Telemedicine: Its Importance in Cardiology Practice. Experience in Chile
2017-05-23EdgardoEscobarMDFACCFAHAandCarlosAkelMDFACP
Edgardo Escobar, MD, FACC, FAHA and Carlos Akel, MD, FACP
1Department of Medicine, University of Chile, International Telemedical System, Chile
Introduction
The objective of telemedicine (TM) is to provide medical assistance in remote locations in the fields of diagnosis, treatment, prevention, and rehabilitation, performed by qualified professionals.
TM makes use of information and communications technology (ICT) to provide medical care,including surgical procedures, regardless of the location of the patients [1, 2].
Telehealth may be de fined as the use of ICT to support distant medical care (teleconsultation, teleimaging, telepathology, teledermatology, telecardiology, etc.). Synonymous terms such as “e-health”and “virtual medicine” are also used.
There are two principal ways to offer TM services, namely:
1. Real time; for example, videoconferences and telerobotic systems with transmission in real time between health providers and patients (consultations and procedures), and between the same health providers and specialists (second opinion and discussions of cases), or distance monitoring of patients and transmission to a health provider with use of electronic tools. It requires a large bandwidth and it is more expensive.
2. Store and forward: transmission of prerecorded videos of digital images (teleimaging, telepathology, teledermatology, teleelectrocardiography, etc.) between patients and primary care physicians and specialists.
Store and forward is typically used by specialty practices in fields such as radiology, ophthalmology,and dermatology. These fields rely on documented information and images rather than on physical examination of the patient.
In contrast, real-time technology is very effective for practitioners who need to see a large number of patients, make frequent follow-up visits, or provide immediate advice to patients.
To sum up, we are already in the era of making use of technology to improve population health.This is a process of transformation of the practice of medicine through ICT.
TM supports rural facilities in the training and retaining of clinicians because it allows on-the-job experience and remote participation in grand rounds. It would be desirable to include TM in the daily work of providers, define a correct strategy to apply it, and establish a formal organization dedicated to the project.
A 28% annual growth of TM visits among rural Medicare beneficiaries has recently been reported[3]. In developing countries, rather than build and staff a large number of sophisticated facilities, TM allows basic clinics to consult and share the expertise of a medical specialist located anywhere in the world[4]. Cost-effectiveness and patient satisfaction have been demonstrated [2], and the American College of Physicians has recently made recommendations to guide the use of TM in primary care settings [5].
Telecardiology
In the field of cardiology, TM is playing a very important role [6]. For instance, TM has proved to be effective in improved control of risk factors in the general population [7, 8]. Among other applications of TM in cardiology, diagnosis and/or control of hypertension, cardiac failure, arrhythmias, and ST-elevation myocardial infarction (STEMI) are important examples.
It has been shown that self-control, when combined with telemonitoring of blood pressure, is a significant improvement in hypertension control at the primary care level. Telemonitoring of hypertension may produce reliable data and it is well accepted by patients [9–11].
In congestive heart failure, TM is associated with lower rates of hospitalization, although it is not clear if there is an impact on prognosis [12–16].It has also been shown that remote monitoring of implantable devices contributes to earlier detection of relevant clinical events, which may, in turn,result in timely medical interventions [17].
In the management of acute coronary syndromes,TM has proved to be very useful [18], particularly in the prehospital management of acute STEMI [19].
Electrocardiogram (ECG) is the gold standard for the diagnosis of STEMI and it is the key tool in the systems of treatment. With proper identification of STEMI, it is possible to significantly shorten previous stages and to transfer the patient directly to the catheterization laboratory for primary angioplasty,or thrombolysis can be performed at the place of first medical contact.
Multiple studies have demonstrated that the performance of a prehospital ECG decreases door-toreperfusion and door-to-balloon times significantly.A time of 90 min or less can be achieved in 86%of cases of STEMI when a prehospital ECG is performed [20].
In American as well as in European guidelines,performance of a prehospital ECG is a class 1 recommendation in patients with symptoms of STEMI[21, 22]. In this scenario, the accurate identification of a suspected STEMI with a proper ECG diagnosis is extremely important. TM has allowed the implementation of a system that allows the performance of a high-quality 12-lead ECG at the place of first medical contact and to relay the ECG via wireless broadcast to a center where a specialist will perform the correct diagnosis.
A meta-analysis revealed a 35% decrease in hospital mortality with the use of TM in cases of STEMI compared with a control group [23]. It has been shown how TM helps to install a network of prompt diagnosis and treatment of STEMI [24].
Experience in Chile
In Chile, cardiovascular diseases constitute the main cause of death among the population, with a mortality rate of 29% for cardiovascular episodes. Within this mortality rate, coronary heart disease accounts for 31% of deaths and cerebrovascular disease accounts for 32% of deaths. For coronary heart disease, the main cause of death is myocardial infarction. TM has made an important contribution toward the solution of this problem mainly in the field of cardiac emergencies. A system of TM as described earlier requires (1) physicians who are experts in ECG diagnosis, (2) communication, and (3) ICT.
Our service has specialists on a 24/7 schedule,and each month processes reports of more than 50,000 ECGs sent from all over the country, including Easter Island. Chile has a good telecommunications system, and our platform allows the fast generation of reports, which are sent via the Internet back to the place of first medical contact, and other places if required. The achievement of more than 50,000 ECGs a month is possible thanks to the use of a software package developed by our engineers,called Integrated Platform of Telemedicine (IPT). A 12-lead ECG is performed at the place of first medical contact with a very small device [24] that is able to transmit the ECG as an analog/digital signal by phone, cell phone, or the Internet to a call center staffed by paramedics and specialists on a 24/7 basis.Technical service is provided by a private company,International Telemedical Systems (Figure 1).
ECGs are received in a computer by trained paramedics. If the tracings are technically correct, after all the clinical and demographic data (from a predesigned list) have been recorded, they are directed to the specialist’s computer. This stage takes only a few minutes. All reports are stored in a central database, which allows the immediate comparison of the actual tracing with previous ones of the same patient or access to the tracings at any time.
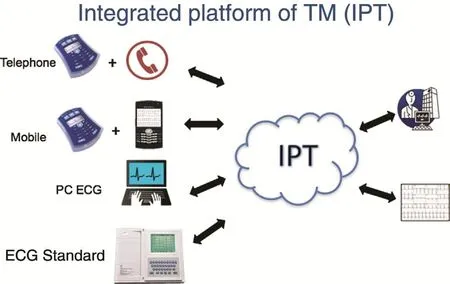
Figure 1 Different Ways of Transmitting ECGs to the Integrated Telemedicine Platform (IPT).
Paramedics are trained to recognize a possible subepicardial lesion and other cardiac emergencies such as bradyarrhythmia or tachyarrhythmia. In these cases the paramedic alerts physicians to give priority to the reports or to the request of the physician in charge. The physician clicks on one of the ECGs according to its priority, and to make the report has three screens. On the central screen the present 12-lead ECG may be seen, with the clinical data as recorded by the paramedic. On this screen the system displays the 12-lead ECG and a 6 seconds duration D2 lead, with electronic signals at the beginning of the P and QRS waves and at the end of the QRS and T waves, calculating automatically heart rate, PQ and QT intervals, and QRS duration. It also displays a signal for ST-segment position (Figure 2).
The physician may change the D2 lead by clicking on any of the 11 other leads and may change the position of the electronic signals if they are not properly situated. The central screen also displays three columns: The first column contains a list of the 14 main categories of ECG diagnosis; for example, arrhythmias, bundle branch blocks, atrioventricular blocks,enlargements of cavities, and pacemaker rhythm. If the physician clicks on one of these main diagnoses,a number of other possibilities are displayed. For instance, there are 52possibilities for arrhythmias(second column). When the physician selects from this list, these possibilities are automatically transferred to a third column, and these diagnoses are sent to the database for future review. Physicians may also add a comment or suggest a new assessment,sentences that are also listed in the first column.
The other two screens are a magnified display,one of the last ECG of the patient, and the other of the present one for comparison purposes. The system allows the review of all previous tracings of the patient and to compare, lead by lead, the present tracing with the previous one or any of the other ECGs.
In other words, physicians do not need to write reports in much detail, which makes the reporting a very quick procedure that takes only a few minutes.This is particularly important for ECGs with ST-T segment elevation suggesting a subepicardial lesion as recognized by the paramedics in their computers.These tracings have absolute priority and the report must be sent to the place of first medical contact within 10 min. In this case or in any other cardiac emergency, the physician making the report may contact the physician in charge to give advice. It is also important to emphasize that all the tracings are audited by a specialist assigned for that purpose almost immediately during the daytime, and the first thing in the morning for those tracings received overnight.
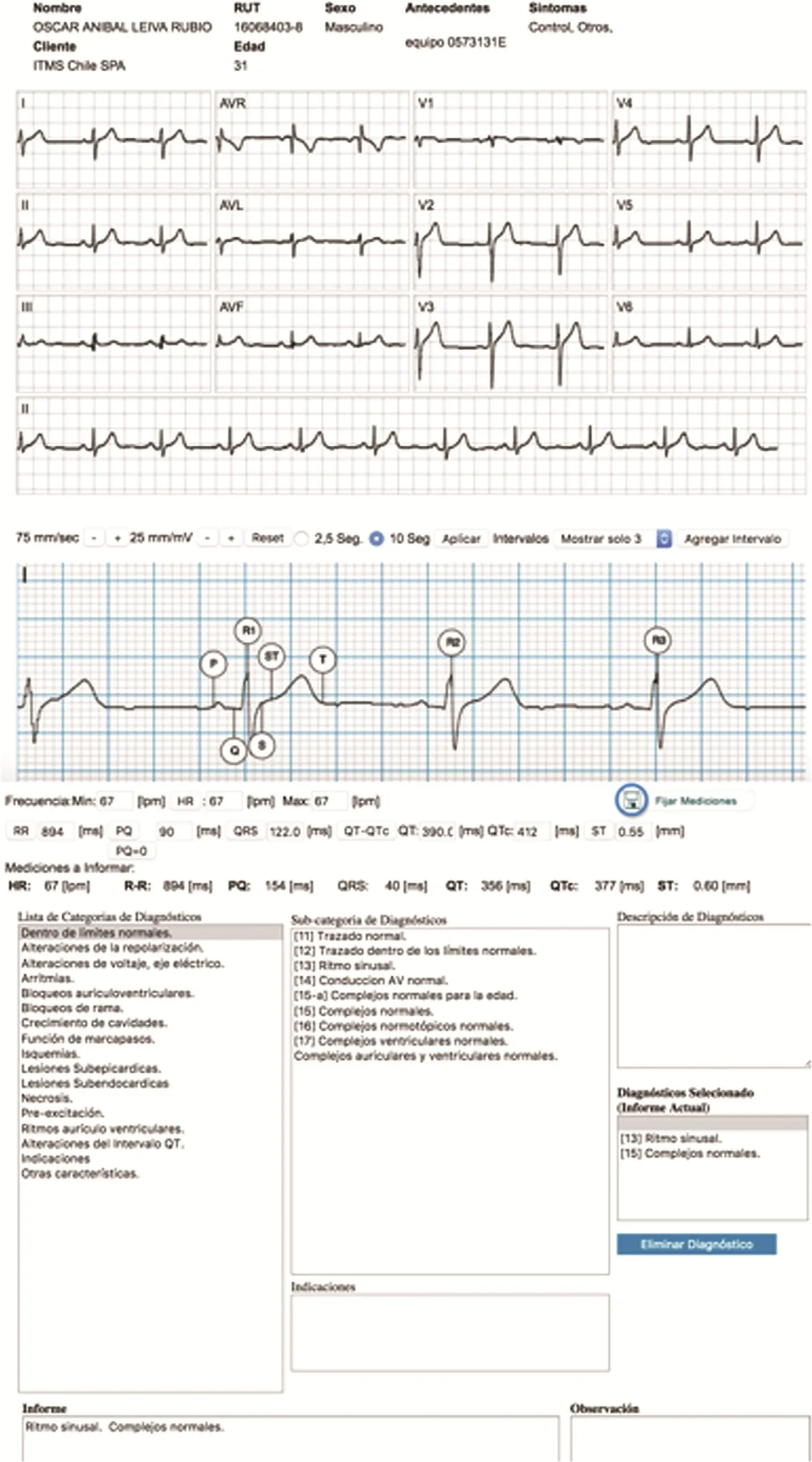
Figure 2 Main Screen Image for ECG Report.
We strongly believe that this system of TM with specialists making the ECG report on a 24/7 basis is better than relying on ECG diagnosis by trained paramedics or nonspecialist physicians.
If the paramedic recognizes an ST-segment elevation, this ECG has absolute priority and should be immediately interpreted by the cardiologist. This can be done in less than 10 min, and the result is sent not only to the place of first medical contact but also simultaneously to the referral hospital as defined by the Ministry of Health. In these cases,there is also a direct interaction of the cardiologist on duty with the physician in charge of the patient.
Among other important political decisions in Chile, there is a law called Garantías Explícitas de Salud (GES; Explicit Health Guarantees) [25].According to this law, the health care system has the obligation to take care of 80 diseases in a predetermined period. If an acute coronary event is suspected, an ECG should be performed in the first 15 min at the place of first medical contact, and diagnosis of STEMI should be con firmed by the TM system specialist.
Since May 1, 2004, the Ministry of Health has implemented national coverage of ECG TM for the purpose of diagnostic interpretation and the possibility of performing thrombolysis even in rural areas. The impact of the GES law has been very significant. Mortality due to STEMI decreased from 12% in the era before the GES law to 8.6%(odds ratio 0.64), adjusted for many other variables.This reduction in mortality was more important in higher-risk patients [26].
From our database of ECGs received, we have analyzed the incidence of STEMI in Chile from 523,371 ECGs [27]. Greater incidence of STEMI in men (69.2%) and its presentation in older age in women were found. STEMIs were more frequent between April and June (i.e., in autumn) and between 9 a.m. and 1 p.m. We have also studied the prevalence of Brugada patterns [28] throughout the country from 122,000 tracings, including those of children. Type 1 Brugada pattern was present in 4.6 in 10,000 tracings, which is similar to figures found in other countries of the Western hemisphere. The frequency of long corrected QT (QTc) interval in different ECG patterns was studied in 13,600 tracings [29]. The most important findings were a long QTc interval in 16% of ECGs that were otherwise normal and in 8% of patients with left ventricular enlargement. We had the opportunity to evaluate the impact of a major earthquake in Chile on a weekend in February 2010 on the incidence of STEMI at the precise moment the earthquake was happening [30].We analyzed 280,592 ECGs from all over the country recorded on weekends in a period of 12 months between 2009 and 2010. There was a statistically significant increase in the incidence of subepicardial lesions during the earthquake compared with any other weekend, being more frequent in women(75%), the reverse of the general finding described above.
TM also allows ambulatory blood pressure monitoring and ECG 24-h monitoring recordings, with a time delay of less than 24 h for the report. Besides cardiology, our system also has applications in spirometry and imaging, which as for cardiology TM, are very important for support of primary care in Chile.
What has been mainly recognized by the users of the system is the fast interpretation of the data,the possibility of sending an ECG from any part of the country, and the ease with which the equipment can be moved and managed. Other advantages are its permanent availability, a prompt second opinion from a cardiologist, avoiding unnecessary transfer of patients who do not need it, and the cost-effectiveness of the system.
TM is an important support for public health, particularly primary care because of its extensive coverage and low cost.
To sum up, TM is a system that gives patients equal access to care and allows primary care physicians to solve problems whose solutions would otherwise be delayed. It is also a support for the specialist, who may count on rapid diagnostic support as in the case of an acute coronary event.
REFERENCES
1. Bhavnani SP, Narula J, Sengupta P. Mobile technology and digitization of health care. Eur Heart J 2016;37:1428–38.
2. Bashour RL, Howell JD, Krupinski EA, Harms KM, Bashour N, Doarn C. The empirical foundations of telemedicine interventions in primary care. Telemed E Health 2016;22:342–75.
3. Mehrotra A, Jena A, Busch A,Souza J, Uscher-Pines L, Landon BE. Utilization of Telemedicine among rural medicare bene ficiaries.J Am Med Assoc 2016;315:2015–6.
4. Keely E, Liddy Cl, Afkham A.Utilization, bene fits and impact of e-consultation service across diverse e-consultation specialties and primary care providers.Telemed E Health 2013;19:733–8.
5. Daniel H, Sulmasy LS. Policy recommendations to guide the use of Telemedicine in primary care settings: an American College of Physicians position paper. Ann Intern Med 2015;163:787–9.
6. Sorensen JT, Clemensen P,Sejersten M. Telecardiología: pasado, presente y futuro. Rev Esp Cardiol 2013;66:212–8.
7. Krakoff LR. Management of cardiovascular risk factors is leaving the of fice: potential impact of telemedicine. J Clin Hypertens 2011;13:791–4.
8. Ganesan AN, Louise J, Horsfall M, Bilsborough Sh A, Hendriks J,McGavigan AD, et al. International he alth intervention on physical activity, sitting and weight.The stepathlon cardiovascular health study. J Am Coll Cardiol 2016;67:2453–63.
9. McManus RJ, Mant J, Bray EP,Holder R, Jones MI, Green field S, et al. Telemonitoring and selfmanagement in the control of hypertension (TASMINH2): a randomized controlled trial. Lancet 2010;376:163–72.
10. Magid DJ, Olson KL, Billups SJ,Wagner NM, Lyons EE, Kroner BA. A pharmacist led, American Heart Association Heart 360 Webenabled home blood pressure monitoring program. Circ Cardiovasc Qual Outcomes 2013;6:157–63.
11. Varleta P, Akel, C, Acevedo M,Salinas C, Pino J, Garcia A, et al. Mobile phone text messaging improves antihypertensive drug adherence in the community.Circulation 2014;130:A18144.
12. Polisena J, Tran K, Cimon K. Home tele monitoring for congestive heart failure: a systematic review and meta-analysis. J Telemed Telecare 2010;16:68–76.
13. Hasan A, Paul V. Tele monitoring in chronic heart failure. Eur Heart J 2011;32:1457–64.
14. Inglis SC, Clark RA, McAlister FA,Stewart S, Cleland JG. Which components of heart failure programs are effective? A systematic review and meta-analysis of the outcomes of structured telephone support or telemonitoring as the primary component of chronic heart failure management in 8323 patients:abridged Cochrane Review. Eur J Heart Fail 2011;13:1028–40.
15. Weintraub A, Gregory D, Patel AR, Levine D, Venesy D, Perry K, et al. A multicenter randomized controlled evaluation of automated home monitoring, and telephonic disease management in patients recently hospitalized for congestive heart failure; the SPAN-CHF II trial. J Card Fail 2010;16:285–92.
16. Koehler F, Winkler S, Schieber M,Sechtem U, Stangl K, Bohm M,et al. Tele medical interventional monitoring in heart failure investigators: impact of remote tele medical management on mortality and hospitalizations in ambulatory patients with chronic heart failure: the telemedical interventional monitoring in heart failure study.Circulation 2011;123:1873–80.
17. Bhavnani S, Waalen J, Srivastava A, Heywood JT. Which patients?Which devices? Health monitoring with wearable and implantable devices in heart failure: meta-analysis of randomized trials. J Am Coll Cardiol 2015;65 (Issue 10S, A 1030).
18. Clemensen P, Loumann-Nielsen S,Sejersten M. Telemedicine fighting acute coronary syndromes. J Electrocardiol 2010;43:615–8.
19. Escobar E, Barbagelata A.Prehospital management of acute STEMI. Practical approaches and international strategies for ea rly intervention. Minneapolis:Cardiotext Publishing; 2015.
20. Quinn T, Johnhsen S, Gale C,Snooks H, McLean S, Woollard M, et al. Effects of prehospital 12 lead electrocardiogram on process of care and mortality of acute coronary syndrome: a linked cohort study from the myocardial ischemia national audit project.Heart 2014;100:944–50.
21. O’Gara PT, Kushner FG, Ascheim DD, Casey DE, Chung MK, de Lemos JA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2013;127:529–55.
22. Steg PG, James SK, Atar D, Badano LP, Lundqvist CB, Borger MA, et al. ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J 2012;33:2569–619.
23. de Waure C, Codeddu C, Gualano M, Ricciardi W. Telemedicine for the reduction of myocardial infarction mortality: a systematic review and a meta-analysis of published studies.Telemed E Health 2102;18:1–6.
24. Cardioline 2015. Available from:http://eng.cardioline.com/prodotti-cardioline/microtel-bt-tel/.Accessed 29 November 2016.
25. AUGE Chilean Ministry of Health.2007. Available from: http://www.supersalud.gob.cl/normativa/668/articles-3174_recurso_1.pdf.Accessed 29 November 2016.
26. Nazal C, Campo P, Corbalan R, Lanas F, Bartolucci J, Sanhueza P, et al.Impacto del plan AUGE en el tratamiento de pacientes con Infarto agudo del miocardio con supradesnivel ST en hospitales chilenos. Rev Med Chil 2008:136:1231–9.
27. Escobar E, Vejar M, del Pino R.Lesiones subepicárdicas en Chile(infarto agudo del miocardio con supradesnivel del segmento ST).Experiencia con telemedicina. Rev Chil Cardiol 2009;28:73–80.
28. Escobar E, Adriazola P, Bello F,Orellana M, Trejo P. Prevalence of EKG Brugada pattern: experience in Chile. Telemed E Health 2008;14(Suppl 1):64.
29. Orellana M, Bello F, Escobar E,Adriazola P, Trejo P, Gonzalez P.Prevalencia del intervalo QT prolongado en diferentes patrones electrocradiográ ficos. Estudio por Telelectrocardiogra fia. Rev Chil Cardiol 2009;28:349–56.
30. Bello F, Adriazola P, Escobar E, Pavlov S, Mezzano G, Lama D. Terremoto 2010: impacto de la incidencia de lesiones subepicárdicas. Experiencia con Telemedicina. Rev Chil Cardiol 2012;31:189–93.
杂志排行
Cardiovascular Innovations and Applications的其它文章
- Takotsubo Syndrome: Does the Octopus Trap Hide Dangers?
- Digoxin and Heart Failure: Are We Clear Yet?
- Role of Cholesterol Crystals During Acute Myocardial Infarction and Cerebrovascular Accident
- Evaluation of Multidisciplinary Collaborative Care in Patients with Acute Coronary Syndrome and Depression and/or Anxiety Disorders
- Chronic Kidney Disease is a New Target of Cardiac Rehabilitation
- Occlusive Spasm of the Left Anterior Descending Artery and First Diagonal Branch After Implantation of Everolimus Eluting Stents Without Re-stenosis in a Female Patient with Resting Angina
