Hepatitis B Virus S Promoter Deletion in Hepatocellular Carcinoma
2016-12-07SuzhenJiangJiajiaZhengXiangMeiChenTingZhangQiangXuHuiZhuangFengminLu
Su-zhen Jiang, Jia-jia Zheng, Xiang-Mei Chen,Ting Zhang, Qiang Xu, Hui Zhuang, Feng-min Lu
Original Article
Hepatitis B Virus S Promoter Deletion in Hepatocellular Carcinoma
Su-zhen Jiang1,2, Jia-jia Zheng1, Xiang-Mei Chen1,Ting Zhang1, Qiang Xu1, Hui Zhuang1, Feng-min Lu1
Hepatitis B virus (HBV); S promoter deletion; ER stress; Hepatocellular carcinoma(HCC)
Hepatitis B virus (HBV) is a hepatotrophic virus that causes acute and chronic liver diseases. China is an intermediate endemic area with HBsAg prevalence of 7.18% in the general population,1 where the chronic HBV infection is believed to be usually acquired prenatally, or in early childhood.2 Chronic HBV infection is recognized as an important risk factor for hepatocellular carcinoma (HCC).3 It has been estimated that more than 90% of HCC is etiologically associated with HBV in China.4
HBV contains four open reading frames (ORFs), encoding the surface proteins, the core antigen and e antigen, the polymerase and the HBx protein. Te surface antigens are encoded by the pre-S/S (pre-surface/surface) region of the genome containing a single S-ORF with three in-frame start codons which are responsible for large (L), medium (M) and small (S) surface proteins. Te pre-S/S region is transcriptionally controlled by two separate promoters, pre-S1 and S promoter. Pre-S1 drives 2.4kb mRNA encoding L, M and S surface proteins, while S drives 2.1kb mRNA encoding only M and S surface proteins.
In this study, we compared dif f erent types of HBV pre-S region mutations in paired tumor and non-tumor tissues to confirm if there were specific types of pre-S mutations that were dominant in tumor tissues, and furthermore, to elucidate the direct oncogenic evidence of pre-S mutation.
MATERIALS AND METHODS
Patients
A total of 34 HCC patients (HBsAg positive) were recruited from the Henan Cancer Hospital (the patient's age ranged from 30 years to 70 years; mean = 50.94±8.00 years). None of the patients had undergone interferon therapy or antiviral treatment. All tissue samples were collected from 2006 to 2008 and stored at -70°C. All cases of HCC diagnosed were confirmed at the corresponding hospital using the criteria set by the European Association for the Study of the Liver (EASL).25 Te pathological diagnosis of HCC and corresponding non-tumor tissue was determined according to the WHO classification.Te patients enrolled in this study fulfilled the following criteria: hepatitis B surface antigen (HBsAg)-positive by enzyme immunoassay (EIA, Abbot Laboratories, Abbot Park, IL, USA); all were negative for antibodies against hepatitis C virus (HCV) (EIA, Abbot Laboratories); autoimmune liver disease, drug-related hepa-titis, alcoholic hepatitis and obstructive jaundice were excluded. Tis study was approved by the Ethics Commitee of Peking University Health Science Center, and an informed consent was obtained from each patient.
Sample preparation and detection of pre-S mutations
Genomic DNA was extracted from snap frozen HCC tumor tissues and corresponding non-tumor liver tissues using proteinase K followed by the standard phenol/chloroform extraction and ethanol precipitation method.
Te pre-S region was amplified by nested Polymerase chain reaction (PCR). External primers were SL1 (5'-TCTGGGAACAAGATCTACAGC-3', nt 2,803-2,822) and SL2 (5'-CCCCAACTTCCAATTACATATCC-3', nt 902-880). Internal primers were P1(5'-TCACCATATCTGGGAACAAGA-3', nt 2,823-2,845) and S4R (5'-AGAAGATGAGGCATAGCAGC-3', nt 436-417).
Sequence analysis and genotyping
Nucleotide sequences were compared with the HBV DNA sequences of wild-type genotype 'C' registered in GenBank (NCBI),AY123424.1. Te nucleotide sequences were determined by the NCBI HBV Genotyping Tool (htp://www.ncbi.nlm.nih.gov/projects/genotyping/formpage.cgi).
In vitro expression and secretion of the cloned pre-S mutants in Huh-7 cell line
Site-directed mutagenesis and plasmid construction
Te HBV DNA sequence (2423-3215/1-1969) was amplified from pZAC-1.2×HBV plasmid (Genotype C, GenBank AY123424.1).Te PCR product was inserted into plasmid pGL3-Basic which lacks eukaryotic promoter and enhancer sequences, named as pGL3-preS/Swt. Meanwhile, pGL3-preS/SΔsp with nt 3020-3202 deletion (Genbank AY123424.1) was constructed. All constructs were confirmed by sequencing.
Cell lines and transfection
Te human hepatoma cell lines HepG2 and Huh-7 were used for in vitro cell culture studies. Te cells were maintained in regular Dulbecco's modified Eagle medium (DMEM) supplemented with 10% fetal bovine serum (Gibco BRL, GrandIsland, NY). Te cells were grown at 37℃ with 5% CO2. Plasmid DNA transfection was carried out by the liposome induction method (Lipofectamine 2000,Invitrogen, USA) according to the manufacturer' s instruction.
Detection of HBV surface proteins in culture supernatants and cell lysate of transfected cells
Te HepG2 cells were transiently transfected with pGL3-preS/Swt, pGL-preS/SΔsp, and pGL3-Basic plasmid. Te supernatants were collected 48 hours after transfection and cell debris in the medium was removed by centrifugation. Quantitative HBsAg was studied by automated chemiluminescent microparticle immunoassay (Architect HBsAg, Abbot, IL). Cells were lysed through repeated freezing and thawing in RIPA lysate buf f er (Beyotime, Beijing) and the lysates were harvested. Total of 60 μg total proteins were resolved on SDS-polyacrylamide gels and transferred to polyvinylidene difluoride (PVDF) membranes. Te membrane was incubated with the antibody conjugated with horseradish peroxidase. Te proteins were detected by using ECL chemiluminescence kit (Promega,USA). Te antibody used for Western blot was the polyclonal antibody against all three HBV surface antigens including the large, middle and small HBsAg (Keyuezhongkai, Beijing).
For the GRP78 and GAPDH, the amplifications consisted of 10 min at 95℃ followed by 35 cycles, each consisting of denaturing for 10 s at 95℃, annealing for 10 s at 60℃, and elongation for 10 s at 72℃. Amplifications were performed in triplicate in LightCycler 480 real-time PCR instrument. Negative controls containing non human cDNA template were included for each gene within each PCR run. Amplification specificity for each gene was confirmed by a single distinct melting curve. PCR products were separated using 1.5%agarose gel electrophoresis to confirm the presence of a single band at the expected amplicon size.
Statistical analysis
All statistical analyses were performed using the Statistical Analysis System (SAS 8.2). Associations in 2×2 tables were evaluated with Fisher's exact test. Te comparison between categorical variables was tested by the chi-square test. All tests were 2-sided and a P value less than 0.05 was considered to be statistically significant.
RESULTS
Demographical and clinical data of HCC patients
Te demographic, disease and virological clinical data of 34 patients with HCC are given in Table 1a and 1b. Te mean serum alanine transaminase (ALT) level was 49.25±20.30 U/ml, and the percentage of positive anti-HBe was 60.61% (20/33) in these patients. Tissue DNAs from 25 paired HCC tumor and non-tumor samples and 9 HCC tumor samples were amplified for HBV pre-S/S region. Phy-logenetic analysis and subgenotype-specific analysis revealed that among 34 HBV-infected HCC patients, the proportions of genotype C2 and C2/Ba were 97.06% (33/34) and 2.94% (1/34), respectively. Te HBV C2/Ba strains were detected in patient with HCC-11 tumor tissue.
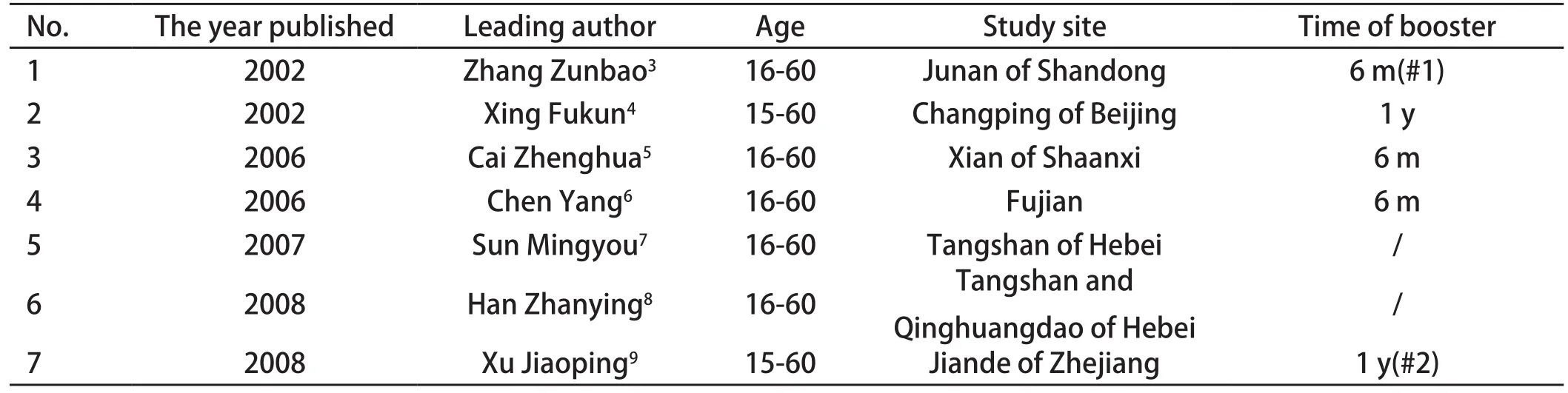
Table 1. Characteristics of eligible articles on HFRS bivalent vaccine effectiveness
Detection and location of pre-S mutation in tumor and non-tumor tissue
Four types of pre-S region mutations were found: pre-S1 start codon in-frame deletion (ranging from the first amino acid to the 11st amino acid) (type I), pre-S2 in-frame deletion (type II), pre-S2 start codon mutation with or without pre-S2 in-frame deletion (type III), and S promoter region in-frame deletion (type IV) (Figure 1).
Te distribution of pre-S mutations in tumor and non-tumor liver tissue was illustrated in table 1. Te 4 types of pre-S deletions were all in-frame deletions according to our sequencing data. Te overall percentages of pre-S mutation were 44.12% (15/34) in tumor tissue and 48.00% (12/25) in non-tumor tissue separately.
Te rates of all the mutant types did not dif f er significantly between tumor tissue and non-tumor tissue (P > 0.05) (Table 2). However, the frequency of type II mutation was higher in non-tumor group as compared to tumor group (40.00% (10/25) vs. 20.59% (7/34)(P = 0.104). Te type IV mutation strains were found to be the dominant population in 17.64% (6/34) tumor tissues. In contrast, only 1 of 25 non-tumor tissues was positive for the mutation, and it was present non-dominantly.
Mutant and wild type HBV strains coexisted in most of the samples tested. It is important to notice that viruses harboring type I and II mutations were not dominant in viral population (Table 1). In contrast, the type III and IV mutant strains were dominant in tumor tissues. Moreover, the type IV mutant in tumor tissues was present as the dominant or sole strain in viral population according to the DNA electropherogram.
ER stress signal gene GRP78 induced by the S promoter mutants
Te protein encoded by GRP78 is localized in the lumen of the endoplasmic reticulum (ER), and is involved in the folding and assembly of proteins in the ER. Te expression of GRP78 and GAPDH was detected in cells transiently transfected with the pGL3-Basic, pGL3-preS/Swt and pGL3-preS/SΔsp for 48 h. As compared with pGL3-Basic, the WT showed slightly enhanced expression of GRP78 (average = 1.46 folds) while the ΔSP mutant showed an obvious, enhanced expression level of GRP78 (average = 6.44 folds)(Figure 6).
DISCUSSION
Previous studies by our lab and others showed that HCC patients with chronic HBV infection had a higher prevalence of HBV with pre-S deletions than chronic HBV infected patients without HCC.6,8,26,27 Indeed, HBV pre-S2 deletions have been suggested as an independent factor associated with the development of HCC.26 However, the observed association was essentially based on crosssectional or case control studies. Nevertheless, almost all of such studies used serum from the patients as specimens. We still need more direct evidence to link HBV pre-S deletions with hepatocarcinogenesis and in vitro oncogenic characteristics studies of pre-S mutations,in order to determine their roles at the molecular mechanistic level. In this study, we analyzed HBV pre-S mutations in paired tumor and the corresponding adjacent non-tumor tissue specimens.
Firstly, our data indicated that all deletions in pre-S1/S2 region were in-frame deletions. Tus the predicted pre-S1 and/or pre-S2 proteins contained internal deletions, and that the integrity of polymerase ORF was maintained.
Secondly, we found that the pre-S1 start codon in-frame deletion coexisted with the wild-type strain and various mutation strains in both tumor and the non-tumor tissues. Te type I mutation of HBV pre-S region (pre-S1 start codon in-frame deletion) permits synthesis of the large surface protein from the second in-frame methionine codon, resulting in the deletion of the first 11 amino acids of LHBs. Te prevalence of such mutations had no dif f erence between tumor and non-tumor specimens studied (P=1.000). Omission of the first 11 amino acids of LHBs is a distinct characteristic of HBV genotype D. However, nearly all patients studied here were infected with HBV genotype C.
In summary, our study reveals that pre-S mutations, especially pre-S2 deletions are relatively common in liver tumor and nontumor tissues. HBV mutations of S promoter in-frame deletion were found to be dominated in tumor tissues only. Tis type IV mutation abolished both M and S surface protein synthesis, caused excessive production of mutant LHBs, and thus induced ER stress due to its improper intracellular transportation and ER accumulation. Te improper ER retention of mutant LHBs induced ER stress and the subsequent events are believed to be the underlying mechanism for the direct tumorigenic property of type IV pre-S mutation.
Foundations
Tis study was supported by grants from the National Projects on Major Infectious Diseases, Ministry of Science and Technolog of China (No. 2009ZX10004-903), and the Doctoral Fund of Ministry of Education of China ( No.20100001110055).
Acknowledgment
We are very grateful to Jamie L. Trans and Vincent Tse for proofreading the manuscript.
1. Lu FM, Zhuang H. Management of hepatitis B in China. Chin Med J 2009; 122:3-4.
2. Liu CJ, Kao JH. Hepatitis B virus-related hepatocellular carcinoma: epidemiology and pathogenic role of viral factors. J Chin Med Assoc 2007;70: 141-145.
3. Chen CJ, Chen DS. Interaction of hepatitis B virus, chemical carcinogen, and genetic susceptibility: multistage hepatocarcinogenesis with multifactorial etiology. Hepatology 2002;36:1046-1049.
4. McGlynn KA, London WT. The global epidemiology of hepatocellular carcinoma: present and future. Clin Liver Dis 2011;15:223-243.
ObjectiveTo identify the dif f erence and significance of dominant types of hepatitis B virus (HBV) pre-S mutation between liver tumor tissues and paired adjacent non-tumor tissues and to test if the mutations were tumor tissue specific.MethodsHBV DNA isolated from 34 paired intratumoral and peritumoral tissues of Hepatocellular Carcinoma (HCC) patients were screened by PCR and direct sequencing. All patients carried HBV with genotype C, except for one B/C heterozygote. Te expression,localization and excretion of LHBs mutant carrying pre-S deletions were characterized in vitro. Te expression of endoplasmic reticulum (ER) GRP78 mRNA was assayed.ResultsFour paterns of pre-S mutations were identified: pre-S1 in-frame deletion involving the first start codon; pre-S2 in-frame deletion; pre-S2 start codon mutation with or without in-frame deletion; and S promoter in-frame deletion (ΔSP). Te first two types were evenly found in both tumor and non-tumor tissues. Tey were rarely present as dominant strains. Te last two types were frequently found in the dominant strains in tumor tissues. Te overall prevalence of HBV carrying ΔSP was 17.64% (6/34) in tumor tissues, but none were dominant in non-tumor tissues. HBV carrying ΔSP was unable to produce S protein in vitro. Immunocytofluorescence assay showed that the ΔSP LHBs mutant aggregated in the cytoplasm, accumulating mainly in the ER. Transient transfection and expression of ΔSP mutant caused GRP78 up-regulation in vitro.ConclusionHBV S promoter deletion was found dominantly in HCC tumor tissue. Te aggregation of mutant large surface proteins in the ER possibly involved in HBV-related HCC.
杂志排行
国际感染病学(电子版)的其它文章
- Identification of the Disrupted Pathways Associated with Periodontitis Based on Human Pathway Network
- Instructions for Infection International Authors
- Progress inResearch on Vestibular Rehabilitation Therapy
- Advances in Studies on Prevalence and Interaction Mechanism of Acquired Immunodeficiency Syndrome and Tuberculosis Coinfection
- Application of CT Perfusion Imaging Technology in the Diagnosis of Hepatitis and Liver Cirrhosis
- Status and Progress in the Control of Infection in Chinese Hospitals