肝硬化门静脉高压性外周血细胞减少与手术预后
2016-05-25吕云福韩晓玉吴鸿飞常顺伍邱庆安
吕云福 韩晓玉 吴鸿飞 常顺伍 邱庆安
·论 著·(门静脉高压症外科专题)
肝硬化门静脉高压性外周血细胞减少与手术预后
吕云福 韩晓玉 吴鸿飞 常顺伍 邱庆安
目的 探讨肝炎后肝硬化门静脉高压性脾肿大病人外周血细胞减少的构成比及对手术预后的影响。方法 研究1991年1月至2015年6月笔者医院收治肝炎后肝硬化门静脉高压性脾肿大病人并发外周血细胞减少376例的临床资料,并将外周血细胞减少进行分度,比较它们的预后。结果 并发单种血细胞减少者占30.1%(113/376),两种血细胞减少者占35.9%(135/376),三种血细胞均减少者占34.0%(128/376)。全组均行脾脏切除+门奇断流术,行分流术58例(15.4%)。单种血细胞减少与多种血细胞减少的手术预后比较差异有统计学意义(P<0.05),在376例血细胞减少中,血小板计数(PLT)减少与白细胞计数减少、红细胞计数减少的手术预后比较差异有统计学意义(P<0.05)。以PLT减少为主,将血细胞减少分为轻、中、重三度,分别给予<2分、2~3分和>3分进行病例统计分析,其预后差异也有统计学意义(P<0.05)。结论 外周血细胞减少对手术预后有一定影响,单种血细胞减少的手术预后明显优于多种血细胞减少,轻度血细胞减少的预后明显优于重度血细胞减少,血细胞减少越多越严重、预后越差。
肝硬化门静脉高压症;外周血细胞减少;分度;手术预后
肝炎后肝硬化门静脉高压性脾肿大病人并发严重消化道出血,严重脾功能亢进和肝癌时,通常需要手术治疗,影响手术预后的因素尽管有多种[1],但外周血细胞减少是一种不可忽视的因素。外周血细胞减少是指入院后第一次从外周静脉血中抽出的血液,细胞计数低于正常检测值,即白细胞计数(WBC)<4.0×109/L、红细胞计数(RBC)<3.5×1012/L和血小板计数(PLT)<100×109/L称为血细胞减少。本文研究了1991年1月至2015年6月笔者医院收治肝炎后肝硬化门静脉高压性脾肿大病人376例的临床资料,就其对手术预后的影响进行分析,现报告如下。
资料与方法
一、临床资料
在376例中,男性257例,女性119例,男女之比为2.2∶1。年龄5~79岁,中位年龄43岁。全组均为肝炎后肝硬化、脾脏普遍增大,B超或CT测量脾脏大小平均为224 mm×159 mm×95 mm。上消化道造影或胃镜检查均显示,食管下段和胃底均有中、重度静脉曲张,76例(20.2%)因消化道出血而入院,179例(47.6%)既往有出血史。全组经输血,补充已缺少的血液有形成分后,行脾切除术,同时行贲门周围血管离断术376例(附加脾肾静脉分流58例)。
二、手术预后定义
手术预后主要有痊愈、好转和死亡三种。痊愈是指腹水、腹胀及出血症状消失,减少的血细胞开始上升并接近正常值,肝脏功能改善,术后无严重并发症,能安全出院;死亡是指术后住院期间死亡,包括病情危重,病人家属要求出院后1周内的死亡;否则为好转。
三、统计学分析
运用SPSS(18.0版)统计软件,单因素分析采用卡方检验,多单因素分析采用多元线性回归处理,P<0.05表示差异有统计学意义。
结 果
本文376例中,单种血细胞减少占30.1%(113/376),两种血细胞减少占35.9%(135/376),三种血细胞均减少占34.0%(128/376)。单种血细胞减少构成比及治疗结果比较见表1,结果显示仅RBC减少组组间比较差异有统计学意义(P<0.05);其余各组组间比较差异无统计学意义(P>0.05)。
单种血细胞减少与两种血细胞减少的疗效比较,差异有统计学意义(χ2=7.446,P=0.024),见表2。单种血细胞减少与多种血细胞减少的疗效比较,差异也有统计学意义(χ2=7.819,P=0.02),见表3。
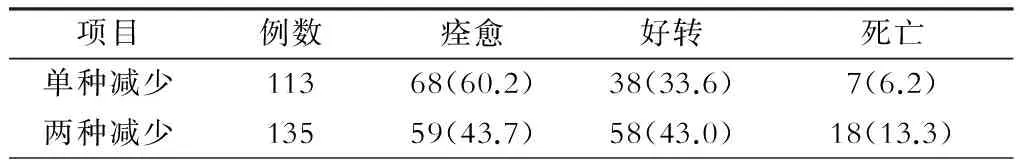
表2 单种血细胞与两种血细胞减少疗效比较[例(%)]
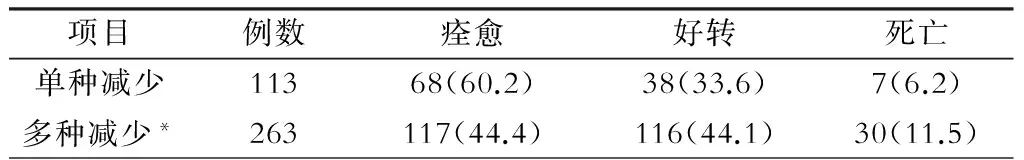
表3 单种血细胞减少与多种血细胞减少疗效比较[例(%)]
注:*指两种以上血细胞减少

表1 113例单种血细胞减少治疗结果组内比较[例(%)]

表4 376例血细胞的多元线性回归分析
于是,以PLT减少为主,同时结合单种血细胞减少疗效比较中有显著差异的RBC减少和临床经验(WBC减少),将376例血细胞减少病例进行分权、打分。PLT>50×109/L打1分,(30~50)×109/L打2分,<30×109/L打3分;RBC(3~4)×1012/L打0分,<3×1012/L打1分;WBC (2~4)×109/L打0分,<2×109/L打1分。将外周血细胞减少总分分为轻(<2分)、中(2~3分)、重(>3分)三度(表5)。
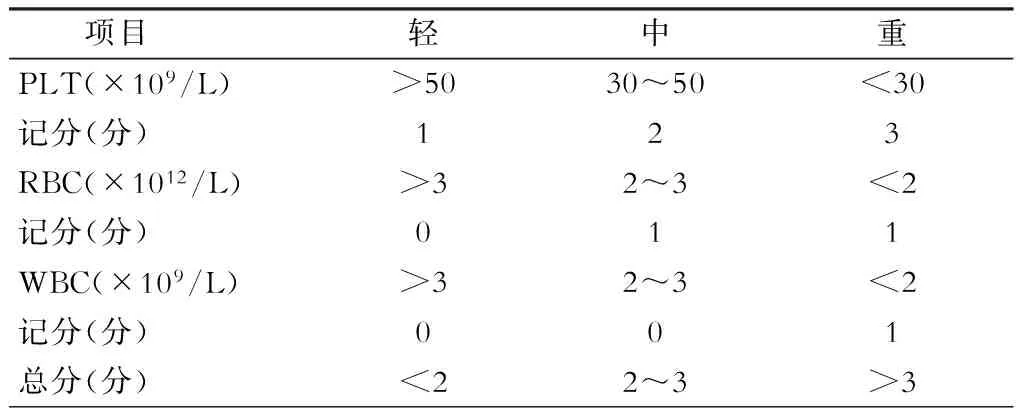
表5 外周血细胞减少(脾功能亢进)分级
不同分值对手术预后的影响见表6,三组疗效比较差异有统计学意义(χ2=10.163,P=0.034)。

表6 不同分值对治疗结果影响的比较[例(%)]
讨 论
肝炎后肝硬化门静脉高压性脾脏肿大病人并发外周血细胞减少约70%表现为多种血细胞减少,30%表现为单种血细胞减少。
从表1看,单种血细胞减少,只有RBC组内比较疗效差异有统计学意义(P<0.05)。从表2、3可知,单种血细胞减少与两种和多种血细胞减少的疗效比较差异有统计学意义(P<0.05),表明血细胞减少越多术后疗效越差。
在多种血细胞减少中,采用多元线性回归分析,发现PLT减少是影响手术疗效的主要因素(P<0.05),而RBC减少、WBC减少和Hb下降均无统计学意义,被列为非主要因素。RBC减少在单种血细胞减少组内疗效比较中有显著性差异,但在多因素中比较差异无统计学意义,可能与单种血细胞减少组样本比较小、有一定的局限性有关。WBC减少无论是单因素分析还是多因素分析,对手术预后的影响均不大,我们有2例病人WBC在1×109/L以下,术后也能顺利康复出院,这可能与术后没有遭遇严重感染有关。从理论上讲,贫血应与预后有关,而本研究无论从单因素分析还是多因素分析,差异均无统计学意义(P>0.05),可能是术前、术中注意输血,贫血得到纠正之故。PLT减少虽在单因素比较中差异无统计学意义,但随着病例数的加大,在多因素线性回归分析中却显示唯一有显著意义的主要因素。

1907年,Chauffard使用脾功能亢进这一名称[13]。1949年Doan[14]做了进一步研究,提出脾功能亢进的必备条件:①脾脏肿大;②血中有一种或数种血细胞成分减少;③骨髓正常或呈增生状态;④脾切除术后血液成分的病理性改变消失。这4点必备条件是对诊断脾功能亢进总体而言,然而肝硬化门静脉高压症病人因脾肿大本身就是门静脉高压症应具备的条件、故评价肝硬化门静脉高压症病人的脾功能亢进主要依据外周血细胞的减少和脾切除术后原减少的血细胞恢复至正常或接近正常。

合理的分度有利于评估疾病的程度;有利于表述和学术交流;有利于与病人及其家属沟通病情,减少医疗纠纷;有利于选择治疗,如系重度血细胞减少或脾功能亢进,手术切除肿大的脾脏是理想的选择;有利于术前采取措施[16],预先防范,提高治愈率。
2 Karasu Z,Gurakar A, Kerwin B,et al. Effect of transjuqular intrahepatic portosystemic shunt on thrombocytopenia associated with cirrhosis.Dig Dis Sci,2000,45:1971-1976.
3 Fadi NB,J Carlos T,Kevin D,et al.Prevalence of Peripheral Blood Cytopenias Hypersplenism)in Patients With Nonalcoholic Liver Disease. Am Coll of Gastroeterology,2000,95:2937-2939.
4 Yan F,Li W,Gao J,et al. cDN Amicoarray-based screening of differentially expressed genes in macrophages in the spleen of patients with portal Hypertension and hypersplenism. Nan Fang Yi Ke Da Xue Xue Bao,2006,26:1548-1551.
5 李路豪,党晓卫,李林,等.门静脉高压病人部分脾栓塞术后并发脾脓肿的危险因素及治疗.腹部外科,2015,28:394-398.DOI: 10.3969/j.issn.1003-5591.2015.06.005.
7 Zhang JY, Wang Y, Zhang J, et al.Risk factors associated with failure from endoscopic therapy in acute non-variceal upper gastrointestinal bleeding.Beijing Da Xue Xue Bao,2010,42:703-707.
8 Cui Y, Hei F, Long C, et al. Perioperative monitoring of thromboelastograph on hemostasis and therapy for cyanotic infants undergoing complex cardiac surgery. Artif Organs,2009,33:909-914.
9 吕云福,李新秋,黄伟炜,等.门静脉高压性脾功能亢进病人的外周血细胞变化.中华普通外科杂志,2007,22:702.
10 Matsuura T, Hayashida M, Saeki I, Taguchi T.The risk factors of persistent thrombocytopenia and splenomegaly after liver transplantation.Pediatr Surg Int,2010,26:1007-1010.
11 Johansson PI, Stensballe J.Hemostatic resuscitation for massive bleeding: the paradigm of plasma and platelets--a review of the current literature.Transfusion,2010,50:701-710.DOI:10.1111/j.1537-2995.2009.02458.x.
12 Shontz R, Karuparthy V, Temple R,et al.Prevalence and risk factors predisposing to coagulopathy in patients receiving epidural analgesia for hepatic surgery. Reg Anesth Pain Med,2009,34:308-311.DOI: 10.1097/AAP.0b013e3181ac7d00.
13 Bashour FN, Teran JC, Mullen KD. Prevalence of peripheral blood cytopenias(hypersplenism)in patients with nonalcoholic liver disease. Am J Gastroeterol,2000,95:2937-2939.
14 Doan CA.Hypersplenism. Bull N Y Acad Med,1949,25:625-650.
15 Lv Y,Han X,Gong X,et al.Grading of peripheral cytopenias caused by nonalcoholic cirrhotic portal hypertension and its clinical significance. Cell Biochem Biophys,2015,71:1141-1145.DOI: 10.1007/s12013-014-0321-x.
16 Shaz BH, Dente CJ, Nicholas J, et al.Increased number of coagulation products in relationship to red blood cell products transfused improves mortality in trauma patients.Transfusion,2010,50:493-500.DOI:10.1111/j.1537-2995.2009.02414.x.
Liver cirrhosis portal hypertension decreased peripheral blood cells and surgical outcomes
LyuYunfu,HanXiaoyu,WuHongfei,ChangShunwu,QiuQingan.
DepartmentofGeneralSurgery,HainanProvincialPeople'sHospital,Haikou570311,China
LyuYunfu,Email:yunfu_lv@126.com
Objective To investigate the constituent ratio of peripheral cytopenias in patients with splenomegaly caused by post-hepatitic cirrhotic portal hypertension and potential influence of peripheral cytopenias on prognosis. Methods Between January 1991 and June 2015, 376 cases of post-hepatitic cirrhotic portal hypertension induced splenomegaly patients associated with peripheral cytopenias, undertook surgery in our hospital, and their clinical data was reviewed. Furthermore, peripheral cytopenias and prognosis in them was graded and compared. Results Patients associated with mono-lineage, bi-lineage, and tri-lineage cytopenias, respectively accounted for 30.1% (113/376), 35.9% (135/376), and 34.0% (128/376). Significant statistical differences (P<0.05) in post-operative prognostic could be noted in patients in contrast of mono-lineage cytopenias and multi-linage cytopenias. In all patients, postoperative prognosis demonstrated significant correlation with thrombocytopenia, leukopenia and erythropenia (P<0.05). According to the severity of thrombocytopenia, cytopenia was graded as mild, medium and severe, referring to <2 grade,2-3 grade and >3 grade respectively. The prognosis revealed significant differences among three groups (P<0.05). Conclusions Peripheral cytopenias can influence postoperative prognosis in patients with splenomegaly caused by post-hepatitic cirrhotic portal hypertension. The prognosis in patients associated with mono-linage peripheral cytopenias is better than those associated with multi-linage cytopenias, and prognosis in patients associated with mild peripheral cytopenias is obviously better than those associated with severe cytopenias. Our study demonstrates the more severe the peripheral cytopenias is, the worse the prognosis is.
Liver cirrhosis portal hypertension; Peripheral cytopenias; Grading; Postoperative prognosis
海南省科技合作专项资金项目(KJHZ2015-28)
570311 海口,海南省人民医院普外中心
吕云福, Email:yunfu_lv@126.com
R657.3+4;R657.3+1
A [DOI] 10.3969/j.issn.1003-5591.2016.03.002
杨镇,裘法祖.关于门静脉高压症预后结局的研究. 腹部外科,2003,16:68-70.
10.3969/j.issn.1003-5591.2003.02.001.
2016-03-16)
