椎小关节空间趋向性与腰椎滑脱的相关性研究
2017-08-07葛卫卫王华斌姚杰孙萍陆文娟
葛卫卫,王华斌,姚杰,孙萍,陆文娟
(南京市中心医院南京市市级机关医院放射科,江苏南京210008)
椎小关节空间趋向性与腰椎滑脱的相关性研究
葛卫卫,王华斌,姚杰,孙萍,陆文娟
(南京市中心医院南京市市级机关医院放射科,江苏南京210008)
目的:探讨椎小关节空间趋向性与退行性腰椎滑脱(degenerative lumbar spondylolisthesis,DLS)之间的关系。方法:选择300例患者,分为:L4~5DLS组89例,L5~S1DLS组156例,无腰椎间盘突出和椎管狭窄的对照组55例3组。均采用CT扫描,测量3组L3~4、L4~5、L5~S1节段头尾侧小关节角并进行比较分析。结果:DLS组头侧的小关节角较尾侧为大(P<0.05);滑脱组头尾侧的差异较对照组更显著。各节段的小关节角,经配对t检验,DLS组和对照组比较差异均有统计学意义。结论:在退行性滑脱患者中,小关节角的增大说明了小关节由冠状位向矢状位的一种空间趋向的变化,这在小关节头侧表现得较显著,尤其是在腰椎滑脱的患者中,这为腰椎滑脱的病因预测提供了一种方法。
脊椎滑脱;椎关节突关节;空间趋向性;小关节角
腰椎小关节由源于下位椎体的上关节突和源于上位椎体的下关节突组成,也是脊柱中唯一的滑膜关节[1]。关节突关节空间趋向与退行性腰椎滑脱(degenerative lumbar spondylolisthesis,DLS)之间有一定的相关性[2]。本文即从关节突关节空间趋向性的变化与DLS的关系着手,探讨小关节空间形态变化是否为DLS的直接病因之一。
1 资料与方法
1.1 一般资料收集2013年3月至2016年3月我院300例因腰腿痛行腰椎CT检查的患者,分为3组:L4~5DLS组89例,L5~S1DLS组156例,对照组55例(无腰椎间盘突出、椎管狭窄、无滑脱者)。为使对照组腰椎小关节更接近正常自然人,选择小关节退变程度为Ⅰ~Ⅱ度的患者(依照Fujiwara等分级)。3组基本资料见表1。纳入标准为CT资料齐全的腰腿痛且无腰腿部手术史者。排除标准:肿瘤、结核、侧弯、骨折等病变。

表1 3组基本资料
1.2 仪器与方法患者均行腰椎CT扫描,采用64排CT机(Philips Ingenuity Core 128),将CT原始图像行MPR。全部患者由1名医师在CT诊断台上以窗宽1 500HU、窗位450HU按照同一方法观察及测量,分2个层面观察小关节角,一个是以平行于上位椎体的下终板层面作为检测层面,即关节突关节的头侧水平,一个是以平行于下位椎体的上终板层面作为检测层面,即关节突关节的尾侧水平,这2个角度的测量都以椎体的后缘作为参考平面。每例均测量L3~4、L4~5、L5~S1这2个节段左右侧小关节角的角度,测量方法见图1。
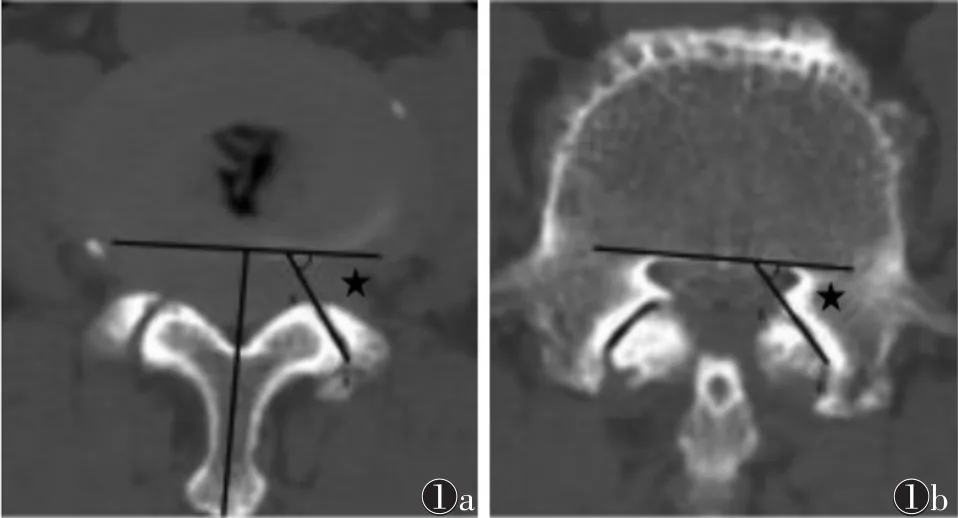
图1 男,72岁,L4~5腰椎滑脱图1a,1b分别为L4~5节段头、尾侧小关节角(★)示意图
1.3 统计学方法使用SPSS 19.0统计软件对所得数据进行统计学分析,计量资料采用±s表示。患者同一节段头尾侧小关节角,以及滑脱组与对照组小关节角之间采用配对t检验,以P<0.05为差异有统计学意义。
2 结果
2.1 组内头尾侧比较(表2)无论是L4~5节段还是L5~S1节段DLS组,其头尾侧的小关节角间的差异均有统计学意义,且头侧的小关节角均值较尾侧为大。
表2 组内头尾侧小关节角比较(°,±s)
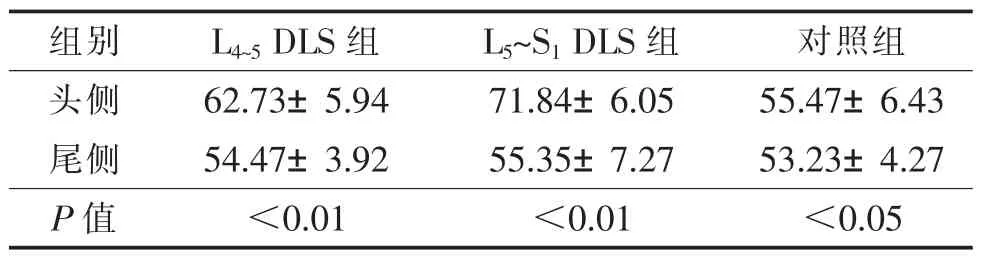
表2 组内头尾侧小关节角比较(°,±s)
组别L4~5DLS组L5~S1DLS组对照组头侧62.73±5.94 71.84±6.05 55.47±6.43尾侧54.47±3.92 55.35±7.27 53.23±4.27 P值<0.01<0.01<0.05
2.2 组间头尾侧比较(表3)DLS组和对照组各节段的头尾侧小关节角,经配对t检验,差异均有统计学意义(均P<0.01或<0.05)。
表3 DLS组与对照组组间头尾侧小关节角比较(°,±s)
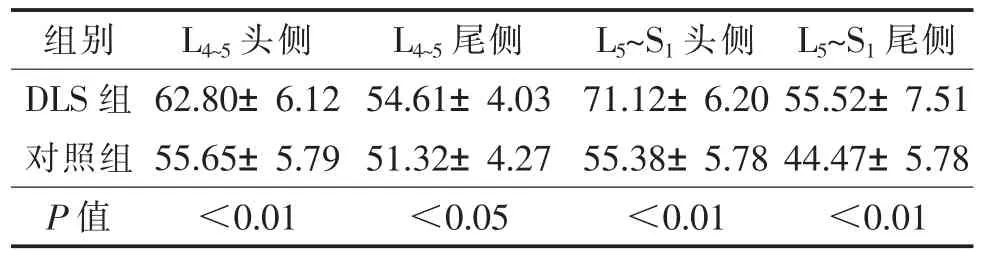
表3 DLS组与对照组组间头尾侧小关节角比较(°,±s)
组别L4~5头侧L4~5尾侧L5~S1头侧L5~S1尾侧DLS组62.80±6.12 54.61±4.03 71.12±6.20 55.52±7.51对照组55.65±5.79 51.32±4.27 55.38±5.78 44.47±5.78 P值<0.01<0.05<0.01<0.01
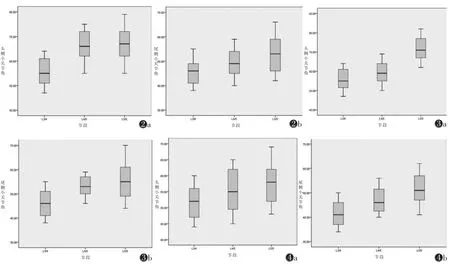
2.3 组内头尾侧小关节角各节段间比较从L3~4、L4~5至L5~S1,头尾侧小关节角均逐渐变大,头侧小关节角变大程度更显著;DLS组较对照组小关节角变大的趋势更明显(图2~4)。
3 讨论
腰椎小关节含有透明软骨、滑膜、纤维囊及1~2mL的关节间隙。上关节突的关节面多呈凹形;下关节突的关节面以凸面形和平面性为主,其次是凹面形和波浪形(S形)[3]。腰椎小关节的取向对维持腰椎稳定有重要作用,但该取向不恒定,随着生长发育过程逐渐变化。在腰椎曲线内,随着年龄增长,关节突关节基本的关节面在胎儿和婴儿时期几乎都是冠状面生长,在以后的生长发育中关节突关节的外侧缘逐渐向矢状方向生长,这种发育中的变化使关节面变成弧形,同时关节突关节的方向以矢状方向为主[4]。
腰椎滑脱层面的小关节突发应力改变,关节面由矢状面向冠状面变化,而退行性改变可促成或加重这种移行,从而导致腰椎不稳;或椎小关节的过度运动,导致小关节面磨损和反应性骨质增生,发生骨性关节炎,从而导致其限制椎体前移的限制作用减弱,又加重腰椎不稳[5]。
本研究中,从L3~4、L4~5至L5~S1,小关节角逐渐变大,L4~5滑脱组的头侧小关节角较尾侧小关节角更能反映小关节从冠状位向矢状位退变的空间趋向性变化;在L5~S1滑脱组,同样可见小关节角逐渐变大的趋势,说明小关节矢状位变化的空间趋向性,头侧小关节角更能反映这一趋势。
异常的机械应力、椎间盘变性及小关节变性被认为是引起椎体节段不稳定的主要因素[6]。腰椎的退变可引起关节突磨损和前方畸变,当达到一定程度时会出现椎体向前方滑脱[7]。因此,小关节结构与退变滑脱关系密切[8]。本研究认为,小关节椎弓根角是反映小关节形态结构的重要测量指标。小关节椎弓根角的意义在于随着角度增大,小关节间隙随之趋于水平位,不利于小关节的稳定性。而头侧小关节角更能反映小关节由冠状位向矢状位移行的趋向性。这一趋势在DLS患者中表现得尤为突出。
本研究认为,在DLS患者中,小关节角的增大说明小关节由冠状位向矢状位的空间趋向变化,该变化在小关节的头侧表现得较显著,在DLS中更明显,为DLS的病因预测提供了一种方法。
[1]Liao S,Zhan Y,Dong Z,et al.Automatic lumbar spondylolisthe-sis measurement in CT images[J].IEEE Trans Med Imaging,2016,35:1658-1669.
[2]Williams R,Cheung JP,Goss B,et al.An international multicenter study assessing the role of ethnicity on variation of lumbar facet joint orientation and the occurrence of degenerative spondylolisthesis in Asia Pacific:a study from the AOSpine Asia Pacific Research Collaboration Consortium[J].Global Spine J,2016,6:35-45.
[3]Schleich C,Muller-Lutz A,Blum K,et al.Facet tropism and facet joint orientation:risk factors for the development of early biochemical alterations of lumbar intervertebral discs[J].Osteoarthritis Cartilage,2016,24:1761-1768.
[4]Tsuji T,Watanabe K,Hosogane N,et al.Risk factors of radiological adjacent disc degeneration with lumbar interbody fusion for degenerative spondylolisthesis[J].J Orthop Sci,2016,21:133-137.
[5]Snoddy MC,Sielatycki JA,Sivaganesan A,et al.Can facet joint fluid on MRI and dynamic instability be a predictor of improvement in back pain following lumbar fusion for degenerative spondylolisthesis?[J].Eur Spine J,2016,25:1-8.
[6]Postacchini F,Postacchini R,Menchetti PP,et al.Lumbar interspinous process fixation and fusion with stand-alone interlaminar Lumbar instrumented fusion implant in patients with degenerative spondylolisthesis undergoing decompression for spinal stenosis[J].Asian Spine J,2016,10:27-37.
[7]Kobayashi T,Chiba H,Jimbo S,et al.Clinical,physical,and radiographic analyses of lumbar degenerative kyphosis and spondylolisthesis among community-based cohort[J].Eur Spine J,2016,25:1-6.
[8]Rao PJ,Ghent F,Phan K,et al.Stand-alone anterior lumbar interbody fusion for treatment of degenerative spondylolisthesis[J].J Clin Neurosci,2015,22:1619-1624.
Correlation study of the spatial tendency of vertebral facet joint and lumbar spondylolisthesis
GE Weiwei,WANG Huabin,YAO Jie,SUN Ping,LU Wenjuan.Department of Radiology,Nanjing Central Hospital Nanjing Governmental Hospital,Nanjing,210008,China.
Objective:To study the relationship between the spatial tendency of vertebral facet joint and degenerative lumbar spondylolisthesis.M ethods:A total of 300 patients were divided into 3 groups:L4/5DLS group of 89 cases,L5/S1DLS group of 156 cases,the control group with no lumbar disc herniation and spinal stenosis of 55 cases.All three groups were scanned with CT,the cephalad and caudad portion of facet joint angle of L3/4、L4/5and L5/S1segment were measured and comparative analysis were performed.Results:The differences between the cephalad and caudad portion of facet joint angle in DLS groups had significant difference,and the cephalad portion of facet joint angle was larger than the caudad side,the difference of the cephalad and caudad portion of facet angle in DLS groups compared with the control group was more significant.By the paired t-test,the facet joint angle of each segment between DLS groups and control group were compared statistically significant different.Conclusions:in cases of degenerative lumbar spondylolisthesis,the increasing of facet joint angle shows that space changes of facet joint from coronal orientation to sagittal orientation,and this change in the small joints of the cephalad side shows more significant,especially in the cases of degenerative lumbar spondylolisthesis,which provides a method to predict the etiology of degenerative lumbar spondylolisthesis.
Spondyloysis;Zygapophyseal joint;Spatial tendency;Facet joint angle
2016-09-07)
10.3969/j.issn.1672-0512.2017.04.011
南京市卫生局课题项目(YKK13194)。
葛卫卫,E-mail:690034791@qq.com。
图2a,2b分别为L4~5滑脱组的头、尾侧小关节角的箱式图图3a,3b分别为L5~S1滑脱组的头、尾侧小关节角的箱式图图4a,4b分别为对照组的头、尾侧小关节角的箱式图
