Vasospastic myocardial infarction: An even rarer occurrence of a rare entity
2017-02-10CemErtanMehmetEmrezpelitnderLimonDenizOrayNihatPekel
Cem Ertan, Mehmet Emre Özpelit, Önder Limon, Deniz Oray, Nihat Pekel
1Department of Emergency Medicine, Izmir University, Izmir, Turkey
2Department of Cardiology, Izmir University, Izmir, Turkey
Vasospastic myocardial infarction: An even rarer occurrence of a rare entity
Cem Ertan1, Mehmet Emre Özpelit2, Önder Limon1, Deniz Oray1, Nihat Pekel2
1Department of Emergency Medicine, Izmir University, Izmir, Turkey
2Department of Cardiology, Izmir University, Izmir, Turkey
INTRODUCTION
Vasospastic angina (VSA) is an important functional cardiac disorder that leads to transient myocardial ischemia and is caused by sudden, intense and reversible coronary artery spasm resulting in subtotal or total occlusion.[1,2]VSA is associated with cardiac conditions such as stable or unstable angina, acute coronary syndromes and lethal arrhythmias. The patients usually present with chest pain, which might or might not be accompanied with ischemic ECG changes.[1,3]Vasospasm is predominantly caused by hyper-reactive vascular smooth muscle cells and probably endothelial dysfunction.[4]It is also reported that prolonged VSA may cause acute myocardial infarction.[2]The prevalence of VSA is known to be as low as 1% to 1.5% of angina admissions.[2]Although the widespread use of calcium channel blockers (CCB) in patients with coronary artery disease (CAD) prevents the occurrence of VSA attacks in susceptible population, 10% to 20% of VSA patients are either resistant or cannot use CCBs due to side effects.[2]Here we report a patient who suffered acute myocardial infarction (AMI) due to documented VSA with no critical coronary lesions.
CASE
A 79-year-old female presented to our emergency department with epigastric pain radiating to her back. She visited gastroenterology with similar pain 10 days ago, hepatic ultrasound and stool blood tests were ordered, which showed no pathologic results. Esophagogastroduodenoscopy was planned for her, but was never performed. The patient also visited the cardiology department 3 days prior to her current ED visit. Coronary angiography (CAG) was performed with high suspicion of coronary artery disease and no critical lesions were determined (plaque formation at left anterior descending post D1 zone and right coronary artery mid-zone).
The patient admitted to our ED due to worsening pain via ambulance. She declared that her pain started suddenly, she felt dizzy and they had to call for an ambulance. Her heart rate was 76 beats/minutes, blood pressure 145/88 mmHg, SpO297 and she had no fever. The ECG of the patient showed ST-segment elevations at leads II, III and aVF along with 0.5–1 mm ST segment elevations and profound negative T waves at V3 to V6 (Figure 1). Cardiology was immediately consulted and acute coronary syndrome (ACS) treatment including heparin 5 000 U IV bolus, morphine sulphate 3 mg IV bolus, ASA 300 mg PO and clopidogrel 600 mg PO was ordered. Thepatient went under emergent CAG. The CAG showed no occluded vessels, but a diffusely constricted vasospastic left anterior descending (LAD) artery (Figure 2A) and right coronary artery (RCA) (Figure 3A). Two milligrams of nitroglycerin was administered as an intravenous bolus and vasospasm resolved instantly (Figure 2B and Figure 3B). The troponin-I level of the patient was found to be 12.67 (0–0.028). The patient was diagnosed as vasospastic myocardial infarction (MI) and discharged 2 days later with calcium channel blockers.

Figure 1. ECG of the patient.
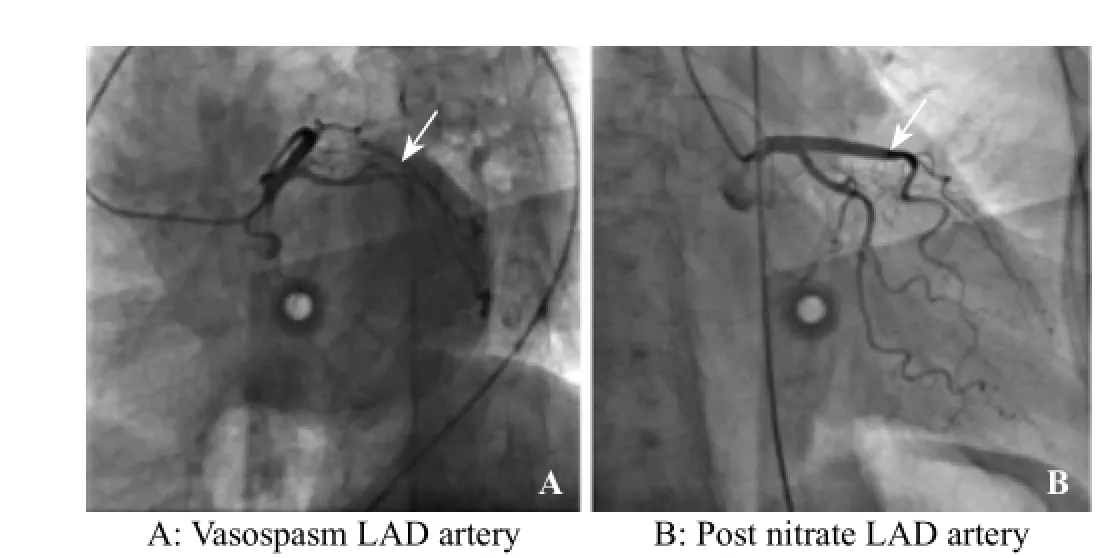
Figure 2. CAG of the left anterior descending (LAD) artery.
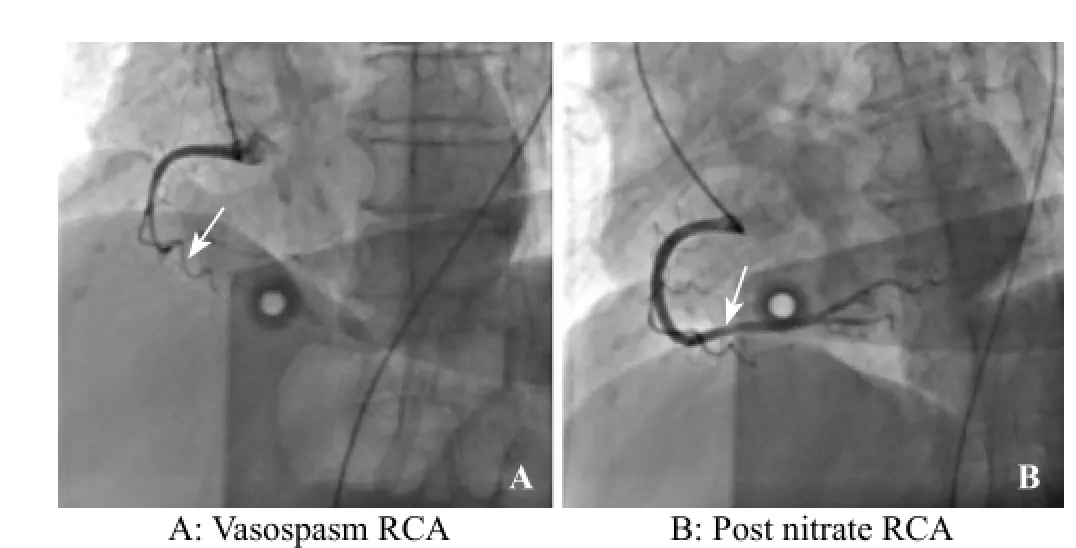
Figure 3. CAG of the right coronary artery (RCA).
DISCUSSION
Coronary artery spasm (CAS) is defined as an intense and reversible vasoconstriction of a coronary artery branch which results in sudden subtotal or total occlusion.[2]The coronary segments may either be stenotic or angiographically normal. CAS may also be focal or diffuse, and it can involve a single or multiple epicardial coronary arteries.[2]CAS is predominantly caused by hyper-reactive vascular smooth muscle cells and probably endothelial dysfunction.[5]The prevalence of VSA is known to be as low as 1% to 1.5% of angina admissions.[6]
It is also reported that prolonged VSA may cause acute MI.[7]Our patient, who suffered chest pain attacks for about ten days, most probably had multiple acutemyocardial infarction episodes based on Troponin-I levels. Her last episode was also documented by an ECG. The fact that her coronary arteries showed no critical obstructive lesions and instant resolution of the spasm following the nitroglycerin bolus supported the vasospastic MI diagnoses.

Table 1. The JCSA Risk Scoring System, consisting of 7 predictors of major adverse cardiac events (MACE)
Several prognostic factors have been established for VSA, including smoking, organic coronary stenosis, multivessel spasm and recently more suggested such as out of hospital cardiac arrest (OHCA), beta blocker use, ST-segment elevation and angina pectoris at rest.[1,8]A risk stratification and prognostic prediction score was proposed by Japanese Coronary Spasm Association (JCSA) (Table 1).[1]Our patient who had no prior OHCA, was not a smoker, and was not under beta blockers, but had angina at rest, had vessel spasms at RCA and LAD, had significant organic stenosis at CAG and had ST elevations in her ECG at the ED with a score of 7 points. This score places her in the high risk strata based on her JCSA risk score and corresponding risk of major adverse cardiac events (MACE).[1]
CONCLUSION
We suggest that, the emergency physicians should be aware of the fact that a recent history of a normal CAG is not solely suff cient to rule out ACS in the ED.
Funding:None.
Ethical approval:Not needed.
Conflicts of interest:The authors declare there is no competing interest related to the study, authors, other individuals or organizations.
Contributors:Ertan C proposed the study and wrote the first draft. All authors read and approved the f nal version of the paper.
REFERENCES
1 Takagi Y, Takahashi J, Yasuda S, Miyata S, Tsunoda R, Ogata Y, et al. Prognostic stratification of patients with vasospasticangina: a comprehensive clinical risk score developed by the Japanese Coronary Spasm Association. J Am Coll Cardiol. 2013;62(13):1144–53.
2 Crea F, Lanza GA. New light on a forgotten disease: vasospastic angina. J Am Coll Cardiol. 2011;58(12):1238–40.
3 Kim MC, Ahn Y, Park KH, Sim DS, Yoon NS, Yoon HJ, et al. Clinical outcomes of low-dose aspirin administration in patients with variant angina pectoris. Int J Cardiol. 2013;167(5): 2333–4.
4 Lanza GA, Careri G, Crea F. Mechanisms of coronary artery spasm. Circulation. 2011;124(16):1774–82.
5 The Task Force on the management of stable coronary artery disease of the European Society of Cardiology. 2013 ESC guidelines on the management of stable coronary artery disease—addenda. Eur Heart J. 2013;34(38):2949–3003.
6 Lanza GA, Sestito A, Sgueglia GA, Infusino F, Manolf M, Crea F, et al. Current clinical features, diagnostic assessment and prognostic determinants of patients with variant angina. Int J Cardiol. 2007;118(1):41–7.
7 Lanza GA, Crea F. Pathophysiology and assessment of coronary spasm. In: Escaned J, Serruys PW, editors. Coronary Stenosis: Imaging, Structure and Physiology. New York, NY: Europa Editions, 2010: 415–430.
8 Takagi Y, Yasuda S, Tsunoda R, Ogata Y, Seki A, Sumiyoshi T, et al. Clinical characteristics and long-term prognosis of vasospastic angina patients who survived out-of-hospital cardiac arrest: multicenter registry study of the Japanese Coronary Spasm Association. Circ Arrhythm Electrophysiol. 2011;4(3):295–302.
Received March 30, 2016
Accepted after revision August 6, 2016
Cem Ertan, Email: cem_ertan@hotmail.com
World J Emerg Med 2017;8(1):68–70
10.5847/wjem.j.1920–8642.2017.01.013
杂志排行
World journal of emergency medicine的其它文章
- Information for Readers
- World Journal of Emergency Medicine
- Instructions for Authors
- An unusual cause of simultaneous bilateral spontaneous pneumothorax
- An unusual emergency department case: ruptured ectopic pregnancy presenting as chest pain
- Toxoplasma encephalitis and AIDS in a patient with seizure and altered mental status: A case report
