同步间歇指令通气支持下吸入氦氧混合气和空氧混合气治疗胎粪吸入综合征的随机对照试验
2016-09-19赵锦宁唐仕芳
马 娟 李 雪 陈 龙 汪 丽 赵锦宁 唐仕芳 史 源
·论著·
同步间歇指令通气支持下吸入氦氧混合气和空氧混合气治疗胎粪吸入综合征的随机对照试验
马娟李雪陈龙汪丽赵锦宁唐仕芳史源
目的探讨胎粪吸入综合征(MAS)新生儿在同步间歇指令通气(SIMV)支持下吸入氦氧混合气(Heliox)和空氧混合气的疗效。方法2014年3月1日至2015年5月30日在第三军医大学大坪医院NICU住院的MAS新生儿,以随机数字表法分为Heliox组和对照组,全部患儿均给予SIMV作为呼吸支持模式;Heliox组吸入Heliox 70(He 70%,O230%)6 h后更换吸入空氧混合气(O230%);对照组吸入空氧混合气。主要观察指标为治疗期间氧合指数(OI)和拔管时间,次要观察指标为机械通气并发症发生率、NICU住院时间、血气分析、炎症反应指标、心肌损伤标志物、生后28 d和100 d时振幅整合脑电图(aEEG)结果。结果Heliox组和对照组分别纳入33和31例。Heliox组OI显著高于对照组,差异有统计学意义(P=0.022), Heliox组拔管时间、机械通气并发症发生率及NICU住院时间均显著低于对照组,差异均有统计学意义(P分别为0.037,0.013和0.010);两组呼吸支持后2、6、12、24、48 h时点血气分析指标(pH、HCO3-1、BE、PaO2、PaCO2)差异均有统计学意义(P均<0.05); Heliox组6 h时点炎症反应指标(IL-6、IL-8、TNF-α、CRP)和24 h时点心肌损伤标志物(CK、 CK-MB)均较0 h时点降低,差异均有统计学意义(P均<0.05)。Heliox组生后28 d和100 d时aEEG检查神经发育重度异常发生率分别为9.1%和3.0%,显著低于对照组的25.8%和9.6%(P<0.05)。结论在SIMV支持下吸入Heliox治疗MAS新生儿较空氧混合气具有良好的疗效,安全性好,值得深入研究。
氦氧混合气;胎粪吸入综合征;新生儿;同步间歇指令通气
胎粪吸入综合征(MAS)是新生儿常见的呼吸系统疾病,以呼吸窘迫和持续肺动脉高压为主要临床表现,病死率高[1~3]。重症MAS患儿常需机械通气治疗[4~8],同步间歇指令通气(SIMV)是一种间歇正压通气(IPPV)与患儿自主呼吸有机结合的间歇按需通气模式,根据患儿自主呼吸要求提供预设通气,具有较少人机对抗产生、有效降低气道压力、减少撤机困难和防止呼吸肌萎缩的优点,已成为MAS治疗的重要手段[9~13]。近年来研究发现氦氧混合气(Heliox)应用于儿童呼吸系统疾病具有独特的优势。新生儿肺发育不完全、呼吸道狭窄,Heliox低密度的物理特性使氧气更易通过因炎症所致更加狭窄的气道管腔,从而可有效降低呼吸道阻力,增加血氧含量,改善呼吸系统症状[14~19]。本研究在SIMV呼吸支持下采用Heliox治疗MAS新生儿以探讨论其临床疗效。
1 方法
1.1伦理和知情同意本研究经第三军医大学大坪医院(我院)伦理委员会批准,所有受试新生儿的监护人均在试验前签署书面知情同意书。
1.2纳入标准①入院时符合第3版《实用新生儿学》临床诊断MAS标准;②符合我院新生儿科SIMV上机标准(出生6 h内应用气囊和面罩正压通气,胸部不抬起,或正压通气15~30 s,心率仍低于80~100·min-1,或1 min内仍无自主呼吸,pH<7.2);③胎龄≥37周且≤42周;④监护人签署书面知情同意书参与本研究。
1.3排除标准具备以下任意1项者:①患先天性或遗传代谢性疾病;②伴外科疾病,需行手术治疗。
1.4分组方法和分配隐藏实施符合入组条件的新生儿在取得书面知情同意书后,按随机数字表法分为Heliox组和对照组,分组序列号装入密闭信封,在试验前由不产生随机序列的试验人员抽取确定分组。
1.5干预措施①基础干预措施:入组新生儿均在气管插管下给予SIMV支持治疗(美国鸟牌AVEA呼吸机,具有氦氧入口接头),根据胎龄调整呼吸机参数(吸气峰压、呼气末正压、吸气时间、吸呼比、呼吸频率),到达目标氧饱和度95%。 ②不同组别干预措施:Heliox组吸入Heliox 70(He 70%,O230%),吸入6 h后更换为空氧混合气(O230%);对照组吸入空氧混合气。③撤机指征:PIP≤15 cmH2O,有效自主呼吸逐渐增强,呼吸机呼吸频率≤10·min-1,血气分析结果正常。
1.6疗效指标
1.6.1主要观察指标治疗期间记录并统计两组患儿氧合指数(OI)和拔管时间。
1.6.2次要观察指标①血气分析:于呼吸支持 0、2、6、12、24、48 h时点采集患儿末梢血0.2 mL行血气分析(pH、HCO3-1、BE、PaO2、PaCO2)。②机械通气并发症发生率。③炎症反应指标和心肌损伤标志物: 采集静脉血,于0和6 h时点测定IL-6、IL-8、CRP、TNF-α,0和24 h时点测定肌酸激酶(CK)、肌酸激酶同工酶(CK-MB)。④NICU住院时间。⑤神经发育情况:于生后28 d和100 d召回行振幅整合脑电图(aEEG)检查,aEEG最低电压<5 μV,最高电压<10 μV为神经发育重度异常[20]。

2 结果
2.1一般情况2014年3月1日至2015年5月30日我院NICU中符合本文纳入和排除标准检验的 MAS新生儿64例,具体纳入和排除流程见图1。Heliox组33例,对照组31例。表1显示,两组0 h时点性别、胎龄、出生体重、分娩方式、炎症反应指标和心肌损伤标志物的差异均无统计学差异(P均>0.05)。
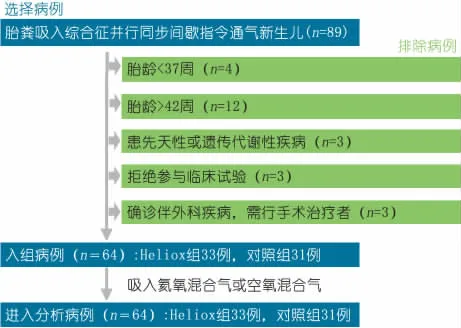
图1 研究对象筛选流程
2.2主要观察指标Heliox组和对照组OI为(301±22)和(264±22) ,t=5.47,P=0.022;拔管时间为(78±30)和(115±50)h,t=12.32,P=0.037;两组2个主要结局指标差异均有统计学意义。
2.3次要观察指标
2.3.1血气分析表2显示,Heliox组和对照组在2、6、12、24、48 h时点pH、PaO2、BE、HCO3-较0 h时点均升高,PaCO2下降 , 上述时点血气分析指标2组差异均有统计学意义。


Heliox(n=33)对照组(n=31)χ2/tP男/女20/1319/120.0030.08胎龄/周39.2±1.539.5±1.217.80.09体重/g3528±2513617±2495.710.12阴道产/剖腹产17/1616/15<0.0010.07IL-8/pg·mL-167.4±6.967.6±7.06.540.25IL-6/pg·mL-131.3±3.131.2±4.03.680.31TNF-α/ng·L-149.4±4.649.4±4.99.540.09CRP/mg·L-16.1±0.86.1±0.86.370.06CK/U·L-1176.1±18.3177.6±18.06.950.06CK-MB/U·L-127.3±8.127.4±8.04.390.07
2.3.2机械通气并发症发生率Heliox组和对照组机械通气并发症发生率为15.2%和29.0%,χ2=5.791,P=0.013,差异有统计学意义。
2.3.3炎症反应指标Heliox组和对照组6 h时点IL-6分别为(15.2±1.8)和(20.0±2.6)pg·mL-1,差异有统计学意义(t=3.91,P=0.019),Heliox组0 h与6 h时点IL-6差异有统计学意义(t=8.45,P=0.033),对照组0 h与6 h时点IL-6差异无统计学意义(t=7.92,P=0.063);Heliox组和对照组6 h时点IL-8分别为(31.7±4.4)和(36.7±4.3)pg·mL-1,差异有统计学意义(t=7.62,P=0.022),Heliox组0 h与6 h时点 IL-8差异有统计学意义(t=3.17,P=0.021),对照组0 h与6 h时点 IL-8差异无统计学意义(t=6.99,P=0.103);Heliox组和对照组TNF-α分别为(38.5±3.9)和(43.0±4.2)ng·mL-1,差异有统计学意义(t=11.25,P=0.034),Heliox组0 h与6 h时点TNF-α差异有统计学意义(t=13.35,P=0.010),对照组0 h与6 h时点TNF-α差异无统计学意义(t=3.16,P=0.072);Heliox组和对照组CRP分别为(5.6±0.5)和(5.9±0.7)mg·L-1,差异有统计学意义(t=9.35,P=0.039),Heliox组0 h与6 h时点CRP差异有统计学意义(t=17.57,P=0.034),对照组0 h与6 h时点CRP差异无统计学意义(t=6.77,P=0.088)。
2.3.4心肌损伤标志物Heliox组和对照组24 h时点CK分别为(131.7±13.7)和(156.6±14.4)U·L-1,差异有统计学意义(t=6.73,P=0.045),Heliox组0 h与24 h时点CK差异有统计学意义(t=8.39,P=0.043),对照组0 h与24 h时点CK差异无统计学意义(t=4.33,P=0.076);Heliox组和对照组24 h时点CK-MB分别为(23.2±7.2)和(26.0±7.9)U·L-1,差异有统计学意义(t=3.67,P=0.039),Heliox组0 h与24 h时点CK-MB差异有统计学意义(t=7.77,P=0.008),对照组0 h与24 h时点CK-MB差异无统计学意义(t=7.90,P=0.055)。
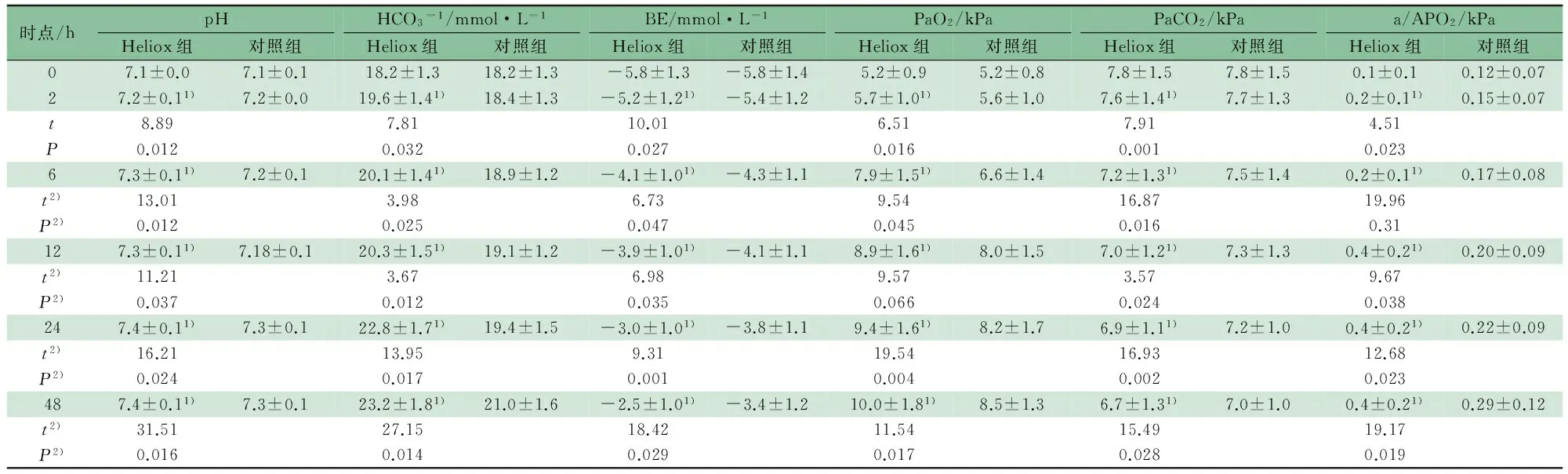
时点/hpHHeliox组对照组HCO3-1/mmol·L-1Heliox组对照组BE/mmol·L-1Heliox组对照组PaO2/kPaHeliox组对照组PaCO2/kPaHeliox组对照组a/APO2/kPaHeliox组对照组07.1±0.07.1±0.118.2±1.318.2±1.3-5.8±1.3-5.8±1.45.2±0.95.2±0.87.8±1.57.8±1.50.1±0.10.12±0.0727.2±0.11)7.2±0.019.6±1.41)18.4±1.3-5.2±1.21)-5.4±1.25.7±1.01)5.6±1.07.6±1.41)7.7±1.30.2±0.11)0.15±0.07t8.897.8110.016.517.914.51P0.0120.0320.0270.0160.0010.02367.3±0.11)7.2±0.120.1±1.41)18.9±1.2-4.1±1.01)-4.3±1.17.9±1.51)6.6±1.47.2±1.31)7.5±1.40.2±0.11)0.17±0.08t2)13.013.986.739.5416.8719.96P2)0.0120.0250.0470.0450.0160.31127.3±0.11)7.18±0.120.3±1.51)19.1±1.2-3.9±1.01)-4.1±1.18.9±1.61)8.0±1.57.0±1.21)7.3±1.30.4±0.21)0.20±0.09t2)11.213.676.989.573.579.67P2)0.0370.0120.0350.0660.0240.038247.4±0.11)7.3±0.122.8±1.71)19.4±1.5-3.0±1.01)-3.8±1.19.4±1.61)8.2±1.76.9±1.11)7.2±1.00.4±0.21)0.22±0.09t2)16.2113.959.3119.5416.9312.68P2)0.0240.0170.0010.0040.0020.023487.4±0.11)7.3±0.123.2±1.81)21.0±1.6-2.5±1.01)-3.4±1.210.0±1.81)8.5±1.36.7±1.31)7.0±1.00.4±0.21)0.29±0.12t2)31.5127.1518.4211.5415.4919.17P2)0.0160.0140.0290.0170.0280.019
注1)Heliox组与对照组相比P<0.05;2) 与0 h时点相比
2.3.5NICU住院时间Heliox组和对照组NICU住院时间为(15.3±4.2)和(19.5±5.0)d,t=7.98,P=0.010,差异有统计学意义。
2.3.6神经发育情况生后28 d时aEEG检查显示Heliox组和对照组神经发育重度异常发生率分别为9.1%(3/33)和25.8%(8/31),差异有统计学意义(χ2=3.138,P=0.047)。生后100 d时aEEG检查显示Heliox组和对照组重度异常发生率分别为3.0%(1/33)和9.6%(3/31),差异有统计学意义(χ2=3.38,P=0.027)。
3 讨论
氦气是无色无味且无毒的非易燃惰性单原子气体,在体内与其他气体不发生反应,无药理活性,具有极好的生物安全性。MAS的主要发病原因为胎儿排出胎粪污染羊水,随后将其吸入呼吸道而引起机械性阻塞,使气道狭窄、阻力变大。氦气低密度、高黏滞度和运动时受到阻力更小的物理特性,使其在MAS的治疗中可显著增加每分钟通气量,增大呼气流速,减轻呼吸功耗,促进氧气向肺泡弥散及CO2排除,有效改善肺顺应性[21,22],因此亟需开发更有效的机械通气方案和模式改善新生儿预后,提高严重低氧的新生儿MAS治疗水平, SIMV较少产生人机对抗,同时心血管并发症少[7],而Heliox低密度的物理特性更适用于新生儿狭窄的呼吸道,有效提高血氧含量[23~25],因此在SIMV支持下予Heliox治疗MAS有可能具有重要的潜在临床应用价值。
MAS可致肺损伤、呼吸衰竭、气漏及持续肺动脉高压,如未及时发现并处理,可能导致新生儿死亡。研究显示氦气可减轻肺损害的炎症反应,且具备有效的抗炎作用,动物实验显示氦气可降低小鼠肺泡出血,肺组织中性粒细胞侵润、水肿和肺透明膜的发生[26],针对MAS患儿的全身化学性炎症反应,采用Heliox联合SIMV治疗MAS可有效发挥抗炎作用,本研究Heliox组较对照组炎症反应指标得到显著改善。Heinen等[27]的动物研究表明氦气在缺血再灌注中具有保护心脏的作用,临床上显示MAS患儿常并发心肌损害,心肌损害的严重程度进一步增加了MAS患儿心力衰竭发生率,本研究显示与对照组相比,Heliox组缺氧状况得到了显著改善,验证了动物实验结果[26,27],Heliox治疗可有效减轻肺损害的炎症反应,且具备一定的抗炎作用,同时在缺血再灌注中具有保护心脏的作用。
本研究Heliox组血气分析指标显著优于对照组,表明采用Heliox治疗MAS有效改善了患儿通气效果,可有效缓解新生儿症状;Heliox组OI、拔管时间、住院时间、机械通气并发症发生率均优于对照组,显示出良好的近期疗效;新生儿窒息的本质是缺氧,多为胎儿窒息(宫内窘迫)的延续,早期可直接导致死亡,远期可导致多种神经系统并发症及后遗症。重症MAS常合并新生儿窒息,所以早期诊断新生儿窒息所造成的脑损伤并积极进行临床干预,对降低患儿病死率及致残率具有重要意义。
aEEG能简便有效的评价神经功能,对神经系统损伤预后有较高的预测价值[28,29];本研究于患儿生后28 d及100 d时行aEEG检查评估神经发育情况,Heliox组28 d及100 d时aEEG重度异常发生率分别为9.1%和3.0%,显著低于对照组的25.8%和9.6%,有较好的近期疗效。
本文为SIMV支持下予Heliox治疗MAS疗效的初步结果,样本量不足可能会影响结果的可靠性;MAS新生儿生后28 d及100 d时aEEG仅可反映近期神经发育情况,并不反映远期神经发育结局。
[1] Konduri GG,Kim UO.Advances in the diagnosis and management of persistent pulmonary hypertension of the newborn.Pediatr Clin North Am,2009,56(3):579-600
[2] Chotigeat U,Champrasert M,Khorana M.et al.Iloprost inhalation for the treatment of severe persistent pulmonary hypertension of the newborn,experience at QSNICH.J Med Assoc Thai,2014(S6):89-94
[3] Kahveci H,Yilmaz O,Avsar UZ,et al.Oral sildenafil and inhaled iloprost in the treatment of pulmonary hypertension of the newborn.Pediatr Pulmonol,2014,49(12):1205-1213
[4] Singh BS,Clark RH,Powers RJ,et al.Meconium aspiration syndrome remains a significant problem in the NICU:Outcomes and treatment patterns in term neonates admitted for intensive care during a ten-year period.J Perinatol,2009,29(7):497-503
[5] Preutthipan A.Home Mechanical Ventilation in Children. Indian J Pediatr,2015,82(9):852-859
[6] Solevag AL,Solberg MT,Saltyte-Benth J.Pulse oximetry performance in mechanically ventilated newborn infants.Early Hum Dev,2015,91(8):471-473
[7] Shi Y,Niu JL,Cai ML,et al.Dimensionless study on dynamics of pressure controlled mechanical ventilation system.Journal of Mechanical Science and Technology,2015,29(2):431-439
[8] Kacmarek RM,Pirrone M,Berra L.Assisted mechanical ventilation:the future is now.BMC Anesthesiol,2015,15:110
[9] Bhutani VK.Developing a systems approach to prevent meconium aspiration syndrome:lessons learned from multinational studies.J Perinatol,2008,28(S3):30-35
[10] Chen XY,Li K,Light AR,et al.Simvastatin attenuates formalin-induced nociceptive behaviors by inhibiting microglial RhoA and p38 MAPK activation.J Pain,2013,14(11):1310-1319
[11] Patel DS,Rafferty GF,Lee S,et al.Work of breathing during SIMV with and without pressure support.Arch Dis Child,2009,94(6):434-436
[12] Hussein K,Hasan AA.Proportional assist ventilation versus conventional synchronized intermittent mandatory ventilation in chronic obstructive pulmonary disease.Egyptian Journal of Chest Diseases and Tuberculosis,2014,64(3):987-994
[13] Mabrouk AA,Osama F.Mansour.et al.Evaluation of some predictors for successful weaning from mechanical ventilation.Egyptian Journal of Chest Diseases and Tuberculosis,2015,64(3):707
[14] Myers TR.Use of heliox in children.Respir Care,2006,51(6):619-631
[15]Szczapa T,Gadzinowski J.Use of heliox in the management of neonates with meconium aspiration syndrome.Neonatology,2011,100(3):265-270
[16]Myers TR,Therapeutic gases for neonatal and pediatric respiratory care.Respir Care,2003,48(4):399-425
[17]Guzmán-Corena a,Morales-Payares D,Pinzón-Redondo H. PRS7-The Use of Heliox in Hospitalized Children From Cartagena Colombia .Value in Health,2015,18(3):170
[18]Jurickova I,Roubík K,Muller M.Delivery of heliox with a semi-closed circuit during spontaneous breathing:a comparative economic theoretical study.BMC Pulm Med,2015,15(1):1-8
[19]Kline-Krammes S,Reed C,Giuliano JS Jr,et al.Heliox in children with croup:a strategy to hasten improvement.Air Med J,2012,31(3):131-137
[20]施亿赟,程国强,邵红梅,等.正常足月新生儿振幅整合脑电图特点的多中心研究.中国循证儿科杂志,2009(4) 6:514-522
[21]Ancora G,Maranella F,Locatelli C,et al.Changes in cerebral homodynamic and amplitude integrated EEG in an asphyxiated newborn during and after cool cap treatment.Brain Dev,2009,31(6):442-444
[22]Beurskens CJ,Wosten-van Asperen RM,Preckel B,et al.The potential of heliox as a therapy for acute respiratory distress syndrome in adults and children:a descriptive review.Respiration,2015,89(2):166-174
[23]Hess D.Ventilator modes used in weaning.Chest,2001,120(6):474-476
[24]El-Khatib M,Jamaleddine G,Soubra R,et al.Pattern of spontaneous breathing:potential marker for weaning outcome.Spontaneous breathing pattern and weaning from mechanical ventilation.Intensive Care Med,2001,27(1):52-58
[25]Quilez ME,Fuster G,Villar J,et al.Erratum to:Injurious mechanical ventilation affects neuronal activation in ventilated rats.Crit Care,2015,19:379
[26]Yilmaz S,Daglioglu K,Yildizdas D,et al.,The effectiveness of heliox in acute respiratory distress syndrome.Ann Thorac Med,2013,8(1):46-52
[27]Heinen A,Huhn R,Smeele KM,et al.,Helium-induced preconditioning in young and old rat heart:impact of mitochondrial Ca(2 + ) -sensitive potassium channel activation.Anesthesiology,2008,109(5):830-836
[28]Hudson J.Facilitating normal physiology in the presence of meconium stained liquor.Pract Midwife,2015,18(6):16-19
[29]Shany E,Benzaquen O,Friger M,et al.Influence of antiepileptic drugs on amplitude-integrated electroencephalography.Pediatr Neurol,2008,39(6):387-391
(本文编辑:张崇凡)
Randomized controlled trial of inhaling heliox and air oxygen mixture in meconium aspiration syndrom under the support of synchronized intermittent mandatory ventilation
MAJuan,LIXue,CHENLong,WANGLi,ZHAOJin-ning,TANGShi-fang,SHIYuan
(DepartmentofPediatrics,DapingHospital,ThirdMilitaryMedicalUniversity,Chongqing400042,China)
SHI Yuan,E-mail:petshi530@ vip.163.com
Objective To investigate the curative effect of inhaling heliox and air oxygen mixture in meconium aspiration syndrome under the support of synchronized intermittent mandatory ventilation (SIMV).MethodsSixty-four children with MAS in NICU of the DaPing Hospital, Third Military Medical University from March 1st, 2014 to May 30th, 2015 were taken as samples. The children, who were treated with SIMV as respiratory support mode, were divided into Helio group (n=33) and control group (n=31) in accordance with the random number table. Heliox group inhaled Heliox 70 (He 70% O230%) for 6 h after replacement of inhaling air oxygen mixture (30% O2); Control group inhaled air oxygen mixed gas. Main outcome measures: oxygenation index (OI) during treatment and extubation time; Secondary outcome measures: incidence of the complications of mechanical ventilation, hospital stays in NICU, bood gas analysis, inflammation index and myocardial injury markers, amplitude integrated electroencephalography (aEEG) results.ResultsOI in the heliox group was significantly higher than that in the control group; the difference was statistically significant (P=0.022), and the extubation time, incidence of the complications of mechanical ventilation and hospital stays in NICU of heliox group were significantly lower than those of control group; the differences were statistically significant (P=0.037, 0.013 and 0.010). Blood gas analysis index (pH, HCO3-, BE, PaO2, PaCO2) in two groups (2, 6, 12, 24, 48 h) presented some discrepancy; the differences were statistically significant (P<0.05). The inflammation index (IL-6, IL-8, TNF-a CRP) at 6 h and myocardial injury markers (CK, CK-MB) at 24 h of the two groups were decreased compared with those at 0 h, and heliox group decreased more significantly compared with the control group; the differences were statistically significant (P<0.05). The aEEG abnormal checking rate of children born after 28 and 100 days of heliox group was 9.1% and 3.0%, significantly lower than 25.8% and 9.6% of the control group (P< 0.05).ConclusionInhaling heliox has better curative effect and high security than inhaling air oxygen mixture for MAS under the support of SIMV, and it is worthy of further study.
Heliox; Meconium aspiration syndrome; Neonate; Synchronized intermittent mandatory ventilation
10.3969/j.issn.1673-5501.2016.02.003
第三军医大学大坪医院儿科重庆,400042
史源,E-mail:petshi530@ vip.163.com
2015-12-30
2016-03-07)