宫腹腔镜联合诊治女性不孕症461例临床疗效分析
2016-08-17乌云塔娜刘玲玲王蔼明
乌云塔娜 刘玲玲 赵 勇 王蔼明,*
1.内蒙古民族大学临床医学院(通辽,028000);2.中国人民解放军海军总医院生殖中心
·临床研究·
宫腹腔镜联合诊治女性不孕症461例临床疗效分析
乌云塔娜1刘玲玲2赵 勇2王蔼明2,*
1.内蒙古民族大学临床医学院(通辽,028000);2.中国人民解放军海军总医院生殖中心
目的:探讨宫腹腔镜联合手术在女性不孕症诊断治疗价值以及术后妊娠结局的相关因素。方法:回顾性分析2008年1月~2014年5月因不孕症在海军总医院行宫腹腔镜联合检查和手术治疗的患者461例,宫腹腔镜下评估不孕症病因、术后电话随访妊娠情况、妊娠结局,比较原发性不孕症和继发性不孕症的妊娠率,观察年龄和盆腔粘连程度对妊娠结局的影响。结果:461例不孕症患者中,原发性不孕225例(48.8%),继发性不孕236例(51.2%)。不孕症的主要原因是盆腔粘连54.5%(251例)、输卵管阻塞50.8%(234例)、子宫内膜异位症157例(34.1%)。盆腔粘连、输卵管阻塞和宫腔粘连发生率继发生不孕症高于原发性不孕症,生殖器结核仅发生于原发性不孕者,其他不孕因素两者之间没有统计学差异。术后随访率为85.25%。术后自然妊娠50.6%,原发性不孕患者的妊娠率为49.5%,继发性不孕患者的妊娠率为51.8%,妊娠时间主要集中在术后1年内,足月分娩43.8%。20~30岁年龄组的妊娠率(54.9%)高于31~43岁组(45.5%)(P<0.05)。无盆腔粘连、轻、中度粘连者和重度粘连者的妊娠率分别为61.5%、54.8%、40.6%和18.9%,无盆腔粘连者妊娠率和足月分娩率明显高于盆腔粘连者(P<0.05);盆腔粘连组中轻、中度粘连者妊娠率和足月分娩率与重度粘连者比较,差异有统计学意义(P<0.05),轻度和中度粘连间比较无统计学差异(P>0.05)。结论:宫腹腔镜联合手术能更加直观的评估不孕症病因,同时可针对病因进行相应治疗,手术时间短、创伤小,能提高不孕患者的临床妊娠率和足月分娩率,对女性不孕症的诊断与治疗有重要临床价值。
宫腹腔镜联合检查;不孕症;妊娠率;足月分娩率
不孕症病因复杂,其中女性因素占40%~55%、男方因素占30%~40%、双方因素占10%、不明原因占10%[1],我国发病率约为7%~10%[2]。目前,常规检查尚不能明确不孕症病因,随着内镜技术的发展,宫腹腔镜联合手术在全面了解盆腔和宫腔内病变的同时能进行针对性治疗,在诊治女性不孕症方面发挥着重要作用。本文对因不孕症在本院行宫腹腔镜联合检查的患者资料进行回顾性分析,探讨不孕症病因及术后妊娠率、妊娠结局以及妊娠时间。
1 资料与方法
1.1 临床资料
2009年1月~2014年5月因不孕症在中国人民解放军海军总医院行宫腹腔镜联合诊治的患者461例,其中原发性不孕症225例(48.81%),继发性不孕症236例(51.19%);年龄30.3±3.9(20~43)岁,不孕3.3±2.7(1~19)年。均接受宫腹腔镜联合检查和治疗, 治疗后至少一侧输卵管通畅;排除男方因素不孕、生殖道畸形,双侧输卵管复通失败或切除者。
1.2 手术方法
1.2.1 术前准备及麻醉 手术前常规检查及准备,排除手术禁忌证,签署知情同意书。所有患者均月经干净后3~7d手术,行气管插管全麻后,患者行膀胱截石位,常规消毒铺巾。
1.2.2 置腹腔镜 在脐上或脐轮下缘穿刺放入Trocar套管针,形成CO2气腹,于下腹两侧各做一个5mm切口,置腹腔镜探查并行相应手术处理,盆腔粘连患者分离粘连,尽量恢复盆腔各脏器正常形态。有输卵管伞端粘连、积水患者行修复整形或造口术;有输卵管系膜囊肿者行剥除术;对输卵管间质部梗阻者腹腔镜监视下宫腔镜下COOK导丝复通,复通术后再行输卵管间质部插管行美蓝通液,明确复通效果。伞端开口处见美蓝液流出,则表示手术疏通成功。若复通失败,根据严重程度考虑是否行IVF助孕或切除输卵管。对于严重积水,功能丧失者征求患者同意后行输卵管结扎术或切除术。双侧输卵管复通失败或者切除者均不纳入本研究。子宫内膜异位病灶行病灶电凝术或囊肿剥除术,卵巢良性肿瘤剥除术等。
1.2.3 置宫腔镜 经宫颈置入宫腔镜,在腹腔镜和宫腔镜下观察宫腔内形态和内膜情况,根据宫腔病变行宫腔粘连分解术、子宫内膜息肉摘除术+诊刮术、子宫纵隔电切除术、影响妊娠的粘膜下肌瘤行肌瘤剔除术等。
1.3 效果评价
1.3.1 输卵管通畅度 ①通畅,输卵管注入美兰溶液无阻力,伞端见美兰液流出,输卵管无局部膨大;②通而不畅,注入美兰液有轻度阻力、加压推美兰输卵管先膨大再见美兰液从伞端流出;③阻塞,阻力大,输卵管无充盈,注液未见伞端有美兰液流出,或者美兰液自宫角流出。
1.3.2 盆腔粘连评分标准[3]①粘连程度,疏松1分,中度致密2分,重度致密3分;②范围,2~6cm 1分,>6~10cm 2分,>10cm 3分;③直肠子宫陷窝,无封闭0分,部分封闭为1分,完全封闭为2分;④双侧输卵管,无粘连0分,单侧粘连1分,双侧粘连2分;⑤双侧输卵管伞端,无闭锁0分,单侧闭锁1分,双侧闭锁2分;⑥双侧卵巢,无粘连0分,单侧粘连1分,双侧粘连2分。各项评分相加:轻度粘连2~5分,中度粘连6~9分,重度粘连10~14分。
1.4 随访
术后1个月开始门诊及电话随访,均随访1~2年,了解患者妊娠情况、妊娠结局以及妊娠时间。
1.5 统计学处理
采用SPSS21.0进行统计分析,组间计数资料率的比较采用χ2检验,P<0.05为差异有统计学意义。
2 结果
2.1宫腹腔镜联合诊断不孕症病因情况
统计结果表明,女性不孕的主要病因由盆腔粘连54.45%(251/461),输卵管阻塞50.76%(234/461)和子宫内膜异位症34.06%(157/461)组成。其中,盆腔粘连、输卵管阻塞、宫腔粘连、子宫内膜结核在原发性不孕症和继发性不孕症中存在差异(P<0.05)。本研究中有15例为不明原因不孕外,其他均有1至多个不孕因素。

表1 原发和继发不孕的病因诊断比较[例(%)]
2.2 宫腹腔镜术后妊娠结局
461例患者中393例获得随访,随访率85.24%,自然妊娠率为50.64%(199/393),足月分娩率为43.76%。年龄在20~30岁组的妊娠率(54.88%)高于31~43岁组(45.51%);随着粘连程度的加重,妊娠率有逐渐下降的趋势;腔粘连者流产和异位妊娠率高于无粘连者(P<0.05);盆腔轻、中度粘连者妊娠率和足月分娩率与重度粘连者比较有统计学差异(P<0.05),轻度和中度粘连间比较无统计学差异(P>0.05)。见表2。
2.4 宫腹腔镜术后妊娠时间分布
随访93例患者中199例妊娠,其中术后<6个月妊娠96例(48.24%),6~12个月妊娠69例(34.67%),累积1年妊娠165例(82.91%);1年后妊娠34例(17.09%)。
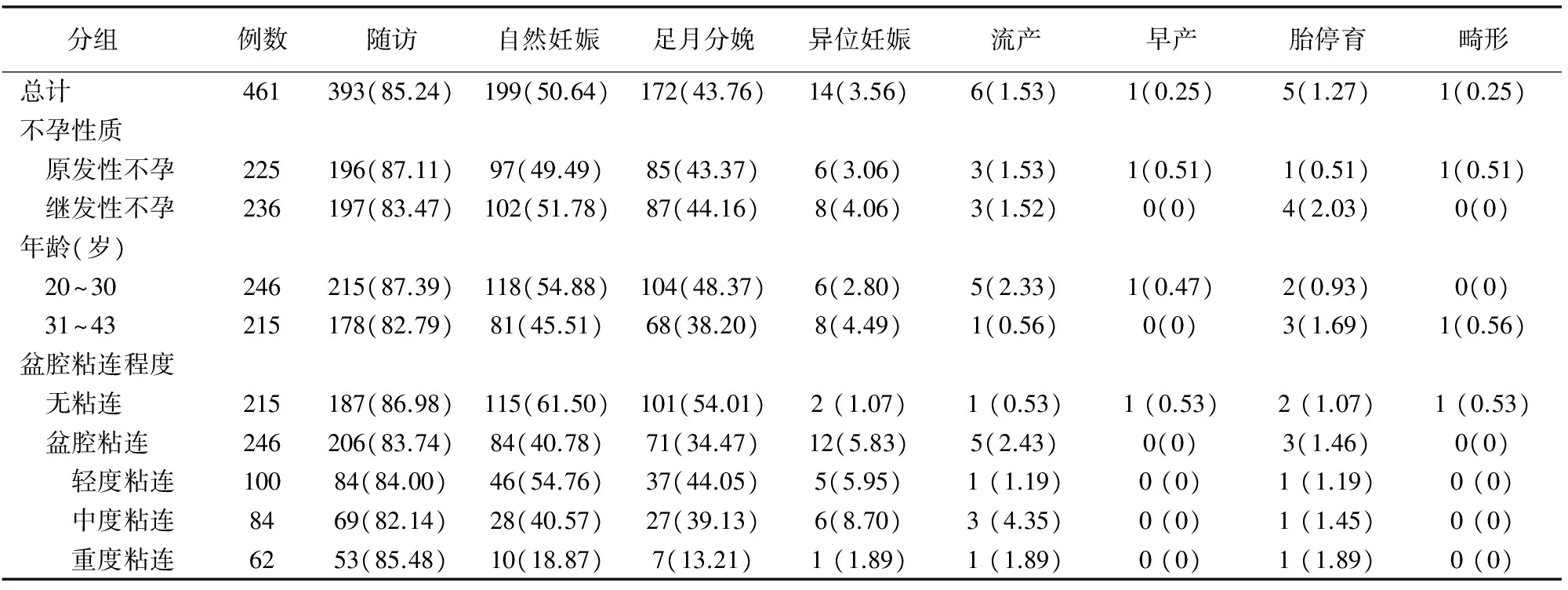
表2 各种不孕因素宫腹腔镜术后妊娠结局比较[例(%)]
3 讨论
女性不孕症病因复杂,25%的不孕症患者有>1个不孕因素[1]。本研究中,盆腔粘连、输卵管阻塞、子宫内膜异位症是导致女性不孕症的三大主要因素,这与国外一些研究结果相似[4-6]。临床上一些盆腔疾病很难在常规盆腔检查中发现[7]。传统的输卵管造影检查也不能准确判断盆腔及宫腔内的小病变,对判断输卵管周围组织粘连的准确率明显低于腹腔镜检查。还有报道称,单纯宫腔镜检查并发症发生率为1.65%[8],腹腔镜监视下行宫腔镜操作并发症可明显下降[9]。宫腹腔镜联合手术能在诊断的同时兼具治疗,恢复正常组织结构,减少手术并发症,增加术后妊娠率,妊娠结局理想。
3.1 不孕症病因分析
有研究显示,盆腔粘连是女性不孕症的首要原因[6]。90%以上的不明原因不孕症与盆腔粘连有关[10]。本文结果显示,54.45%的不孕患者有盆腔粘连,继发性不孕症盆腔粘连发生率高于原发性不孕症。其中重度粘连在原发、继发性不孕中差异更明显。在宫腹腔镜联合手术下分离粘连,恢复盆腔正常解剖关系,不仅能提高手术成功率,还避免了开腹手术带来的术后再粘连的发生。
输卵管阻塞是造成不孕的第二大因素,本文原发性不孕症和继发性不孕症输卵管阻塞发生率分别为45.78%和55.51%。输卵管阻塞通常是由于盆腔炎、子宫内膜异位症和盆腔手术后的损伤引起[11]。传统的输卵管造影检查不能准确的判断盆腔及宫腔内的小病变,漏诊率达32.12%[12]。Kasius等[13]的研究也表明,HSG对判断输卵管近端阻塞的准确率为70%,但对判断输卵管周围组织粘连的准确率只有11%,明显低于腹腔镜检查。单纯腹腔镜或宫腔镜对某些疾病的诊断与治疗有一定的局限性,宫腹腔镜联合手术能互相弥补不足,全面评估盆腔及宫腔病变,并进行相应治疗。
子宫内膜异位症是不孕症第三大病因。有研究表明,25%~50%的不孕症患者合并子宫内膜异位症,而30%~50%的子宫内膜异位症患者合并不孕[14]。腹腔镜检查是诊断子宫内膜异位症的金标准[15]。腹腔镜手术不仅可以清楚地观察到子宫内膜异位病灶,还可以分离粘连并恢复输卵管、卵巢、子宫等盆腔脏器的正常解剖关系,也可以缓解患者的痛经及慢性盆腔痛等症状,有利于提高受孕率。
除上述三大病因外,本文资料中子宫内膜息肉、子宫肌瘤、子宫畸形、PCOS、宫腔粘连、输卵管系膜囊肿、卵巢良性肿瘤、生殖器结核等依次是造成不孕症的病因。其中子宫内膜息肉发生率最高,子宫畸形中纵隔子宫发生率最高,这与Nayak 等[16]的研究结果一致。有研究表明,纵隔子宫切除后妊娠结局(足月分娩率80% 、早产率5%、妊娠丢失率15%)比处理前(妊娠丢失率80%、早产率10%、足月分娩率10%)明显改善。继发性不孕患者中宫腔粘连发生率明显高于原发性不孕患者,这与患者多次人工流产史或宫内膜结核有关[17]。生殖器结核仅发生于原发性不孕症,这主要是由于输卵管黏膜被破坏或粘连、功能丧失,内膜结核主要影响受精卵着床。
3.2 术后妊娠率相关因素分析
393例随访患者中自然妊娠率为50.64%,足月分娩率为43.76%。20~30岁年龄组的自然妊娠率明显高于31~43岁组。因此,女性年龄是生育力的重要决定因素。所以,在临床上对≤30岁不孕症患者可以建议其先行宫腹腔镜评估与诊治。对年龄较大者可根据患者的病情、术中双侧输卵管通常情况及损伤程度、卵巢储备功能等进行综合评估,决定是否行辅助生殖技术助孕。
本文结果显示,随着粘连程度的加重,妊娠率有逐渐下降的趋势。盆腔粘连组中轻、中度粘连者妊娠率和足月分娩率高于重度粘连者,无盆腔粘连者妊娠率和足月分娩率明显高于盆腔粘连者。说明盆腔粘连对妊娠结局的影响很大。分析其原因:轻度粘连未破坏输卵管的结构和走形,而中、重度粘连可使输卵管扭曲、变形、管壁增厚硬化、黏膜被破坏、伞端粘连闭锁或输卵管积水,导致输卵管阻塞,从而影响妊娠。而且重度粘连者输卵管内部生理功能已严重损伤,很难恢复输卵管正常解剖结构,手术效果欠佳。因此,宫腹腔镜下分离盆腔粘连,充分暴露输卵管、卵巢、子宫及盆腔结缔组织,尽量恢复盆腔正常解剖形态和功能,能提高妊娠率和足月分娩率,而且能降低早期流产和异位妊娠的发生。
3.3 术后妊娠时间分析
199例自然妊娠中术后1年内妊娠占82.91%,说明妊娠多集中在术后1年内。因此建议患者术后1年内,甚至6个月内尽早试孕,可提高受孕率。如果术后1年后仍未成功受孕者,年轻、病情较轻者可行输卵管检查,如输卵管通畅可以继续指导妊娠;如果患者年龄较大、卵巢储备功能低下、粘连复发或输卵管功能严重受损,建议患者尽早行IVF-ET助孕,以避免错过最佳生育年龄。
宫腹腔镜联合手术能安全、有效、全面的评估不孕症患者盆腔、宫腔情况,在检查的同时对盆腔、输卵管、宫腔病变进行相应的治疗,并发症少、漏诊率低、恢复快、创伤小、术后妊娠结局理想,还可改善盆腔环境,为辅助生殖治疗创造有利条件,对女性不孕症的诊治有重要的临床价值。
[1] Boivin J, Bunting L, Collins JA, et al. International estimates of infertility prevalence and treatment-seeking: Potential need and demand for infertility medical care. Hum Reprod, 2007,22:1506-1512.
[2] 谢幸,苟文丽.妇产科学[M].第8版.北京:人民卫生出版社,2013:369.
[3] 孙爱军,黄坚,周远征,等.不孕症患者不同程度盆腔粘连的相关因素探讨[J].生殖医学杂志,2007,16(3):145-149.
[4] Aziz N. Laparoscopic evaluation of female factors in infertility.J Coll Physicians Surg Pak,2010,20(10):649-52.
[5] Jian G, Khatuja R, JUneja A,Mehta S.Laparoscopy:As a First Line Diagnostic Tool for Infertility Evaluation.J Clin Diagn Res,2014, 8(10): OC01-OC02.
[6] King CR, Heuer MA, Scharf ES, Shuster JJ.Treating Female Infertility and Improving IVF Pregnancy Rates With a Manual Physical Therapy Technique. MedGenMed, 2004,6(2): 51.
[7] Puri S,Jain D,Kaushal S,et al.Laparohysteroscopy in female infertility: A diagnostic cum therapeutic tool in Indian setting.Int J Appl Basic Med Res, 2015, 5(1): 46-48.
[8] Mettler L, Wendland EM, Patel P,et al.Hysteroscopy:an analysis of 2-years' experience.JSLS,2002,6(3):195-197.
[9] Erhong Zhang, Yanan Zhang, Li Fang, et al.Combined Hysterolaparoscopy for the Diagnosis of Famale Infertility:a Retrospective Study of 132 Patients in china. Mater Sociomed,2014,26(3):156-157.
[10] Litm an E, Giudice L, Lathi R,et al.Role of laparoscopic treatment of endometriosis in patients with failed in vitro fertilization cycles[J].Fertil Steril,2005,84(6):1574-1578.
[11] Bhattacharya S, Johson N, Tijani HA,et al.Female infertility. BMJ Clin Evid, 2010: 0819.
[12] Vaid K, Mehra S, Verma M, Jain S, et al. Pan endoscopic approach "hysterolaparoscopy"as an initial procedure in selected infertile women. J Clin Diagn Res, 2014, 8(2): 95-98.
[13] Kasius JC, Fatemi HM,et al.The impact of endometritis on reproductive outcome[J].Fertil Steril,2011,96(6):1451-1456.
[14] Practice committee of the American Society for Reproductive Medicine.Endometriosis and infertility[J].Fertil Steril,2006,86(5Suppl1):156-160.
[15] Mishra VV, Gaddagi RA, Aggarwal R,et al.Prevalence; Characteristics and Management of Endometriosis Amongst Infertile Women: A One Year Retrospective Study.J Clin Diagn Res,2015, 9(6): QC01-QC03.
[16] Nayak PK, Mahapatra PC, Mallick J,et al.Role of diagnostic hystero-laparoscopy in the evaluation of infertility: A retrospective study of 300 patients.J Hum Reprod Sci, 2013,6(1): 32-34.
[17] Homer HA, Li TC, Cooke ID. The septate uterus: A review of management and reproductive outcome. Fertil Steril, 2000,73:1-14.
[责任编辑:董 琳]
Clinical analysis of hysteroscopy combined with laparoscopy in the diagnosis and treatment of 461 infertility women
WUYUN Tana1,LIU Lingling2,ZHAO Yong2,WANG Aiming2*
1.Instituteofclinicalmedicine,InnerMongoliaUniversityfortheNationalities,Tongliao,InnerMongolia, 028000; 2.Reproductivecenter,NavyPLAGeneralHospital,Beijing
*Correspondingauthor:WANGAiming,Email:one_army@sina.com
Objective: To explore the value of hysteroscopy combined with laparoscopy for diagnosis and treatment of infertility women, and to study the relation factors on pregnancy outcomes of women after surgery. Methods: A retrospective study was conducted based on data of 461 infertility women from January, 2008 to May, 2014 at Navy General Hospital, who were all diagnosed and treated by hysteroscopy combined with laparoscopy. The data about pregnancy and pregnant outcomes of these women after surgery were collected by telephone. Pregnancy rates of women with primary infertility or secondary infertility were compared. And influence of age or pelvic adhesion on pregnancy outcome was also analyzed. Results: Among 461 women, there were 225 (48.8%) cases with primary infertility and 236 cases (51.2%) with secondary infertility. The main reasons of infertility included pelvic adhesions (251 cases, 54.5%), fallopian tube obstruction (234 cases, 50.8%), and endometriosis (157 cases, 34.1%). The rate of pelvic adhesions, fallopian tube obstruction and intrauterine adhesion of women with secondary infertility were higher than those of women with primary infertility. Genital tuberculosis only occurred in women with primary infertility (P<0.05). Other infertility reasons had no significant difference between women with primary infertility and women with secondary infertility. The total rate of follow-up after surgical was 85.25%. Rate of spontaneous conception after surgery was 50.6%, rate of pregnancy in women with primary infertility was 49.5%, and that in women with secondary infertility was 51.8%. Rate of term delivery was 43.8%. Pregnancy mainly occurred within 1 year after surgery. Pregnancy rate of women in 20 to 30 years old women was 54.9%, which was significant higher than that of women in 31 to 43 years old (45.5%)(P<0.05). Pregnancy rates of women with non pelvic adhesions, mild pelvic adhesions, moderate adhesions or severe adhesions was 61.5%、54.8%、40.6% and 18.9%, respectively. Both rate of pregnancy and term delivery of women with no pelvic adhesions were significant higher than those of women with pelvic adhesions (P<0.05). Rate of pregnancy and rate of term delivery in women with mild or moderate pelvic adhesions was significant higher than those of women with severe adhesions(P<0.05). However, there was no different between women with mild pelvic adhesions and women with moderate adhesions (P>0.05). Conclusion: Hysteroscopy combined with laparoscopy can evaluate the reason of infertility directly, and can deal with reasons for infertility women at the same time. Treatment by hysteroscopy combined with laparoscopy can short operation time, reduce trauma and increases rate of pregnancy and term delivery for infertility women. Hysteroscopy combined with laparoscopy has great valuable on diagnosing and treatment of infertility women.
Hysteroscopy combined with laparoscopy; Infertility women; Rate of pregnancy; Rate of term delivery
2015-11-16
2016-01-08
10.3969/j.issn.1004-8189. 2016.04
*通讯作者:one_army@sina.com