心房颤动患者血清可溶性基质裂解素2表达水平及其与左心房重构的关系研究
2016-07-25刘先霞
赵 勇,刘先霞
·论著·
心房颤动患者血清可溶性基质裂解素2表达水平及其与左心房重构的关系研究
赵 勇,刘先霞
570311海南省海口市,海南省农垦总医院心内科
【摘要】目的探讨左心室收缩功能正常的心房颤动患者血清可溶性基质裂解素2(sST-2)水平及其与左心房重构的关系。方法选取2013年度海南省农垦总医院收治的年龄<75岁的左心室收缩功能正常的阵发性或持续性心房颤动患者86例作为试验组,另选取同期在本院体检健康,且性别和年龄与试验组相匹配者86例作为对照组。收集受试者人口学资料和临床基线资料,心脏超声测量左心室舒张末期内径、室间隔厚度,并计算左心室射血分数(LVEF)和左心房容积指数(LAVI)。采用酶联免疫吸附试验(ELISA)法检测受试者血清sST-2水平。采用单因素及多因素Logistic回归分析影响心房颤动发生的因素;采用Spearman相关分析和多元线性回归分析sST-2水平与基线资料的相关性。结果对照组和试验组性别、年龄、体质指数(BMI)、吸烟率、白细胞计数、估算肾小球滤过率(eGFR)、左心室舒张末期内径、室间隔厚度及LVEF比较,差异均无统计学意义(P>0.05);试验组LAVI和sST-2水平均高于对照组(P<0.05)。阵发性心房颤动患者病程、LAVI和sST-2水平均低于持续性心房颤动患者(P<0.05)。多因素Logistic回归分析结果显示,LAVI和sST-2水平是影响心房颤动发生的独立危险因素(P<0.05)。Spearman相关分析结果显示,心房颤动患者年龄、病程和LAVI与sST-2水平呈正相关(r=0.188、0.350、0.404,P<0.05)。多元线性回归分析结果显示,LAVI是影响心房颤动患者sST-2水平的因素(P<0.05)。结论左心室收缩功能正常的心房颤动患者血清sST-2水平明显升高,在持续性心房颤动患者中更加明显,且其是心房颤动发生的危险因素,与LAVI独立相关。
【关键词】心房颤动;可溶性基质裂解素2;左心房容积指数
赵勇,刘先霞.心房颤动患者血清可溶性基质裂解素2表达水平及其与左心房重构的关系研究[J].中国全科医学,2016,19(20):2426-2429,2434.[www.chinagp.net]
ZHAO Y,LIU X X.Expression of serum souble ST-2 in patients with atrial fibrillation and its correlation with left atrial pemodeling[J].Chinese General Practice,2016,19(20):2426-2429,2434.
心房颤动是临床中最常见的可导致严重并发症的心律失常[1],发现和确定心房颤动发生与危险分层的生物学标志物具有重要意义[2]。基质裂解素2(ST-2)作为白介素(IL)-1受体家族成员,在体内分别以跨膜蛋白形式(ST-2L)和可溶性蛋白形式(sST-2)存在,通过与其配体IL-33结合参与调控组织纤维化作用[3]。早期研究发现,当心肌细胞或心肌成纤维细胞受到机械牵拉或应变力变化时,ST-2和IL-33表达明显增加[4],两者结合发挥抗肥厚和抗纤维化作用。而sST-2与IL-33结合作为IL-33/ST-2通路开关发挥与ST-2L相反的作用。当sST-2过度分泌时,ST-2L的有益作用被抵消,促进心肌细胞肥厚和纤维化。大量研究发现,sST-2水平升高与心力衰竭明显相关,是心功能不全患者预后不良的独立危险因子[5-6]。但sST-2水平与心房颤动和心房纤维化的关系目前还不清楚。本研究拟探讨血清sST-2水平与左心室收缩功能正常的心房颤动患者的关系,为临床中应用sST-2作为心房颤动的生物学标志物积累资料。
1对象与方法
1.1研究对象选取2013年度海南省农垦总医院收治的年龄<75岁的左心室收缩功能正常的阵发性或持续性心房颤动患者86例(试验组),其中阵发性心房颤动49例,持续性心房颤动37例。阵发性心房颤动定义为心房颤动在7 d内自行终止,持续性心房颤动定义为心房颤动发作持续7 d及以上,或者需要药物/直流电复律转律。排除高血压、糖尿病、中重度心脏瓣膜病、先天性心脏病、酗酒史、甲状腺功能异常、冠心病、肾功能不全、自身免疫性疾病、近期感染、妊娠和进行心房颤动射频消融术者;左心房直径>55 mm,或心功能不全者。另选取同期在本院体检健康,且性别和年龄与试验组相匹配者86例作为对照组。受试者入选前均被详细告知试验目的、风险和益处并签署知情同意书,本研究所有流程符合赫尔辛基宣言临床试验准则,且获得本院伦理委员会批准。
1.2资料收集收集所有受试者人口学资料和临床基线资料。其中人口学资料包括性别、年龄、体质指数(BMI)和吸烟史,临床基线资料包括病程、白细胞计数和估算肾小球滤过率(eGFR)。采用德国Philips IE33超声显像仪评估左心房结构和左心室功能,超声探头为S4超声探头,探头频率为2.5 MHz,受试者取左侧卧位,平静呼吸,固定二维左心室长轴切面图像后,测量左心室舒张末期内径、室间隔厚度,并计算左心室射血分数(LVEF)。使用双平面面积-长度法计算左心房容积(LAV),左心房容积指数(LAVI)=LAV/体表面积,体表面积=0.006 1×身高+0.012 8×体质量-0.152 9。
1.3血清sST-2水平测定采集受试者晨起空腹静脉血5 ml,以3 600 r/min离心5 min,分离血清,存储于-80 ℃冰箱。采用人ST-2酶联免疫吸附试验(ELISA)检测试剂盒(上海酶研生物科技有限公司)检测sST-2水平。连续稀释已知浓度的sST-2构建标准曲线,通过对数转化计算样本血清sST-2水平。

2结果
2.1对照组和试验组基线资料和临床资料比较两组受试者性别、年龄、BMI、吸烟率、白细胞计数、eGFR、左心室舒张末期内径、室间隔厚度及LVEF比较,差异均无统计学意义(P>0.05);试验组LAVI和sST-2水平均高于对照组,差异有统计学意义(P<0.05,见表1)。
2.2阵发性和持续性心房颤动患者基线资料和临床资料比较阵发性心房颤动和持续性心房颤动患者性别、年龄、BMI、吸烟率、白细胞计数、eGFR、左心室舒张末期内径、室间隔厚度、LVEF比较,差异均无统计学意义(P>0.05);阵发性心房颤动患者病程、LAVI和sST-2水平均低于持续性心房颤动患者,差异有统计学意义(P<0.05,见表2)。
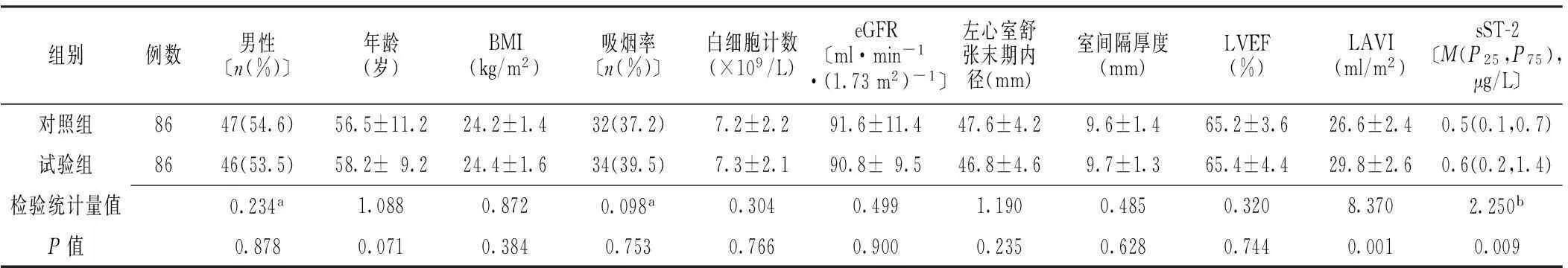
表1 对照组和试验组基线资料和临床资料比较
注:a为χ2值,b为Z值,余检验统计量值为t值;BMI=体质指数,eGFR=估算肾小球滤过率,LVEF=左心室射血分数,LAVI=左心房容积指数,sST-2=可溶性基质裂解素2
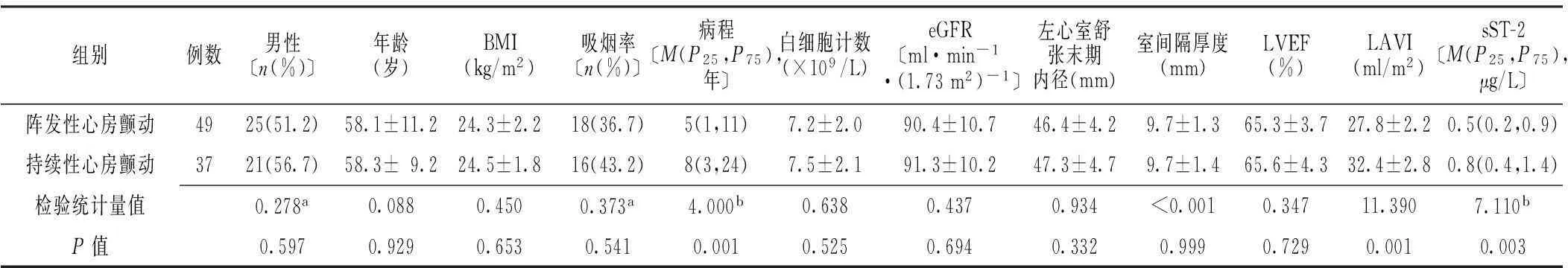
表2 阵发性和持续性心房颤动患者基线资料和临床资料比较
注:a为χ2值,b为Z值,余检验统计量值为t值
2.3单因素及多因素Logistic回归分析以是否发生心房颤动(赋值:是=1,否=0)为因变量,分别以性别(赋值:男=1,女=0)、年龄、BMI、吸烟(赋值:是=1,否=0)、白细胞计数、eGFR、左心室舒张末期内径、室间隔厚度、LVEF、LAVI和sST-2水平为自变量进行单因素Logistic回归分析,结果显示,LAVI和sST-2水平是影响心房颤动发生的因素(P<0.05,见表3)。以是否发生心房颤动为因变量,以LAVI和sST-2水平为自变量进行多因素Logistic回归分析,结果显示,LAVI和sST-2水平是影响心房颤动发生的独立危险因素(P<0.05,见表4)。
表3心房颤动发生影响因素的单因素Logistic回归分析
Table 3Univariate Logistic regression analysis on influencing factors for atrial fibrillation

因素βSEWaldχ2值OR(95%CI)P值性别<0.0010.368<0.0011.000(0.487,2.055)0.878年龄0.0240.0181.9091.025(0.990,1.060)0.167BMI0.1400.0121.3421.014(0.990,1.039)0.247吸烟-0.3320.3091.1560.718(0.392,1.314)0.282白细胞计数-0.0300.0750.1670.970(0.838,1.123)0.683eGFR-1.5381.9540.6200.215(0.005,9.897)0.431左心室舒张末期内径0.0070.1070.0051.008(0.818,1.242)0.944室间隔厚度0.0030.0040.4801.003(0.995,1.011)0.489LVEF-0.0180.0480.1390.982(0.893,1.080)0.710LAVI0.3200.8432.1101.390(1.220,1.550)0.030sST-25.1761.2496.300176.890(17.300,1829.160)0.010
表4心房颤动发生影响因素的多因素Logistic回归分析
Table 4Multivariate Logistic regression analysis on influencing factors for atrial fibrillation

因素βSEWaldχ2值OR(95%CI)P值LAVI0.320.0241.2451.384(1.193,1.601)0.006sST-2-0.1331.83412.44087.532(6.065,1265.034)0.010
2.4相关性分析及多元线性回归分析Spearman相关分析结果显示,心房颤动患者年龄、病程和LAVI与sST-2水平呈正相关(r=0.188、0.350、0.404,P<0.05)。以sST-2水平为因变量,以年龄、病程、LAVI为自变量进行多元线性回归分析,结果显示,LAVI是影响心房颤动患者sST-2水平的因素(P<0.05,见表5)。
表5sST-2水平与基线资料的相关性分析及多元线性回归分析
Table 5Correlation analysis and multivariate linear regression analysis of sST-2 level and baseline data
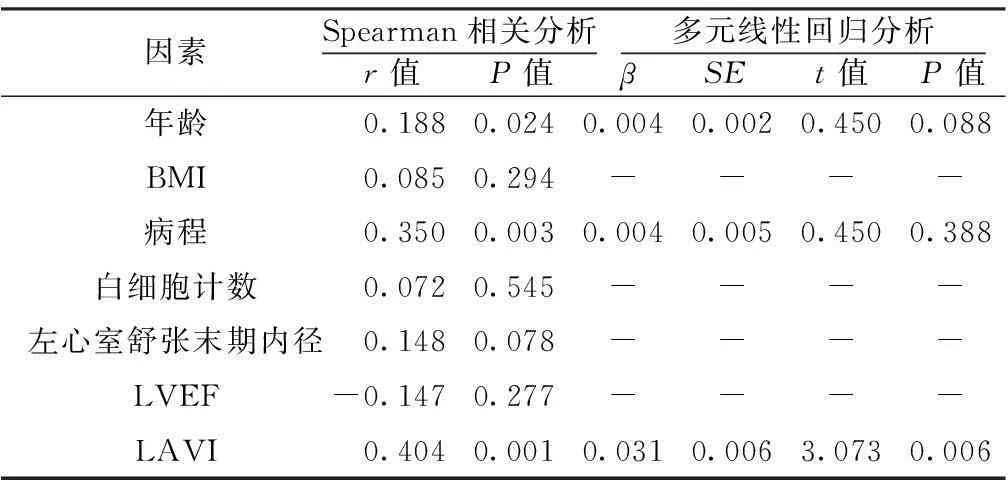
因素Spearman相关分析r值 P值 多元线性回归分析β SE t值 P值年龄0.1880.0240.0040.0020.4500.088BMI0.0850.294----病程0.3500.0030.0040.0050.4500.388白细胞计数0.0720.545----左心室舒张末期内径0.1480.078----LVEF-0.1470.277----LAVI0.4040.0010.0310.0063.0730.006
注:-表示无此数值
3讨论
研究发现,电重构、组织学重构是心房颤动发生、发展的核心机制[7]。心房纤维化是心房颤动引起电重构和组织学重构的重要标志[8-9]。无论是原发性心房颤动或继发于瓣膜病的心房颤动患者均发现胶原过度沉积现象[10-11]。sST-2作为一种新型的生物学标志物,广泛参与组织纤维化和心肌重塑。多项研究发现sST-2水平升高不仅是心力衰竭患者预后不良的重要标志,而且与心肌梗死后心肌坏死密切相关[12-13]。虽然心肌纤维化在心房颤动的发生、发展中扮演重要角色,但是,目前sST-2是否与心房颤动的发生和预后相关还不清楚。
本研究发现,左心室收缩功能正常的心房颤动患者血清sST-2水平较对照组明显升高,而且持续性心房颤动患者血清sST-2水平明显高于阵发性心房颤动患者,血清sST-2水平是影响心房颤动发生的因素。sST-2作为IL-1受体家族成员,当心肌细胞应变力增加时,刺激淋巴细胞和巨噬细胞分泌sST-2明显增加[14]。研究发现,sST-2与肺脏、心脏、皮肤及肾脏纤维化等多种纤维化疾病密切相关[15]。心脏纤维化尤其是左心房纤维化是心房颤动发生的重要原因[8]。GURSES等[16]研究发现,心脏纤维化标志物半乳糖凝集素3(Galectin-3)与心房颤动发生明显相关,尤其是持续性心房颤动患者血清Galectin-3表达水平更高。本研究采用sST-2作为心脏纤维化标志物探讨心房纤维化与心房颤动的关系,与上述研究得出一致结论。近期一项有关sST-2与Galectin-3的对比研究发现,sST-2对心力衰竭患者危险分层和预后评估的价值明显优于Galectin-3[17]。但对于心房颤动患者,sST-2与Galectin-3孰优孰劣,还需进一步的临床研究探索。
本研究结果亦显示,血清sST-2水平与LAVI独立相关。LAVI作为心房颤动的重要评价指标,经体表面积校正后,能够较好地反映心房颤动患者心房结构的变化。最新研究发现,LAVI不仅对心房颤动患者预测脑卒中和射频消融术后心房颤动复发具有重要价值[18-19],而且是评价心房颤动患者心房纤维化的重要超声学评价指标[20]。本研究发现心房颤动患者血清sST-2水平与LAVI独立相关,进一步说明sST-2在调控心房颤动患者心房纤维化中扮演重要角色。但sST-2如何调控心房颤动这一复杂的病理生理过程还需进一步研究。
总之,sST-2作为一种新型心肌纤维化标志物,与心房颤动发生明显相关。未来需进一步探讨sST-2在判断心房颤动预后、预测脑卒中发生和心房颤动消融后复发中的重要价值。本研究的不足在于,sST-2并非心脏特异标志物,可能受其他系统纤维化疾病影响。另外,本研究仅确定了sST-2与心房颤动的相关性,但不能确定两者的因果关系。
作者贡献:赵勇进行试验设计与实施、资料收集整理、撰写论文、成文并对文章负责;刘先霞进行试验实施、评估、资料收集,并进行质量控制及审校。
本文无利益冲突。
参考文献
[1]HU Y F,CHEN Y J,LIN Y J,et al.Inflammation and the pathogenesis of atrial fibrillation[J].Nat Rev Cardiol,2015,12(4):230-243.DOI:10.1038/nrcardio.2015.2.
[2]LIPPI G,CERVELLIN G,SANCHIS-GOMAR F.Galectin-3 in atrial fibrillation:simple bystander,player or both?[J].Clin Biochem,2015,48(12):818-822.DOI:10.1016/j.clinbiochem.2015.04.021.
[3]JANUZZI J L,MEBAZAA A,DI SOMMA S.ST2 and prognosis in acutely decompensated heart failure:the International ST2 Consensus Panel[J].Am J Cardiol,2015,115(7 Suppl):26B-31.DOI:10.1016/j.amjcard.2015.01.037.
[4]WEINBERG E O,SHIMPO M,DE KEULENAER G W,et al.Expression and regulation of ST2,an interleukin-1 receptor family member,in cardiomyocytes and myocardial infarction[J].Circulation,2002,106(23):2961-2966.DOI:10.1161/01.CIR.0000038705.69871.D9.
[5]KURLIANSKAYA A K,OSTROVSKY Y P,KOLIADKO M G,et al.Elevated levels of ST-2 are linked with prognostic pathomorphological parameters of heart fibrosis in patients with severe heart failure[J].Eur J Heart Fail,2014,16:237.
[6]PASSINO C,BARISON A,VERGARO G,et al.Markers of fibrosis,inflammation,and remodeling pathways in heart failure[J].Clin Chim Acta,2015,443:29-38.DOI:10.1016/j.cca.2014.09.006.
[7]SCHOTTEN U,VERHEULE S,KIRCHHOF P,et al.Pathophysiological mechanisms of atrial fibrillation:atranslational appraisal[J].Physiol Rev,2011,91(1):265-325.DOI:10.1152/physrev.00031.2009.
[8]DACCARETT M,BADGER T J,AKOUM N,et al.Association of left atrial fibrosis detected by delayed-enhancement magnetic resonance imaging and the risk of stroke in patients with atrial fibrillation[J].J Am Coll Cardiol,2011,57(7):831-838.DOI:10.1016/j.jacc.2010.09.049.
[9]BENITO B,GAY-JORDI G,SERRANO-MOLLAR A,et al.Cardiac arrhythmogenic remodeling in a rat model of long-term intensive exercise training[J].Circulation,2011,123(1):13-22.DOI:10.1161/CIRCULATIONAHA.110.938282.
[10]FRUSTACI A,CHIMENTI C,BELLOCCI F,et al.Histological substrate of atrial biopsies in patients with lone atrial fibrillation[J].Circulation,1997,96(4):1180-1184.DOI:10.1161/01.CIR.96.4.1180.
[11]BOLDT A,WETZEL U,LAUSCHKE J,et al.Fibrosis in left atrial tissue of patients with atrial fibrillation with and without underlying mitral valve disease[J].Heart,2004,90(4):400-405.DOI:10.1136/hrt.2003.015347.
[12]WEIR R A,MILLER A M,MURPHY G E,et al.Serum soluble ST2:apotential novel mediator in left ventricular and infarct remodeling after acute myocardial infarction[J].J Am Coll Cardiol,2010,55(3):243-250.DOI:10.1016/j.jacc.2009.08.047.
[13]KY B,FRENCH B,MCCLOSKEY K,et al.High-sensitivity ST2 for prediction of adverse outcomes in chronic heart failure[J].Circ Heart Fail,2011,4(2):180-187.DOI:10.1161/CIRCHEARTFAILURE.110.958223.
[14]COGLIANESE E E,LARSON M G,VASAN R S,et al.Distribution and clinical correlates of the interleukin receptor family member soluble ST2 in the Framingham Heart Study[J].Clin Chem,2012,58(12):1673-1681.DOI:10.1373/clinchem.2012.192153.
[15]高巧艳,李明才,李燕,等.IL-33/ST2信号通路在纤维化疾病中的作用[J].中国病理生理杂志,2013,29(9):1712-1717.DOI:10.3969/j.issn.1000-4718.2013.09.032.
GAO Q Y,LI M C,LI Y,et al.Role of IL-33/ST2 signaling pathway in fibrosis diseases[J].Chinese Journal of Pathophysiology,2013,29(9):1712-1717.DOI:10.3969/j.issn.1000-4718.2013.09.032.
[16]GURSES K M,YALCIN M U,KOCYIGIT D,et al.Effects of persistent atrial fibrillation on serum galectin-3 levels[J].Am J Cardiol,2015,115(5):647-651.DOI:10.1016/j.amjcard.2014.12.021.
[17]BAYES-GENIS A,DE ANTONIO M,VILA J,et al.Head-to-head comparison of 2 myocardial fibrosis biomarkers for long-term heart failure risk stratification:ST2 versus galectin-3[J].J Am Coll Cardiol,2014,63(2):158-166.DOI:10.1016/j.jacc.2013.07.087.
[18]KIM T W,JUNG S W,SONG I U,et al.Left atrial dilatation is associated with severe ischemic stroke in men with non-valvular atrial fibrillation[J].J Neurol Sci,2015,354(1/2):97-102.DOI:10.1016/j.jns.2015.05.008.
[19]COSTA F M,FERREIRA A M,OLIVEIRA S,et al.Left atrial volume is more important than the type of atrial fibrillation in predicting the long-term success of catheter ablation[J].Int J Cardiol,2015,184:56-61.DOI:10.1016/j.ijcard.2015.01.060.
[20]SONMEZ O,ERTEM F U,VATANKULU M A,et al.Novel fibro-inflammation markers in assessing left atrial remodeling in non-valvular atrial fibrillation[J].Med Sci Monit,2014,20:463-470.DOI:10.12659/MSM.890635.
(本文编辑:贾萌萌)
Expression of Serum Souble ST-2 in Patients With Atrial Fibrillation and Its Correlation With Left Atrial Remodeling
ZHAOYong,LIUXian-xia.
DepartmentofCardiology,HainanProvincialNongkenGeneralHospital,Haikou570311,China
【Abstract】ObjectiveTo investigate the expression of serum souble ST-2(sST-2)in atrial fibrillation(AF)patients with normal left ventricular systolic function and its correlation with left atrial remodeling.MethodsWe enrolled 86 paroxysmal or persistent AF patients with normal left ventricular systolic function aged <75 who received treatment in Hainan Provincial Nongken General Hospital in 2013 as trial group,and enrolled 86 healthy matched in gender and age who received physical examination in the same period in the hospital as control group.Demographic data and clinical data of the subjects were collected.We measured left ventricular end diastolic dimension and interventricular septal thickness using cardiac uhrasonography,and calculated LVEF and LAVI.ELISA was performed to determine the serum sST-2 level of the subjects.Univariate and multivariate Logistic regression analysis were performed to identify the risk factors for AF,and Spearman correlation analysis and multiple linear regression analysis were conducted to investigate the correlation between sST-2 level and baseline data.ResultsControl group and trial group were not significantly different in gender,age,BMI,smoking rate,WBC,eGFR,left ventricular end diastolic dimension,interventricular septal thickness and LVEF(P>0.05);trial group was higher than control group in LAVI and sST-2 level(P<0.05).Paroxysmal AF patients had shorter disease course and lower LAVI and sST-2 level than persistent AF patients(P<0.05).Multivariate Logistic regression analysis showed that LAVI and sST-2 level were risk factors for AF(P<0.05).Spearman correlation analysis showed that age,length of disease course and LAVI had positive correlation with sST-2 level(r=0.188,0.350,0.404,P<0.05).Multiple linear regression analysis showed that LAVI was an influencing factor for the sST-2 level of AF patients(P<0.05).ConclusionAF patients with normal left ventricular systolic function see obvious elevation in serum sST-2 level,especially for patients with persistent AF.Serum sST-2 level is a risk factor for AF and is independently correlated with LAVI.
【Key words】Atrial fibrillation;Soluble ST-2;Left atrial volume index
通信作者:赵勇,570311 海南省海口市,海南省农垦总医院心内科;E-mail:zhaoyong19771@163.com
【中图分类号】R 541.75
【文献标识码】A
DOI:10.3969/j.issn.1007-9572.2016.20.014
(收稿日期:2015-07-31;修回日期:2016-01-29)
