Influence of immobilization and sensory re-education on the sensory recovery after reconstruction of digital nerves with direct suture or muscle-in-vein conduits
2016-12-02TheodoraManoliJenniferLynnSchieferLukasSchulzThomasFuchsbergerHansEberhardSchaller
Theodora Manoli, Jennifer Lynn Schiefer, Lukas Schulz, Thomas Fuchsberger, Hans-Eberhard Schaller
Department of Hand, Plastic and Reconstructive Surgery, Burn Unit, BG Trauma Center, University of Tuebingen, Tuebingen, Germany
RESEARCH
Influence of immobilization and sensory re-education on the sensory recovery after reconstruction of digital nerves with direct suture or muscle-in-vein conduits
Theodora Manoli*, Jennifer Lynn Schiefer, Lukas Schulz, Thomas Fuchsberger, Hans-Eberhard Schaller
Department of Hand, Plastic and Reconstructive Surgery, Burn Unit, BG Trauma Center, University of Tuebingen, Tuebingen, Germany
The influence of duration of immobilization and postoperative sensory re-education on the final outcome after reconstruction of digital nerves with direct suture or muscle-in-vein conduits was investigated. The final sensory outcome of 35 patients with 41 digital nerve injuries, who either underwent a direct suture (DS) or a nerve reconstruction with muscle-in-vein conduits (MVC), was assessed the earliest 12 months postoperatively using static and moving two-point discrimination as well as Semmes-Weinstein monofilaments. There was no significant difference in sensory recovery in cases with an immobilization of 3-7 days versus 10 days in the DS or MVC group. Moreover, no statistically significant difference in sensory recovery was found in cases receiving postoperative sensory re-education versus those not receiving in the DS or MVC group. An early mobilization does not seem to have a negative impact on the final outcome after digital nerve reconstruction. The effect of sensory re-education after digital nerve reconstruction should be reconsidered.
nerve regeneration; peripheral nerve; digital nerve; sensory re-education; immobilization; digital; direct suture; muscle-in-vein conduits
Accepted: 2015-12-02
Introduction
Digital nerve injuries of the upper limb are very common. After almost a century of research in the field of nerve repair, the microsurgical methods of reconstruction are well described and practiced. It is known that in order to achieve the best possible regeneration after reconstruction of peripheral nerve defects, the surgical technique must provide an optimal milieu for the ingrowth of the new axon sprouts after Wallerian degeneration takes place. In case of a sharp transected nerve, direct suture (DS) of the proximal and distal stumps can be performed if a tensionless coaptation is possible (Dahlin, 2008; Siemionow et al., 2010). In case of gap lesions, muscle-in-vein conduits (MVC) (Geuna et al., 2004; Battiston et al., 2005; Marcoccio et al., 2010; Tos et al., 2012; Manoli et al., 2014) can be used as alternatives to conventional nerve autografts for bridging nerve defects without causing a sensory loss at the harvesting site. Many parameters may influence the final outcome after nerve regeneration is completed, such as different mobility regimes as well as the performance of sensory re-education.
Different postoperative mobility regimes following nerve reconstruction and repair can be found in the literature and are often determined by the involved surgeon or surgical unit in an empirical way (Jabir and Iwuagwu, 2014). Moreover, an additional tendon injury commonly leads to a different postoperative mobility regime from in case of isolated nerve injury. An equivalent outcome regardless of the immobilization regime that varied between free mobilization, protected immobilization and static immobilization for 2 to 4 weeks after nerve repair (Clare et al., 2004; Yu et al., 2004; Vipond et al., 2007; Henry et al., 2012). Lohmeyer et al. (2010) surveyed 35 centers all over Germany specialized on hand surgery on their postoperative mobility regime after digital nerve injuries, injuries of flexor tendons and combined injuries of flexor tendons and digital nerves. Most centers immobilized the injured hand for 10 days after isolated digital nerve injury. After combined injuries of flexor tendons and digital nerves the mean immobilization time was 6 days, followed by a protected mobility regime in 85% cases according to the Kleinert or Washington regime for 6-8 weeks. In our center a static immobilization of 10 days is performed after isolated nerve injury of the hand and a mean static immobilization of 5 days after combined injuries of flexor tendons and digital nerves, followed by a protected mobilization according to the Kleinert regime for 6 weeks.
Little is known about the influence of sensory re-education after digital nerve reconstruction (Oud et al., 2007). Cheng et al. (2001) demonstrated a better recovery of both moving and static two-point discrimination in a group that received a sensory re-education after digital nerve injury distal to the metacarpal joint compared to the control group in a 6-month follow-up examination but no further examination was given on a later time point, when regeneration would be expected to be completed. Other studies demonstrating that sensory re-education minimizes discomfort and improves sensibility have been performed on more proximal lesions of mostly mixed nerves(Parry and Salter, 1976; Imai et al., 1991; Miller et al., 2012). Empirically, it is not clear if there is a significant effect of sensory re-education on the final outcome after digital reconstruction. It can be postulated that a sensory re-education program could be omitted in case of digital nerves, since the hand as a grasping organ is anyways performing a sensory re-education through its normal daily functional use itself.
The aim of this study was to examine the influence of duration of immobilization and postoperative sensory re-education on the final outcome of sensory recovery after digital nerve reconstruction with either direct nerve suture or MVCs.
Patients and Methods
The study was consistent with §15 of the professional code of conduct of physicians in Germany and was approved by the ethics committee of the University of Tuebingen (117/2012BO2).
Patients
Patients treated between 2008 and 2012 in the Department of Hand, Plastic and Reconstructive Surgery at the BG Trauma Center Tuebingen, Germany, with either DS, or reconstruction by MVCs of one or more sensory digital nerves from the level of the metacarpophalangeal joint to the level of the distal interphalangeal joint on the palmar side of the hand, were selected as candidates for the study. Excluded were patients with total or subtotal amputations with a combined injury of blood vessels, nerves, tendons and bones. Patients were then invited to a prospective follow-up examination telephonically or via the earliest 12 months after the operation. Only individuals that understood sufficiently the background of the study and agreed to participate in the follow-up examinations were included in the study. The participants gave their written informed consent before proceeding with the follow-up examination. Parents of patients under 18 years of age provided their informed consent prior to the examination of their children. Two patients that could not understand the background of the study or were not cooperative enough to perform the clinical assessment tests of the follow-up examination adequately had to be excluded from the study.
Altogether 35 patients with 41 injuries of digital nerves treated with direct nerve suture (n = 22) or reconstruction with MVCs (n = 19) participated in the study. Nerve reconstructions, also from the same individuals, have been analyzed as distinct cases (Manoli et al., 2014). The age of patients ranged between 15 and 72 years. The distribution of patients according to their treatment, mean age, primary or secondary reconstruction, gap length, existence of a complete injury of the flexor tendons and performance of a postoperative sensory re-education is depicted in Table 1.
Surgical procedures
DS was performed if a tensionless adaptation of the nerve stumps was possible. MVCs were used for bridging nerve defects if a direct suture was not possible. All direct sutures were performed primarily on the day of injury. Nerve reconstructions by means of MVCs were either performed primarily up to 12 hours after injury or secondarily up to 15 weeks after injury. Secondary reconstructions were performed when the nerve injury was not primarily recognized or when a primary nerve reconstruction was not possible. The length of the bridged nerve gap ranged from 1 to 6 cm. In case of direct nerve suture, both nerve stumps were directly approximated and sutured with 2-3 epineural stitches (10-0 nylon) avoiding tension and torsion of both stumps. In cases with nerve gaps, the autologous MVC was interposed between the two nerve ends. To prepare a MVC, a subcutaneous vein, slightly wider than the damaged nerve, was harvested from the palmar side of the forearm. At the same site, a fascial incision was performed and a thin muscle strip was excised. The muscle was then pulled into the vein along its longitudinal course of fibers using a micro forceps. Then the vein ends were sutured over the nerve tissue including all fascicles with 10-0 nylon (Manoli et al., 2014).
Immobilization regime
The following immobilization regime was applied if the surgeon did not make any modifications e.g., due to postoperative swelling: After sole nerve reconstruction with direct nerve suture (nDS= 9) or MVCs (nMVC= 15), the injured hands were in most cases completely immobilized in a custom plaster forearm splint for 10 days. Afterwards free mobilization was allowed, avoiding pressure, traction and torsion at the injured site for 6 weeks. If one or both flexor tendons had to be sutured additionally (nDS= 13, nMVC= 4), a complete immobilization in a custom plaster forearm splint was performed for 5-7 days followed by a 6-week protected mobilization in a custom-molded thermoplastic Kleinert hand and finger splint, in most cases.
Finally, 12 cases treated with DS and 6 cases treated with MVCs were immobilized completely for 3-7 days, whereas 10 cases treated with DS and 13 cases treated with MVCs were immobilized completely for 10 days.
Sensory re-education
Patients that received a postoperative sensory re-education (nDS= 9, nMVC= 9) underwent the following regime beginning from postoperative week 4: The training started with stroking movements from the level of injury to the distal fingertip using the eraser side of a pencil or/and a toothbrush. It first began under visual control, repeating the same procedure with closed eyes focusing on the sensory perception and afterwards followed by verification of the perception after reopening the eyes. After recovery of this kind of perception, the training was switched to striking movements with light pressure using the same items. The pressure applied in both stroking and striking trainings should be as high as not to cause any pain. After recovery of striking perception was completed, training was completed by exercising the perception of different materials like beans, peas, rice and sand as well as by application of hot and cold materials. For the different steps of the training, patients were instructed by ergotherapists. The patients should perform the exercises 4 times daily for 5 minutes independently, at least 6-12 months after operation. Only patients that performedthe above regime for at least 6 months were included.
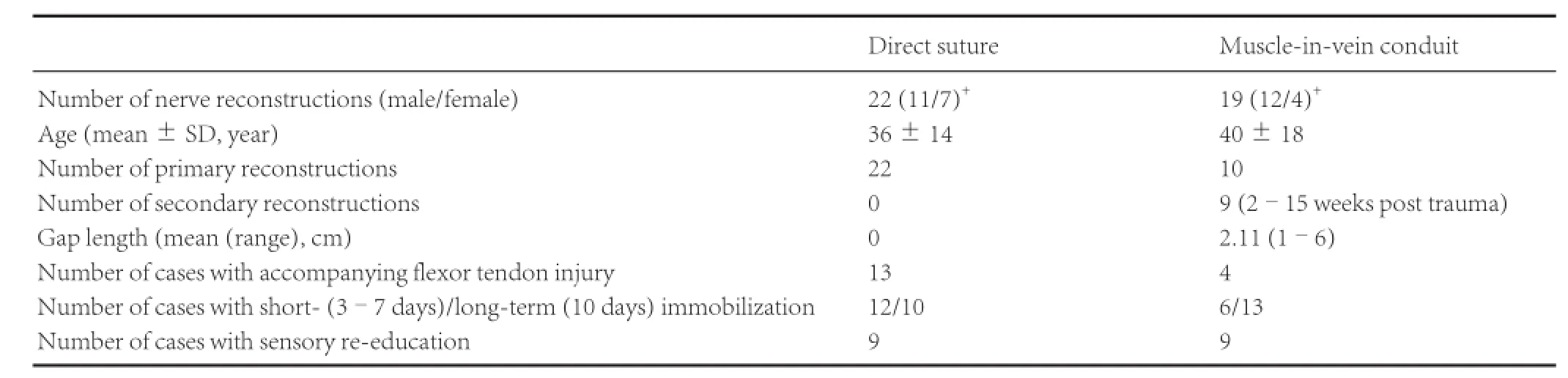
Table 1 Summary of patients within the two groups in terms of mean age, distribution of primary and secondary reconstruction, gap length, existence of an injury of the flexor tendons, duration of immobilization and performance of a postoperative sensory re-education

Figure 2 Influence of duration of immobilization in days (Y-axis) on sensory recovery of injured hands according to Semmes-Weinstein monofilaments (SWM) test.

Figure 1 Flow charts of patient enrolment, treatment, and follow-up for examining the influence of immobilization (A) and sensory re-education (B) on the sensory recovery after reconstruction of digital nerves with direct suture (DS) or muscle-in-vein conduits (MVCs). d: Day(s).
Follow-up examination
All follow-up examinations were performed 12-42 months after nerve repair. Prior to the follow-up examination, information regarding postoperative therapy including the mobilization regime and sensory re-education of the injured digit was collected from the case file and later additionally confirmed by the patients.
During the follow up examination, Homecraft Rolyan® Semmes-Weinstein monofilaments (SWM; Homecraft Rolyan; A Patterson Medical Company, Sutton-in-Ashfield, UK) were used to assess pressure perception on the palmar side of the hand (Barber et al., 2001). The set consisted of 20 monofilaments whereas each monofilament was labeled with the logarithm to base 10 of the pressure force it produces onto the skin. In order to obtain objective results each monofilament was vertically pressed onto the skin until it slightly bended holding it for 1-2 seconds. The examination began always with the 2.83 monofilament followed by the next thicker monofilament until the patient stated a perception with closed eyes. Up to 11 monofilaments (2.83 to 5.18) had to be used to obtain a positive result. The interpretation of sensory recovery according to the monofilament labels was as following: 2.83 (N: normal); 3.22 or 3.61 (DLT: diminished light touch); 3.84, 4.08, 4.17 or 4.31 (DPS: diminished protective sensation); 4.56, 4.74, 4.93, 5.07 or 5.18 (LPS: loss of protective sensation).
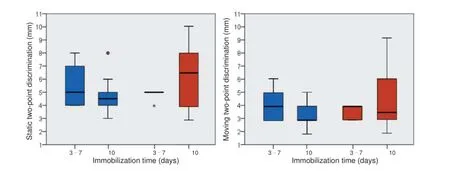
Figure 3 Influence of duration of immobilization on sensory recovery of injured hands according to static (left) and moving (right) two-point discrimination.
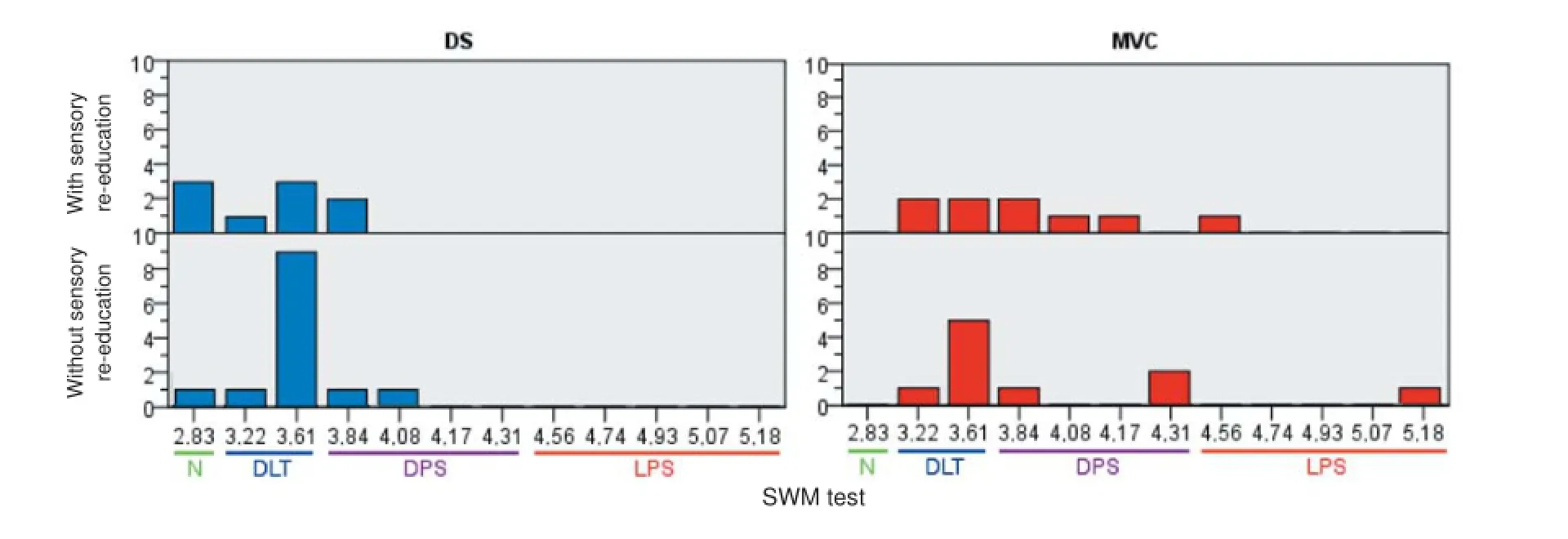
Figure 4 Influence of sensory re-education on sensory recovery of injured hands according to Semmes-Weinstein monofilaments (SWM) test.
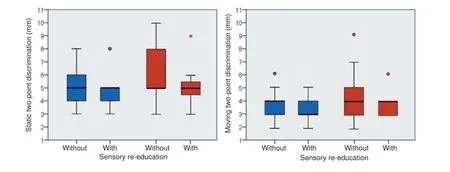
Figure 5 Influence of sensory re-education training on sensory recovery of injured hands according to static (left) and moving (right) two-point discrimination.
Examination of spatial discrimination was assessed with static and moving two-point discrimination (s2PD and m2PD) and carried out with a two-point discriminator (Touch-Test®, North Coast Medical Inc., Gilroy, CA, USA) (Mailander et al., 1989). Testing intervals ranging from 2-15 mm could beassessed. For measuring static two-point discrimination, patients were asked to close their eyes and the examined finger was slightly held from the dorsal side. Then one or two points were applied to the skin for at least 3 seconds. Light pressure was added to the weight of the device carefully until blanching of the skin occurred. The test was applied at the fingertip in line of the anatomical course of the examined sensory digital nerve. Three repetitive responses should be accurate for scoring. Moving two-point discrimination was tested in a similar way. One or both points of the discriminator were applied at the level of the distal interphalangeal joint and were slowly moved distally to the fingertip. The lowest possible pressure was applied, so that the patient could appreciate the stimulus and respond without hesitation. Testing began with 8 mm and stopped at 2 mm (Manoli et al., 2014).
Hereby all clinical tests were performed by the same assessor (LS), who was not involved in the surgical procedure.
Flow charts of patient enrolment, treatment, and follow-up are depicted in Figure 1.
Data analysis
Statistical analysis of the collected data was carried out with R version 3.1.2 and its package “stats” (R Foundation for Statistical Computing, Vienna, Austria). The results of SWM test and static and moving discrimination were evaluated using one-tailed Wilcoxon rank-sum-tests to find out a) whether the short-term immobilization groups would demonstrate worse (higher) values than the long-term immobilization groups and b) whether the groups without sensory re-education would demonstrate worse (higher) values than the groups with sensory re-education, for the cases after direct suture or reconstruction with muscle-in-vein conduits separately. After applying a Bonferroni correction for multiple testing (12 hypotheses tested), the level of significance was set by a P value of < 0.004. IBM SPSS Statistics, Version 21.0 (IBM Corp, Armonk, NY, USA) was used for graphical data analysis.
Results
Effects of immobilization time on sensory recovery
12 cases treated with DS were immobilized completely for 3-7 days and 10 cases for 10 days (Figure 2). Two of the 12 cases (17%) immobilized for 3-7 days achieved a recovery to normal levels according to SWM test, 9 (75%) demonstrated a DLT and 1 (8%) a DPS. 2 of the 10 cases (20%) immobilized for 10 days had a recovery to normal levels, 5 (50%) demonstrated a DLT and 3 (30%) a DPS. No statistically significant differences between the cases with an immobilization of 3-7 days or 10 days in the DS group could be found (PSWM= 0.72). Six cases treated with MVCs were immobilized completely for 3-7 days and 13 for 10 days. Three of the 6 cases (50%) immobilized for 3-7 days demonstrated a DLT and the other 3 (50%) a DPS. Seven of the 13 cases (54%) immobilized for 10 days demonstrated a DLT, 4 (31%) a DPS and 2 (15%) a LPS. No statistically significant differences between the cases with an immobilization of 3-7 days or 10 days in the MVC group could be found (PSWM= 0.48).
The results of static and moving two-point discrimination are depicted in Figure 3. No statistically significant differences between the cases with an immobilization of 3-7 days or 10 days could be found in the DS group (Ps2PD= 0.10, Pm2PD= 0.02) or MVC group (Ps2PD= 0.97, Pm2PD= 0.93) for both static and moving discriminations.
Effects of sensory re-education on sensory recovery
Altogether 9 cases treated with DS and 9 treated with MVCs received postoperative sensory re-education training (Figure 4). Three of 9 cases (33%) treated with DS achieved a sensory recovery to normal levels according to SWM test, 4 (44%) demonstrated a DLT and 2 (22%) a DPS. From the 13 cases of DS group that received no sensory re-education training at all, 1 (8%) achieved a sensory recovery to normal levels, 10 (77%) demonstrated a DLT and 2 (66%) a DPS. No statistically significant differences between the cases with or without sensory re-education training in the DS group could be found (PSWM= 0.18). Four of 9 (44%) cases treated with MVCs and receiving a postoperative sensory re-education training demonstrated a DLT, 4 (44%) a DPS and 1 (11%) a LPS. Six of 10 cases (60%) treated with MVCs and receiving no postoperative sensory re-education training demonstrated a DLT, 3 (30%) a DPS and 1 (10%) a LPS. No statistically significant differences between the cases with or without sensory re-education training in the MVC group were identified (PSWM= 0.48).
The results of static and moving two-point discrimination are depicted in Figure 5. No statistically significant differences between the cases with or without sensory re-education training could be found in the DS group (Ps2PD= 0.57, Pm2PD= 0.32) or MVC group (Ps2PD= 0.42, Pm2PD= 0.47) for both static and moving discriminations.
Discussion
Many researchers have focused on peripheral nerve regeneration after injury and tried to raise the functional outcome on different ways (Millesi, 1985; Mailander et al., 1989; Siemionow and Brzezicki, 2009). Despite the many different microsurgical methods of repair, most of them are well described and practiced, especially the nerve suture and the nerve autografting. A more recently described method is the reconstruction with MVCs (Battiston et al., 2000; Geuna et al., 2004), which has also achieved comparable postoperative results as nerve autografting after reconstruction of digital nerves (Manoli et al., 2014). However, the focus of the previous studies was not mostly set on co-existing factors that may influence the outcome of nerve regeneration like duration of postoperative immobilization and performance of sensory re-education training. Therefore, the influence of these two factors was investigated after DS or reconstruction with MVC of digital nerves of the hand in the current study.
Duration of immobilization
The recent immobilization regimes after peripheral nerve injuries are rather shorter compared to older regimes. Especially in case of digital nerve injuries, a prolonged immobilization of the hand may yield to a persistent stiffness associated with a functional loss and a delayed return to work (Clare et al.,2004). Chao et al. (2001) showed in a fresh cadaver study on human digital nerves that an immediate postoperative passive mobilization after tension free nerve coaptation or reconstruction with nerve autografting did not lead to nerve disruption. It was suggested that tendon mobilization protocols might still be performed after combined nerve injury followed by a tension free nerve coaptation to avoid poor tendon gliding or hand stiffness due to immobilization (Chao et al., 2001). A systematic literature review including four studies with 138 patients by Jabir and Iwuagwu (2014) evaluating mobilization regimes after nerve repair of the digit yielded an equivalent outcome regardless of the immobilization regime after nerve repair. In detail, Clare et al. (2004) compared splinting for 1-2 days with complete immobilization for 2 weeks after digital nerve repair. Vipond et al. (2007) compared debunked dressing for 4 days with splinting for 3 weeks. Henry et al. (2012) compared protected active mobilization over 4 weeks with complete immobilization over the same time and Yu et al. (2004) compared complete immobilization for about 4 days and about 3 weeks after nerve repair.
Our data underlines the idea that fast mobilization does not have a negative impact on the outcome of digital nerve regeneration. Following direct suture, 92% of the cases after early mobilization (3-7 days) and 70% after immobilization for 10 days demonstrated very good to good results according to SWM test (N or DLT). Following reconstruction with MVCs, 50% of the cases after fast mobilization (3-7 days) and 58% after immobilization for 10 days demonstrated very good results (DLT). No statistically significant differences between cases treated with early or later immobilization could be demonstrated after both DS and reconstruction with MVCs according to both SWM-test and two-point discrimination in the current study, using sensitive one-tailed statistics. Therefore, the assumption that an immobilization for at least 10 days would protect nerve sutures from any tears yielding to dehiscence of nerve stumps is not validated.
Postoperative sensory re-education
Wynn-Parry and Salter (1976) published the first sensory-recovery program in 1966 (Parry and Salter, 1976). Since then many research groups have worked on explaining its effect and improving the training (Dellon and Jabaley, 1982; Daniele and Aguado, 2003). A systematic literature review reported limited evidence for the effectiveness of sensory re-education after peripheral nerve injury of the upper limb in general (Oud et al., 2007). Most of the studies included in this evaluation were reported about more proximal lesions of mixed nerves of the upper extremity than with digital sensory nerves (Parry and Salter, 1976; Imai et al., 1991).
In a recent review, a limited evidence to support the use of early and late sensory re-education programs was reported. Also in this case only mixed nerves were included in the analysis. These results are not comparable to the ones after digital nerve repair, since the problem of non-selective reinnervation is not major in case of pure sensory nerves (Miller et al., 2012).
Only the randomized clinical trial of Cheng et al. (2001) dealt with the effect of sensory re-education after digital nerve repair, including 24 cases treated with and 25 cases treated without tactile stimulation performed for 3 weeks to 4.5 months, beginning 3 weeks after operation. They found a significantly better recovery of the two-point discrimination but not of the cutaneous pressure threshold 6 months after digital nerve repair in the first group compared to the control group. However, no late follow-up examination at least 12 months after nerve injury, when nerve regeneration would be expected to be completed, was performed (Cheng et al., 2001). In the rat model for instance, the number of axons distal to a repair increases dramatically up to 3 months, followed by a plateaus from 6 to 9 months, and returns to about normal levels after 2 years (Mackinnon et al., 1991). It is unclear, whether employing the injured hand as a grasping organ in daily routine does not have a similar effect like digital sensory re-education training itself in healthy humans, so that this might be redundant in case of isolated lesions of digital nerves. Our data yielded no significant differences in sensory recovery of the digits assessed by the SWM-test (which measures cutaneous pressure) and the two-point discrimination due to sensory re-education for both DS and reconstruction with MVCs.
Symptoms of sensory disturbance after digital nerve repair usually include subjective findings as numbness, temperature dysregulation, pain, hypersensitivity and tingling, but no examination methods exist that simultaneously evaluate all these sensations together. The SWM-test and two-point discrimination were chosen as relatively reliable methods to assess sensory recovery. Both methods have, however, some limitations that have to be taken into consideration. They are influenced for example by body temperature, skin thickness and subjective factors related to both the examiner and the patient.
Conclusion
A fast mobilization after 3-7 days compared to an immobilization for 10 days did not seem to have a negative impact on nerve regeneration. The need of a sensory re-education after digital nerve reconstruction should be reconsidered.
Author contributions: TM was responsible for conception and design of this research, performed clinical studies, was in charge of data analysis and paper preparation and review, and was a guarantor of the paper. JLS designed this study, performed literature searches, conducted clinical studies, and also participated in data analysis and paper preparation. LS participated in design of this research, performed literature searches, conducted clinical studies, was responsible for data acquisition and paper editing. TF performed clinical studies and was responsible for paper editing. HES also participated in clinical studies and reviewed the paper. All authors approved the final version of this paper.
Conflicts of interest: None declared.
Plagiarism check: This paper was screened twice using Cross-Check to verify originality before publication.
Peer review: This paper was double-blinded and stringently reviewed by international expert reviewers.
Barber MA, Conolley J, Spaulding CM, Dellon AL (2001) Evaluation of pressure threshold prior to foot ulceration: one-versus two-point static touch. J Am Podiatr Med Assoc 91:508-514.
Battiston B, Tos P, Cushway TR, Geuna S (2000) Nerve repair by means of vein filled with muscle grafts I. Clinical results. Microsurgery 20:32-36.
Battiston B, Geuna S, Ferrero M, Tos P (2005) Nerve repair by means of tubulization: literature review and personal clinical experience comparing biological and synthetic conduits for sensory nerve repair. Microsurgery 25:258-267.
Chao RP, Braün SA, Ta KT, Palesty JA, Mine R, Syed SA, Chang DJ, Thomson JG (2001) Early passive mobilization after digital nerve repair and grafting in a fresh cadaver. Plast Reconstr Surg 108:386-391.
Cheng AS, Hung L, Wong JM, Lau H, Chan J (2001) A prospective study of early tactile stimulation after digital nerve repair. Clin Orthop Relat Res:169-175.
Clare TD, de Haviland Mee S, Belcher HJCR (2004) Rehabilitation of digital nerve repair: is splinting necessary? J Hand Ther Br 29:552-556.
Dahlin LB (2008) Techniques of peripheral nerve repair. Scand J Surg 97:310-316.
Daniele HR, Aguado L (2003) Early compensatory sensory re-education. J Reconstr Microsurg 19:107-110.
Dellon AL, Jabaley ME (1982) Reeducation of sensation in the hand following nerve suture. Clin Orthop Relat Res:75-79.
Geuna S, Tos P, Battiston B, Giacobini-Robecchi MG (2004) Bridging peripheral nerve defects with muscle-vein combined guides. Neurol Res 26:139-144.
Henry FP, Farkhad RI, Butt FS, O’Shaughnessy M, O’Sullivan ST (2012) A comparison between complete immobilisation and protected active mobilisation in sensory nerve recovery following isolated digital nerve injury. J Hand Surg Eur Vol 37:422-426.
Imai H, Tajima T, Natsumi Y (1991) Successful reeducation of functional sensibility after median nerve repair at the wrist. J Hand Surg Am 16:60-65.
Jabir S, Iwuagwu FC (2014) Postoperative mobilization regimens following digital nerve repair: a systematic review. Eplasty 14:e5.
Lohmeyer JA, Siemers F, Mailänder P (2010) Therapy standards after flexor tendon and nerve injuries of the hand: results from a survey of German centres for hand surgery. Unfallchirurg 113:203-209.
Mackinnon SE, Dellon AL, O’Brien JP (1991) Changes in nerve fiber numbers distal to a nerve repair in the rat sciatic nerve model. Muscle Nerve 14:1116-1122.
Mailander P, Schaller E, Berger A, Ruhe K (1989) Return of static and moving 2-point discrimination following nerve reconstruction. Handchir Mikrochir Plast Chir 21:299-301.
Manoli T, Schulz L, Stahl S, Jaminet P, Schaller HE (2014) Evaluation of sensory recovery after reconstruction of digital nerves of the hand using muscle-in-vein conduits in comparison to nerve suture or nerve autografting. Microsurgery 34:608-615.
Marcoccio I, Ignazio M, Vigasio A, Adolfo V (2010) Muscle-in-vein nerve guide for secondary reconstruction in digital nerve lesions. J Hand Surg Am 35:1418-1426.
Miller LK, Chester R, Jerosch-Herold C (2012) Effects of sensory reeducation programs on functional hand sensibility after median and ulnar repair: a systematic review. J Hand Ther 25:297-306.
Millesi H (1985) Peripheral nerve repair: terminology, questions, and facts. J Reconstr Microsurg 2:21-31.
Oud T, Beelen A, Eijffinger E, Nollet F (2007) Sensory re-education after nerve injury of the upper limb: a systematic review. Clin Rehabil 21:483-494.
Parry CB, Salter M (1976) Sensory re-education after median nerve lesions. Hand 8:250-257.
Siemionow M, Brzezicki G (2009) Chapter 8: Current techniques and concepts in peripheral nerve repair. Int Rev Neurobiol 87:141-172.
Siemionow M, Bozkurt M, Zor F (2010) Regeneration and repair of peripheral nerves with different biomaterials: review. Microsurgery 30:574-588.
Tos P, Battiston B, Ciclamini D, Geuna S, Artiaco S (2012) Primary repair of crush nerve injuries by means of biological tubulization with muscle-vein-combined grafts. Microsurgery 32:358-363.
Vipond N, Taylor W, Rider M (2007) Postoperative splinting for isolated digital nerve injuries in the hand. J Hand Ther 20:222-230.
Yu RS, Catalano LWr, Barron OA, Johnson C, Glickel SZ (2004) Limited, protected postsurgical motion does not affect the results of digital nerve repair. J Hand Surg Am 29:302-306.
Copyedied by Keliris G, Oda R, Li CH, Song LP, Zhao M
10.4103/1673-5374.169638 http://www.nrronline.org/
How to cite this article: Manoli T, Schiefer JL, Schulz L, Fuchsberger T, Schaller HE (2016) Influence of immobilization and sensory re-education on the sensory recovery after reconstruction of digital nerves with direct suture or muscle-in-vein conduits. Neural Regen Res 11(2):338-
*Correspondence to: Theodora Manoli, M.D., theodora.manoli@gmail.com.
orcid: 0000-0003-3014-1990 (Theodora Manoli)
杂志排行
中国神经再生研究(英文版)的其它文章
- Impaired consciousness caused by injury of the lower ascending reticular activating system: evaluation by diffusion tensor tractography
- Epalrestat protects against diabetic peripheral neuropathy by alleviating oxidative stress and inhibiting polyol pathway
- Effects of microtubule-associated protein tau expression on neural stem cell migration after spinal cord injury
- Neuroprotective role of (Val8)GLP-1-Glu-PAL in an in vitro model of Parkinson’s disease
- Ginsenoside Rg1 protects against neurodegeneration by inducing neurite outgrowth in cultured hippocampal neurons
- Neural differentiation and synaptogenesis in retinal development