微创技术治疗妇科手术后输尿管损伤(附33例报告)
2017-04-26李茂林卓栋章静王治国敖平
李茂林 卓栋 章静 王治国 敖平
1皖南医学院附属弋矶山医院泌尿外科 241001 安徽芜湖
微创技术治疗妇科手术后输尿管损伤(附33例报告)
李茂林1卓栋1章静1王治国1敖平1
1皖南医学院附属弋矶山医院泌尿外科 241001 安徽芜湖
目的:探讨妇科手术导致输尿管损伤行输尿管镜和腹腔镜治疗的安全性及有效性。方法:回顾性分析2008年1月~2016年6月妇科手术发生输尿管损伤并微创治疗的33例患者临床资料。平均年龄45(20~69)岁。术中发现输尿管损伤5例,即刻使用腹腔镜或膀胱镜置入双J管,腹腔镜下输尿管修补缝合或输尿管端端吻合;术后延迟发现输尿管损伤28例,其中1例为孤立肾患者,术后8 h发现引流液量异常多并行输尿管镜检查,见输尿管下段局部缺损,予置入双J管并腹腔镜下修补输尿管。其余均在术后7~35 d出现阴道残端漏尿。先行输尿管镜直视下置入双J管,置管成功16例,予以留置2~3个月。失败11例患者行腹腔镜探查。若损伤位置低,输尿管与膀胱直接插入吻合。若损伤位置高,则游离裁剪膀胱壁瓣并缝合成管状与输尿管吻合。结果:16例术后延迟发现输尿管损伤并成功置入双J管,有1例患者长期漏尿,3个月后再行腹腔镜手术成功,其余膀胱镜下拔除双J管无漏尿的发生。11例置管失败的患者均一期行腹腔镜修复手术成功。手术耗时110~160 min,平均132 min。术后住院5~8 d,平均6 d,予以保留导尿3~4周,术后4~8周膀胱镜下拔除双J管。全部病例术后3~6个月行B超检查提示轻度肾积水。结论:妇科手术致输尿管损伤可置入双J管,置管成功经保守治疗效果理想。置管后保守治疗失败可行腹腔镜治疗,虽然具有一定挑战,但安全有效,相比传统手术具有创伤小、瘢痕少、术后恢复快等优势,可最大限度地减少患者心理负担,避免医患纠纷的发生。
微创技术;妇科手术;输尿管损伤
女性生殖系统与输尿管位置毗邻。在女性生殖系统相关手术治疗时可能会因解剖变异、术中操作不当或术者经验不足等造成输尿管不同程度的损伤。既往对于输尿管损伤后保守治疗失败的患者多采用开放二次手术,该类手术创伤较大、术后恢复时间长。短期内连续手术易引起患者及家属的不满,容易导致医患纠纷。近年来输尿管损伤治疗已逐步从开放修复手术到微创治疗,如输尿管支架置入术、腹腔镜下支架置入修补术、腹腔镜输尿管断端再吻合术以及输尿管膀胱再植术[1]。本研究回顾性分析2008年1月~2016年6月我院妇科手术发生输尿管损伤并行微创技术治疗的33例患者临床资料,现将结果报告如下。
1 资料与方法
1.1 临床资料
本组患者33例,年龄20~69岁,平均45岁。腹腔镜恶性肿瘤手术15例,腹腔镜辅助阴式全子宫切除术8例,腹腔镜子宫肌瘤切除6例,腹腔镜附件切除术4例,患者基本资料见表1。其中5例患者因输尿管走行区有淡红色不明液体渗出,或腹腔镜观察输尿管肌层明显缺损而确诊。术后发现输尿管损伤28例中有1例为孤立肾患者,术后8 h发现腹腔引流量异常增多,而尿量<80 ml,检测腹腔引流液肌酐达5 773 μmol/L,行输尿管镜检查,发现输尿管下段破口。其余27例均在术后7~35 d发现阴道残端有不明液体异常漏出,检测液体肌酐达1 147~8 952 μmol/L,静脉尿路造影检查显示一侧肾轻度积水,输尿管下段梗阻伴尿外渗(图1、2)。
1.2 手术方法
术中发现输尿管损伤5例行腹腔镜或膀胱镜下置入双J管,输尿管全层损伤或浆肌层损伤明显者腹腔镜下4-0可吸收线间断缝合。如输尿管损伤严重,裁剪切除损伤段输尿管,行输尿管端端吻合。术后发现输尿管损伤28例中的1例孤立肾患者,输尿管镜检查发现输尿管下段破口,输尿管内置入双J管后腹腔镜下输尿管破损处间断缝合;其余先行输尿管镜直视下置双J管,置管成功16例,留置双J管2~3个月,另外11例输尿管镜下置双J管失败患者行腹腔镜探查。腹盆腔术野多粘连严重,用剪刀锐性加钝性分离粘连,避免损伤肠管和髂血管。于损伤部位以上离断输尿管,残端用4-0可吸收线缝扎。游离对侧膀胱壁,膀胱向患侧牵引,如输尿管长度足以与膀胱吻合,输尿管插入膀胱10 mm,输尿管膀胱直接吻合。如损伤位置稍高,游离裁剪膀胱壁瓣并缝合成管状与输尿管吻合。置入双J管引流,保留导尿。
2 结果
33名患者手术顺利,2例输尿管膀胱再植患者术后反复出现尿路感染,经正规抗感染治疗治愈。16例术后延迟发现输尿管损伤并成功置入双J管中有1例患者长期漏尿,3个月后再行腹腔镜手术成功,其余膀胱镜下拔除双J管无漏尿发生。11例置管失败患者行均一期行腹腔镜修复术。其中行腹腔镜输尿管膀胱再植9例,膀胱瓣输尿管吻合2例。手术耗时110~160 min,平均132 min。术后住院5~8 d,平均6 d。保留导尿3~4周,术后4~8周膀胱镜直视下拔除双J管。输尿管损伤术后3~6个月复查B超提示轻度肾积水。在以后3~24个月随访中患者无漏尿、中重度肾积水、输尿管狭窄等情况发生。

图1 左输尿管下段造影剂外溢伴左肾轻度积水

图2 右输尿管下段造影剂外溢
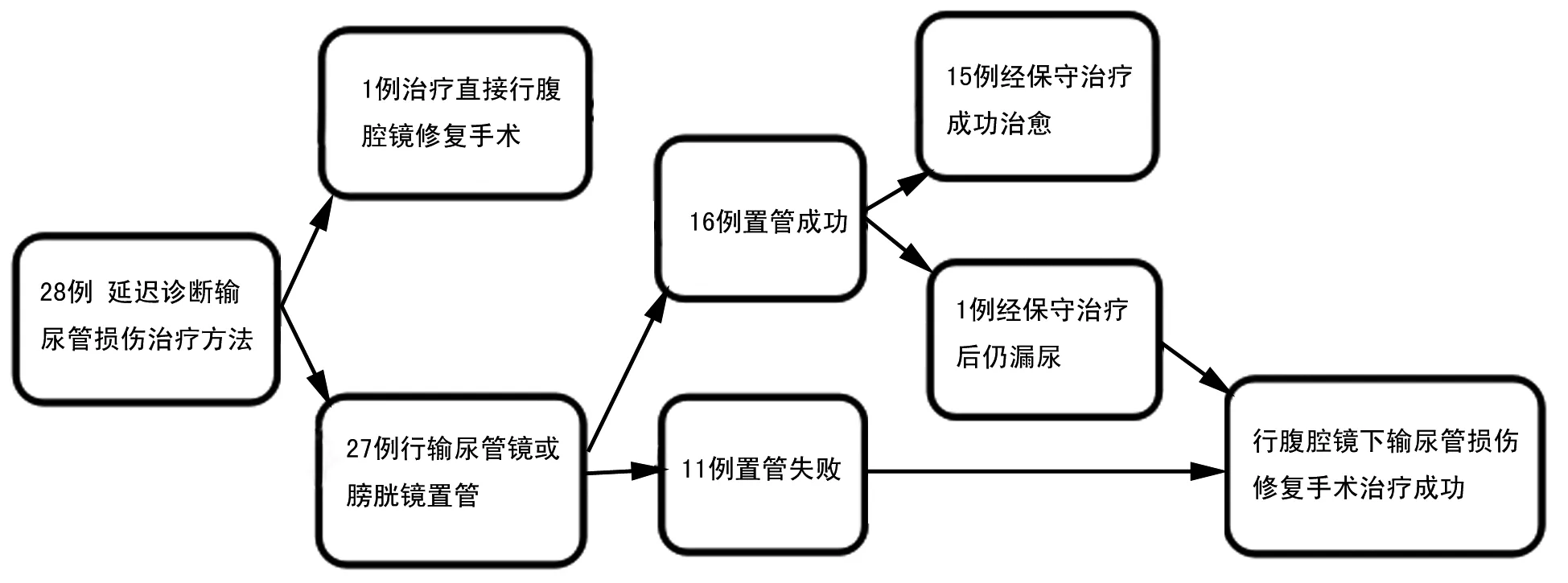
图3 28例延迟发现输尿管损伤患者治疗流转示意图
3 讨论
输尿管损伤是一种少见手术并发症,然而据估计,52%~82%的医源性输尿管损伤发生在妇科手术中[2]。近年随着妇科腹腔镜技术应用越来越广泛,手术适应证和手术范围不断扩大,术中误损输尿管也有增多的趋势。据统计,因妇科腹腔镜手术导致输尿管损伤发病率为0.03%~0.13%,而在复杂手术中输尿管损伤率高达0.2%~1.6%[3]。本组中输尿管损伤发病率为0.18%(33/18 334),与文献[3]类似。医源性输尿管损伤如能术中发现应立即修补,保障输尿管通畅,避免严重情况发生。然而不幸的是,50%~70%的输尿管损伤在术中并没有及时发现[4]。本组中28例(84.84%)输尿管损伤术后确诊,高于文献报道。可能与腹腔镜手术中能量器械的运用导致热损伤难以发现有关。目前对于延迟诊断的输尿管损伤处理尚有分歧。提倡分期手术者认为分期手术可减轻输尿管局部血肿、炎性反应和水肿,有利于手术修复成功,减少围手术期并发症。也有学者认为2周内确诊输尿管损伤可予以即时手术修复,可使住院时间缩短,漏尿、伤口感染等手术并发症减少,也可减轻患者在等待修复期间许多心理压力和精神创伤[5]。
近年来微创治疗输尿管损伤已越来越多的报道,治疗已逐步从开放修复手术到微创治疗,如输尿管支架置入术、腹腔镜下支架植入修补术、腹腔镜输尿管断端再吻合术以及远端输尿管膀胱再植术[1],其治疗的可行性、安全性及有效性也得到更多的证实。Rajamaheswari等[6]报道输尿管损伤案例中输尿管支架置入术成功率可高达76 %(13/17),经保守治疗拔出双J管平均随访24.6个月中无漏尿等并发症的发生。Kumar等[7]报道84例输尿管损伤,输尿管支架通过率仅仅9%(8/84),术后也取得较满意的治疗效果。本组延迟诊断的输尿管损伤中仅有16例(57.14%)双J管成功置入,遗憾的是有1例患者长期漏尿,后行腹腔镜治疗。我们建议最好在输尿管镜直视下置双J管,一方面可避免盲目置管导致输尿管损伤加重,同时可以评估输尿管损伤的程度。如果损伤缺损严重,可一期行腹腔镜修复。置双J管治疗,无再次手术切口创伤,患者痛苦小,费用低,心理上也更易接受。
置双J管失败行输尿管端端吻合或远端输尿管膀胱再植术时,腹腔镜具有微创以及放大作用的优势,使得在操作过程中更加精细。另外,腹腔镜更易在腹膜后较深且有限的空间进行手术修复。有学者报道腹腔镜输尿管端端吻合术的成功率为88.24%~100%[8, 9]。本组术中发现的5例输尿管损伤患者行腹腔镜输尿管修补或端端吻合术均取得手术成功。我们在所有的患者随访中并未出现输尿管狭窄。但随访时间尚较短。Rassweiler等[10]指出,相对于开放手术,腹腔镜输尿管膀胱再植术具有术后痛苦小,住院时间短,康复快等优势。Pal等[11]提出虽然传统输尿管重建术是输尿管下段梗阻的治疗标准,但腹腔镜下输尿管膀胱再植在技术上的优势,逐渐成为治疗输尿管下段梗阻一个可行性选择。本组输尿管阴道瘘11例患者行腹腔镜探查,术中局部炎症反应粘连比较严重,游离输尿管损伤部位及其远端比较困难,我们选择腹腔镜下输尿管与膀胱吻合术。如输尿管损伤位置较高,游离膀胱瓣并缝合形成管状再与输尿管吻合。手术的难点在于是二次手术,腹腔及手术术野粘连严重。既要保证输尿管膀胱充分游离,又必须避免副损伤发生,特别是避免肠管损伤、肠瘘发生等严重的后果。我们的经验是游离过程中尽量采用剪刀冷分离,保证了术野和分离层面的清晰,同时也避免了超声刀、电刀等导致的热损伤。腹腔镜通道应用原妇科腹腔镜手术通道位置,不增加患者损伤,降低了患者的不满。术后平均住院6 d(5~8 d)。随访3~24个月,无漏尿、输尿管狭窄等发生。
输尿管损伤是妇科手术中严重并发症之一,术者一定要提高对输尿管损伤的警惕,减少损伤的发生,卓栋等[12]等报道,术前预置输尿管导管支架有助于术中辨识输尿管,并可预防输尿管损伤。对于已经发生输尿管损伤建议早期处理。部分输尿管损伤患者通过输尿管镜直视下置入双J管行保守治疗,可以达到满意的效果。对于保守治疗失败者行腹腔镜治疗,虽然具有一定挑战,但相比传统手术具有创伤小、术后恢复快、住院时间短等优势,可最大限度的减少患者心理负担,避免医患纠纷的发生。总之,微创治疗输尿管损伤是安全、有效又可行的选择。
[1]De Cicco C, Ussia A, Koninckx PR. Laparoscopic ureteral repair in gynaecological surgery. Curr Opin Obstet Gynecol, 2011,23(4):296-300.
[2]St Lezin MA, Stoller ML. Surgical ureteral injuries. Urology,1991,38(6): 497-506.
[3]Makai G, Isaacson K. Complications of gynecologic laparoscopy.Clin Obstet Gynecol,2009.52(3):401-411.
[4]Ostrzenski A, Radolinski B, Ostrzenska KM. A review of laparoscopic ureteral injury in pelvic surgery. Obstet Gynecol Surv, 2003,58(12):794-799.
[5]Modi P, Goel R, Dodiya S. Laparoscopic ureteroneocystostomy for distal ureteral injuries. Urology, 2005,66(4):751-753.
[6]Rajamaheswari N, Chhikara AB, Seethalakshmi K. Management of ureterovaginal fistulae: an audit. Int Urogynecol J, 2013,24(6):959-962.
[7]Kumar A, Goyal NK, Das SK, et al. Our experience with genitourinary fistulae. Urol Int, 2009,82(4):404-410.
[8]De Cicco C, Schonman R, Craessaerts M, et al. Laparoscopic management of ureteral lesions in gynecology. Fertil Steril, 2009,92(4):1424-1427.
[9]Mereu L, Gagliardi ML, Clarizia R, et al. Laparoscopic management of ureteral endometriosis in case of moderate-severe hydroureteronephrosis. Fertil Steril, 2010,93(1):46-51.
[10]Rassweiler JJ, Gözen AS, Erdogru T, et al. Ureteral reimplantation for management of ureteral strictures: A retrospective comparison of laparoscopic and open techniques. Eur Urol, 2007,51(2):512-522.
[11]Pal DK, Wats V, Ghosh B. Urologic complications following obstetrics and gynecologicai surgery: Our experience in a tertiary care hospital. Urol Ann, 2016,8(1):26-30.
[12]卓栋,杨军文,杨维娟.留置输尿管导管预防妇科手术中输尿管损伤.微创医学,2008,3(3):259-260.
Minimally invasive technique in the treatment of ureteral injury after the gynecologic surgery (A report of 33 cases)
LiMaolin1ZhuoDong1ZhangJing1WangZhiguo1AoPing1
(1Department of Urology, Yijishan Hospital Affiliated to Wannan Medical College, Wuhu 241001, China) Corresponding author: Zhuo Dong, whzhuo2008@sina.com
Objective: To investigate the safety and efficacy of ureteroscope and laparoscopic surgery for the treatment of ureteral injury caused by a gynecological operation. Methods: In the study, 33 cases of ureteral injury in gynecologic operation, with mean age being 45 (20 to 69) years. 5 cases of ureteral injuries were found during the operation and immediate laparoscopic-aided D-J stent insertion was done through ureteral lesion. Repair and suture or end to end anastomosis of ureter was followed. Delayed ureteral injury was found in 28 cases, including 1 case of solitary kidney patients. In this case, abnormal drainage fluid was found 8 hours after operation, the partial lesion of the lower ureter were examined by ureteroscopy, and D-J stent insertion and laparoscopic repair were done. Vaginal stump leakage was found 7 to 35 days after operation in the rest 27 cases. Then cystoscopic-aided or ureteroscopic-aided D-J stent insertion succeeded in 16 cases, and the D-J stent retained for 3 to 2 months. Laparoscopic exploration was done in the other 11 cases of patients with D-J stent insertion failure. Low lesion location, Direct insertion of ureter and bladder was done in the cases of low lesion location. If lesion location was high, free cutting of bladder wall flap and synthesis of tubular in order we do ureteroneocystostomy by free cutting of bladder wall flap and the synthesis of tubular. Results: One of the 16 patients who did successfully D-J stent insertion had long term urinary fistula. This patient recovered after undergoing laparoscopic surgery successfully after 3 months. The 11 cases of patients with D-J stent insertion failure were also healed after one-stage laparoscopic repair. In these cases, operating time was 110-160 min (mean,132 min); ostoperative hospitalization was 5 to 8 days (mean, 6 days); retention catheterization time was 3 to 4 weeks. We removed D-J stent under the cystoscope 4 to 8 weeks after operation. B-us were carried out 3 to 6 months after operation, and mild hydronephrosis was seen in all cases. Conclusions: Ureteral injury caused by gynecological surgery can be cured by inserting the D-J stent. If the conservative treatment failed, patients can be treated by laparoscopy. Although some challenges existed, there are the advantages of safe and effective, less trauma, less scar and faster postoperative recover. And laparoscopy operation can reduce the psychological burden of patients, to avoid the occurrence of medical disputes.
minimally invasive technique; gynaecology surgery; ureteral injury
卓栋,whzhuo2008@sina.com
2017-01-16
R693
A
10.19558/j.cnki.10-1020/r.2017.02.006
论 著
