese
[6]KOBTAKOLXMLOA A, STAVMPTMLM N J, PIERAMENOB D, et al. The Swiss lithoclast: an ideal intracorporeal lithotripter[J].Urol Int, 1995, 55(1): 19-20.
[7]曾鹏, 蒋重和, 李光明, 等. CT值预测经皮肾镜EMS碎石清石系统的取石效率[J]. 中国内镜杂志, 2016, 22(5): 17-20.
[7]ZENG P, JIANG C H, LI G M, et al. Clinical value of CT for predicting the stone removal rate after PCNL assisted by EMS lithoclast master[J]. China Journal of Endoscopy, 2016, 22(5): 17-20. Chinese
[8]王乐浩, 许哲, 陈锡彬, 等. 经尿道膀胱结石气压弹道碎石的技术改良:附视频[J]. 中华腔镜泌尿外科杂志: 电子版, 2014,8(4): 32-34.
[8]WANG L H, XU Z, CHEN X B, et al. Technological improvements of transurethral pneumatic lithotripsy for bladder calculi video[J].Chin J Endourol: Electronic Edition, 2014, 8(4): 32-34. Chinese
[9]范庆全. 经尿道Peel-away鞘输尿管镜气压弹道碎石治疗膀胱结石[J]. 中国医师进修杂志, 2012, 35(20): 57-59.
[9]FAN Q Q. Pneumatic ballistic lithotripsy treatment on bladder calculi via Transurethral Peel-away sheath ureteroscopy[J].Chinese Journal of Postgraduate of Medicine, 2012, 35(20): 57-59.Chinese
[10]韩聪祥, 许伟杰, 李伟, 等. 带外鞘引流腔镜下尿道会师术治疗尿道断裂(附21例报告)[J]. 中华男科学杂志, 2016, 22(7):613-616.
[10]HAN C X, XU W J, LI W, et al. Endoscopic realignment with drainage via a peel-away sheath for the treatment of urethral rupture: a report of 21 cases[J]. National Journal of Andrology,2016, 22(7): 613-616. Chinese
Ef fi cacy between ureteroscopic via urethral Peel-away sheath and transurethral ureteroscopy in treating bladder calculi:A comparative study
Liang Guo1, Jun-feng Duan2, Dong-jie Li1, Jie Gu1, An-ming Pu2, Jian Ouyang2, Xiao-bo Zhang1
(1.Department of International Medical Service, Xiangya Hospital, Central South University, Changsha,Hunan 410008, China; 2.Department of Urology, the 331st Hospital, Zhuzhou, Hunan 412008, China)
Objective To compare the effectiveness of ureteroscopic via urethral Peel-away sheath and transurethral ureteroscopy in treatment of bladder calculi. Methods Clinical data of 76 cases of bladder calculi patients were collected from January 2013 to December 2015. All the patients were randomly divided into two groups: Group A was performed by ureteroscopic lithotripsy via urethral Peel-away sheath (n = 45). Group B was transurethral ureteroscopic lithotripsy (n = 31). Results 76 cases of bladder calculi were successfully treatedby one-time lithotripsy. Lithotripsy time: group A was (17.8 ± 5.9) min, group B was (22.7 ± 8.3) min (t = 2.96,P = 0.004); stone clearance time: group A (12.6 ± 4.9) min, group B (24.5 ± 5.3) min (t = 9.90, P = 0.000);Intraoperative urethral mucosa injury : group A (1.0 ± 0.5), group B (2.1 ± 0.4) (t = 9.47, P = 0.000); VAS score:group A (1.9 ± 0.6), group B (2.6 ± 0.6) points (t = 4.72, P = 0.000); indwelling catheter time: group A (1.0 ± 0.2) d,B group (1.4 ± 0.9) d (t = 2.59, P = 0.012); There was no signi fi cant difference in hospitalization expense, group A was (7 437.4 ± 356.7), group B was (7 296.8 ± 333.8) (t = -1.73, P = 0.087). There were no complications such as hemorrhage, perforation and rupture of the 2 groups, without convertion to open surgery either. After the treatment of oral antibiotic, 1 case of postoperative urinary tract infection was cured in group B. In our study, case of postoperative urinary retention was 1 in group A, versus 5 in group B, with statistical difference (χ2= 6.43, P = 0.011). Follow up: 13 patients were lost to follow-up, the other patients were followed up for 6 ~ 12 months. There was 1 case of elderly male patient with urinary retention due to BPH in each of the 2 groups, the other patients had no recurrence of calculus. By analyzing the statistical results, it was found that the experimental group had obvious advantages over the control group in the lithotripsy time, stone clearance time, urethral mucosa injury, postoperative pain and postoperative indwelling catheter time. Conclusion There is no signi fi cant difference in ef fi cacy of the treatment of bladder calculi between ureteroscopic via urethral Peel-away sheath and transurethral ureteroscopy. However, our study shows the Peel-away ureteroscopy has the advantages of shorter lithotripsy time, shorter time of stone clearance and less injury of urethra mucosa menbrane, there was no signi fi cant difference in operation cost between two groups.Therefore, Ureteroscopic via urethral Peel-away sheath is an effective method for endoscopic bladder lithotripsy.
bladder calculi; peel-away sheath; transurethral; ureteroscope
R694.4
A
10.3969/j.issn.1007-1989.2017.10.006
1007-1989(2017)10-0026-05
2017-04-05
张晓波,E-mail:xiaobozxb@163.com;Tel:0731-89753054
(彭薇 编辑)