妊娠子宫破裂13例临床分析
2017-07-19华人意王彦林林楠郭玉娜
华人意,王彦林,林楠,郭玉娜
(中国福利会国际和平妇幼保健院妇产科,上海 200030)
妊娠子宫破裂13例临床分析
华人意,王彦林,林楠,郭玉娜
(中国福利会国际和平妇幼保健院妇产科,上海 200030)
探讨妊娠时子宫破裂发生的原因,总结临床治疗经验,从而更好地诊断处理这一产科急症.从病史、临床特点、治疗手段及母婴预后等多方面比较分析了2009年1月至2016年12月中国福利会国际和平妇幼保健院子宫破裂病例13例,其中完全性子宫破裂占69.23%,不完全性子宫破裂占30.77%.13例子宫破裂患者中,3例经阴道分娩,1例为阴道分娩中转剖宫产分娩,1例剖宫取胎,8例为剖宫产分娩.在病因方面,疤痕子宫占69.23%,原发性子宫破裂占30.77%.在临床处理方面,除2例行全子宫切除外,其余11例均行子宫破裂修补术.子宫破裂是严重的产科并发症,产妇及新生儿并发症发生率较高.疤痕子宫是最主要的病因,子宫破裂通常以剧烈腹痛及胎心异常为临床表现,在临床上应严密观察,结合病史及早对子宫破裂作出诊断.
子宫破裂;临床特点;高危因素
子宫破裂是一种严重危害母婴生命安全的产科并发症,发生率约为1/4 336∼1/1 235[1].子宫破裂的并发症包括产时及产后出血、失血性休克、弥散性血管内凝血(disseminated or diffuse intravascular coagulation,DIC)、胎儿宫内窘迫甚至胎死宫内,使输血治疗及子宫切除风险增加.本工作回顾性分析了中国福利会国际和平妇幼保健院自2009年1月至2016年12月共13例子宫破裂病例,并对子宫破裂的病因及临床特点进行了分析.
1 研究方法
收集2009年1月至2016年12月妊娠子宫破裂病例,共13例.所有患者均经手术确诊.
2 结果
2.1 患者基本资料
13名患者年龄为25∼41岁,平均年龄为32.8±5.75岁,孕周为18∼41周,平均孕周为35+ 6周.近期手术距本次妊娠时间平均为3.86±2.55a.35岁及以上高龄孕妇5人,合并巨大儿1例,合并妊娠期糖尿病(gestational diabates mellitus,GDM)3例,合并妊娠期高血压1例.
2.2 子宫破裂的类型及危险因素
13例患者中完全性子宫破裂9例(占69.23%),不完全性子宫破裂4例(占30.77%).疤痕子宫9例,其中子宫肌瘤剥除术后1例,前次剖宫产术后8例(其中前两次剖宫产2例,前次剖宫产合并子宫肌瘤剥除术后1例),原发性子宫破裂4例.在原发性子宫破裂中,有3例为完全破裂,1例为不完全破裂,2例经过引产.
2.3 临床处理及妊娠结果
13例子宫破裂患者中,3例经阴道分娩,1例为阴道分娩中转剖宫产分娩,1例为剖宫取胎,8例为剖宫产分娩.10例手术终止妊娠病例中,4例因“胎儿宫内窘迫”及“羊水Ⅲ度”手术, 2例以腹痛为临床表现,3例经阴道分娩病例均以产后出血为主要临床表现.在临床处理方面,除2例行全子宫切除外,其余11例均行子宫破裂修补术.子宫破裂后发生失血性休克有7例, DIC 1例,无孕产妇死亡.在新生儿预后方面,除1例胎死宫内及1例新生儿重度窒息外,其余新生儿预后良好,10 minApagar评分10分(见表1).
3 讨论
子宫破裂的临床表现不典型,主要症状包括剧烈腹痛、肌紧张、阴道流血、失血性休克,因此早期诊断子宫破裂有一定难度.但临床发现子宫破裂常伴有胎儿心率变化,因此胎心监护发现胎窘可作为诊断的重要辅助手段[2].荷兰的一项研究比较了前次剖宫产后阴道试产过程中子宫完全性破裂及试产成功产妇第一产程胎心监护报告,发现在77%子宫破裂病例中,会出现病理性胎心监护,主要表现为10次以上的重度变异减速[3].但目前为止,还没有发现与子宫破裂相关的特异性胎心监护波形[4].
在病因方面,子宫破裂最常见的原因是前次剖宫产[5-6].子宫下段切口的缝合方式对剖宫产后子宫破裂发生的影响一直是产科医生关注的话题.已有研究指出,单层缝合法相比双层缝合,子宫破裂发生率升高4倍[7].2014年,一项针对19 604名经产妇的研究发现,7 683名前次剖宫产后阴道分娩的产妇中,子宫破裂的发生率为1.3%(103名).回顾这些产妇的手术记录发现,前次剖宫产手术中双层缝合与单层缝合在子宫破裂的发生率方面没有差异.
在育龄期妇女中,子宫肌瘤的发生率为20%∼25%[8].经开腹子宫肌瘤剥除术后,妊娠期子宫破裂发生率极低,两项临床研究回顾了236 454例分娩,在209例子宫破裂中,仅4例与子宫
肌瘤剥除有关[9-10].在412名接受经腹子宫肌瘤剥除患者中,子宫破裂的发生率为0.2%(1例).磁共振成像(magnetic resonance imaging,MRI)发现经腹子宫肌瘤剥除的子宫伤口大约在术后12周愈合,一般不伴有血肿或水肿[11-12].腹腔镜技术在临床中的应用越来越广泛.与传统开腹手术相比,腹腔镜手术创面小,术后恢复快,住院时间短[13].尽管许多临床研究提出腹腔镜子宫肌瘤剥除术后并无子宫破裂情况的发生,但在近20年中,至少有15例子宫破裂报道与之相关[14-17].目前,子宫破裂并不被作为腹腔镜术后并发症,但有学者指出不成熟的子宫缝合技术、止血不充分导致血肿形成或过度使用单极、双极电凝止血都会增加术后子宫破裂的风险[18].产后的子宫复旧及重塑是一个特殊的过程,肌瘤剥除后的子宫伤口愈合与剖宫产子宫疤痕不同.不完全子宫破裂病理提示,病灶处胶原成分增加而肌肉组织成分减少[19].肌瘤剥除后子宫疤痕处取样提示TGFβ3减少,成纤维细胞生长因子表达量增加,血管表皮生长因子、血小板分化生长因子以及TNFα表达量轻度升高.近两年,要求在前次剖宫产后进行阴道试产(trial of labor after cesarean,TOLAC)的产妇越来越多.国外研究统计显示,每年有47.2%∼71.7%前次剖宫产的产妇要求进行TOLAC,其中剖宫产后阴道分娩(vaginal birth after cesarean,VBAC)的成功率为63.4%∼76.0%[20-21].目前,我国临床VABC主要参照英美医学会及妇产科学会相关指南进行,还没有以循证医学为基础的子宫肌瘤剥除术后分娩方式的相关指南.
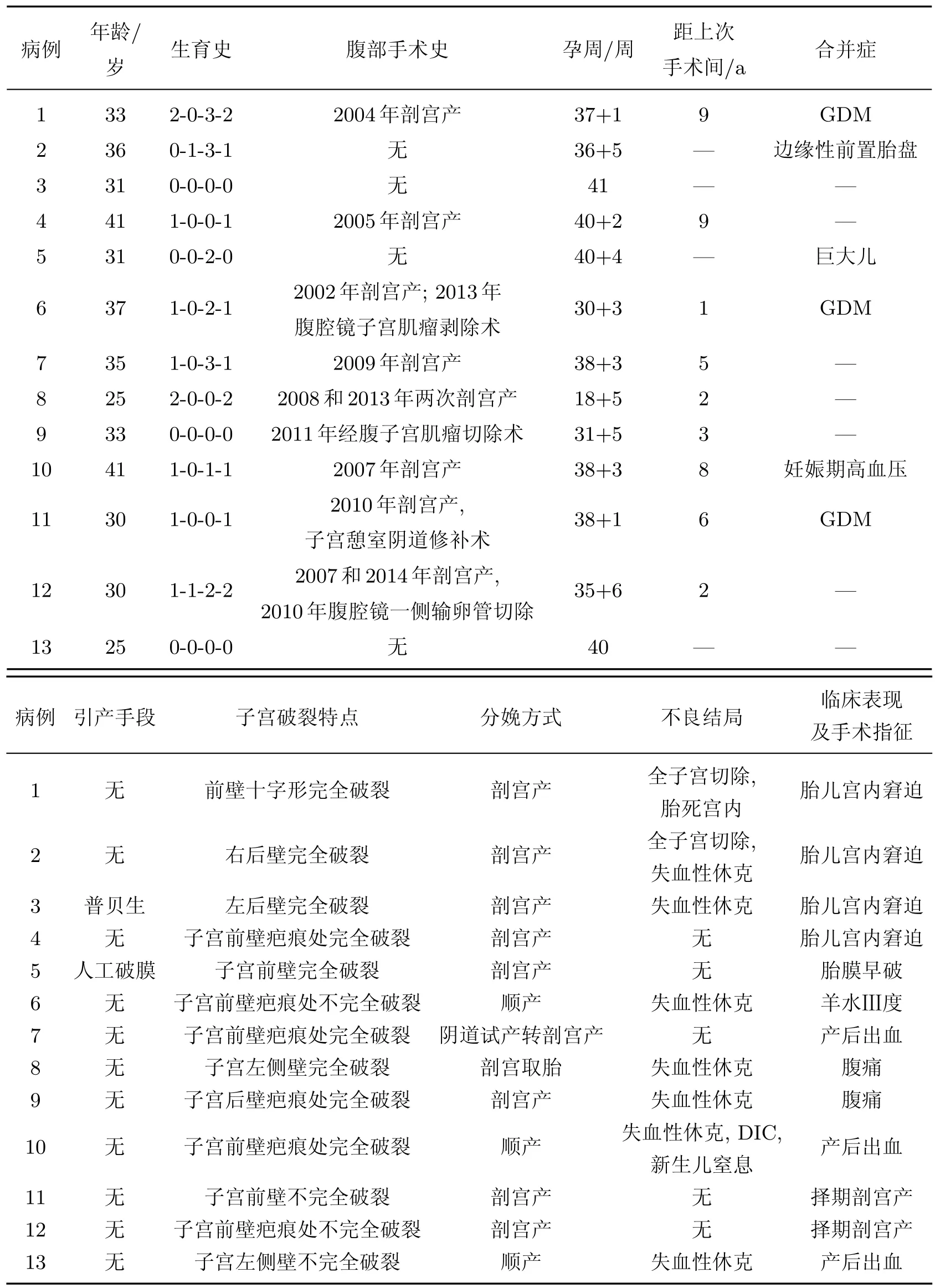
表1 子宫破裂患者的临床特点及结局Table 1 Clinical characters of patients with uterine rupture
除外继发于疤痕子宫的子宫破裂,文献[22]报道了原发性子宫破裂的发生率为1/16 000.在本工作研究的13例患者中,原发性子宫破裂占30.77%.一些大样本研究指出,原发性子宫破裂在临床上往往较难及时被诊断,妊娠结果相对继发子宫破裂不理想[5].导致原发性子宫破裂的危险因素主要包括产妇年龄大于35岁,身高小于160 cm,胎儿体重大于4 500 g或大于胎龄.临床案例报道指出,前置胎盘可能也是子宫破裂的高危因素之一[2,23].
在治疗方面,本工作中大部分病例都成功接受了子宫破裂修补术,预后良好.Patricio等[24]通过腹腔镜检查发现一例孕20周发生的子宫破裂,并在腹腔镜下进行了修补,后产妇继续妊娠,并在孕34周时进行剖宫产,母儿预后均良好.
4 总结
随着国家对“二胎”政策的全面开放,以及临床TOLAC的开展,应随时警惕子宫破裂的发生.在产程中加强观察,应对子宫破裂做到早发现早处理,降低这一严重并发症对母婴健康的影响.同时,应加强临床研究,找到临床有特异性的子宫破裂预测指标.
[1]Egbe T O,Halle-Ekane G E,Tchente C N,et al.Management of uterine rupture:a case report and review of the literature[J].BMC Research Notes,2016,9(1):492.
[2]Kawabe A,Wang L,Kikugawa A,et al.Severe abdominal pain exacerbated by fetal movement is an early sign of the onset of uterine rupture[J].Taiwanese Journal of Obstetrics&Gynecology, 2016,55(5):721-723.
[3]Andersen M M,Thisted D L,Amer-Wahlin I,et al.Can intrapartum cardiotocography predict uterine rupture among women with prior caesarean delivery?:a population based casecontrol study[J].PloS One,2016,11(2):e0146347.
[4]Ridgeway J J,Weyrich D L,Benedetti T J.Fetal heart rate changes associated with uterine rupture[J].Obstet Gynecol,2004,103(3):506-512.
[5]Zwart J J,Richters J M,Ory F,et al.Uterine rupture in the Netherlands:a nationwide population-based cohort study[J].BJOG,2009,116(8):1069-1080.
[6]Kaczmarczyk M,Sparen P,Terry P,et al.Risk factors for uterine rupture and neonatal consequences of uterine rupture:a population-based study of successive pregnancies in Sweden[J].BJOG,2007,114(10):1208-1214.
[7]Durnwald C,Mercer B.Uterine rupture,perioperative and perinatal morbidity after singlelayer and double-layer closure at cesarean delivery[J].Am J Obstet Gynecol,2003,189(4): 925-929.
[8]Buttram V C,Jr Reiter R C.Uterine leiomyomata:etiology,symptomatology,and management[J].Fertility and Sterility,1981,36(4):433-445.
[9]Garnet J D.Uterine rupture during pregnancy.An analysis of 133 patients[J].Obstet Gynecol, 1964,23:898-905.
[10]Palerme G R,Friedman E A.Rupture of the gravid uterus in the third trimester[J].Am J Obstet Gynecol,1966,94(4):571-576.
[11]Tsuji S,Takahashi K,Imaoka I,et al.MRI evaluation of the uterine structure after myomectomy[J].Gynecol Obstet Invest,2006,61(2):106-110.
[12]Darwish A M,Nasr A M,Ei-Nashar D A.Evaluation of postmyomectomy uterine scar[J]. Journal of Clinical Ultrasound,2005,33(4):181-186.
[13]Jin C,Hu Y,Chen X C,et al.Laparoscopic versus open myomectomy—a meta-analysis of randomized controlled trials[J].Eur J Obstet Gynecol Reprod Biol,2009,145(1):14-21.
[14]Malzoni M,Sizzi O,Rossetti A,et al.Laparoscopic myomectomy:a report of 982 procedures[J].Surgical Technology International,2006,15:123-129.
[15]Hockstein S.Spontaneous uterine rupture in the early third trimester after laparoscopically assisted myomectomy.A case report[J].The Journal of Reproductive Medicine,2000,45(2): 139-141.
[16]Parker W H,Iacampo K,Long T.Uterine rupture after laparoscopic removal of a pedunculated myoma[J].Journal of Minimally Invasive Gynecology,2007,14(3):362-364.
[17]Oktem O,Gokaslan H,Durmusoglu F.Spontaneous uterine rupture in pregnancy 8 years after laparoscopic myomectomy[J].The Journal of the American Association of Gynecologic Laparoscopists,2001,8(4):618-621.
[18]Koh C,Janik G.Laparoscopic myomectomy:the current status[J].Current Opinion in Obstetrics&Gynecology,2003,15(4):295-301.
[19]Pollio F,Staibano S,Mascolo M,et al.Uterine dehiscence in term pregnant patients with one previous cesarean delivery:growth factor immunoexpression and collagen content in the scarred lower uterine segment[J].Am J Obstet Gynecol,2006,194(2):527-534.
[20]Knight H E,Gurol-Urganci I,Van Der Meulen J H,et al.Vaginal birth after caesarean section:a cohort study investigating factors associated with its uptake and success[J].BJOG, 2014,121(2):183-192.
[21]Kwee A,Bots M L,Visser G H,et al.Obstetric management and outcome of pregnancy in women with a history of caesarean section in the Netherlands[J].Eur J Obstet Gynecol Reprod Biol,2007,132(2):171-176.
[22]Gibbins K J,Weber T,Holmgren C M,et al.Maternal and fetal morbidity associated with uterine rupture of the unscarred uterus[J].Am J Obstet Gynecol,2015,213(3):382.e1.
[23]Hung F Y,Wang P T,Weng S L,et al.Placenta percreta presenting as a pinhole uterine rupture and acute abdomen[J].Taiwanese Journal of Obstetrics&Gynecology,2010,49(1): 115-116.
[24]Patricio L,Martins D,Henriques A,et al.Repaired uterine rupture at mid gestation[J]. Archives of Gynecology and Obstetrics,2013,288(2):457-458.
Clinical analysis of 13 patients with uterine rupture during pregnancy
HUA Renyi,WANG Yanlin,LIN Nan,GUO Yuna
(Obstetrics and Gynecology Department,International Peace Maternity and Child Health Hospital of China Welfare Institution,Shanghai 200030,China)
To analyze the high-risk factors,clinical characteristics and prognosis of uterine rupture during pregnancy,clinical data of 13 patients with uterine rupture in International Peace Maternity and Child Health Hospital from January 2009 to December 2016 were analyzed retrospectively.Among the 13 patients,69.23%had complete uterine rupture. The rest had incomplete uterine rupture.3 patients had vaginal delivery;1 had a trial of vaginal delivery followed by a caesarean section,and 8 had caesarean section.9 patients had scarred uterus.Hysterectomy was performed in 2patients.Scarred uterus is one of the most common risk factors of uterine rupture during pregnancy.A typical symptom of uterine rupture is continuous abdominal pain.Prognosis of the uterine rupture requires further investigation.
uterine rupture;clinical characteristics;risk factor
R 711.4
A
1007-2861(2017)03-0402-06
10.12066/j.issn.1007-2861.1937
2017-04-07
国家自然科学基金青年基金资助项目(81300513);上海交通大学“医工交叉研究基金”资助项目(YG2014MS37)
郭玉娜(1973—),女,副主任医师,研究方向为产科相关疾病.E-mail:gyuna@live.com
