年轻患者腰椎间盘Pfirrmann分级与椎间盘膨出及突出的相关性研究
2016-05-12郑作锋李优伟张东坡毛磊
郑作锋,李优伟,张东坡,毛磊
年轻患者腰椎间盘Pfirrmann分级与椎间盘膨出及突出的相关性研究
郑作锋,李优伟*,张东坡,毛磊
[摘要]目的 通过磁共振成像,观察30岁以下腰痛患者腰椎间盘退行性改变的Pfirrmann分级特征以及相关的其他改变,并评价Pfirrmann分级与椎间盘膨出及突出的相关性。材料与方法 回顾性分析83例30岁以下因腰痛行腰椎MRI检查的患者,其中男50例,女33例,平均年龄25岁。由2名影像科医师对MR图像进行分析,观察L1~S1椎间盘信号、椎间盘形态、纤维环撕裂、椎间盘膨出、椎间盘突出、椎体终板及许莫氏结节的改变。椎间盘退行性改变采用Pfirrmann分级。观察指标的相关性分析采用Pearson多元相关分析。结果 纳入研究的椎间盘共415个,其中Pfirrmann分级Ⅰ~Ⅱ级退变322个(77.6%),Ⅲ级退变56个(13.5%),Ⅳ级退变33个(7.9%),Ⅴ级退变4个(1.0%);103个椎间盘出现膨出或突出;椎间盘膨出以L4~5椎间盘最多(42.2%),且多合并Ⅲ级退变(51.1%);椎间盘突出以L5~S1椎间盘最多(51.7%),且多合并Ⅳ级退变(46.6%);17例患者出现椎间盘后方高信号区(HIZ),且均位于L4~5、L5~S1椎间盘水平;3例患者出现终板退变。多元相关分析结果显示Pfirrmann Ⅲ级退变与椎间盘膨出有明显相关性(r=0.972;P=0.006),与椎间盘突出无明显相关性(r=0.639;P=0.245);Pfirrmann Ⅳ级退变与椎间盘突出(r=0.999,P=0.000)及HIZ (r=0.919,P=0.028)有明显相关性,与椎间盘膨出无明显相关性(r=0.769,P=0.128)。HIZ与椎间盘膨出(r=0.919,P=0.027)及突出(r=0.935,P=0.020)均有相关性。结论 腰椎MRI成像能够清晰显示年轻患者椎间盘早期退行性改变的不同病理阶段;Pfirrmann Ⅲ退变与Pfirrmann Ⅳ级退变分别与椎间盘膨出和椎间盘突出有相关性;年轻患者应及早发现椎间盘早期退变,以对临床评价提供更有价值信息。
[关键词]椎间盘移位;磁共振成像;年轻人
作者单位:
北京市垂杨柳医院放射科,北京100022
李优伟,E-mail: lywhot@sohu.com
接受日期:2016-02-15
郑作锋, 李优伟, 张东坡, 等. 年轻患者腰椎间盘Pfirrmann分级与椎间盘膨出及突出的相关性研究. 磁共振成像, 2016, 7(3): 203-208.
椎间盘退行性改变引起的下腰痛较常见,随年龄的增长和生活方式的改变,其发病率逐渐增高,也越来越年轻化。既往文献中对老年人研究较多,而对年轻患者的研究较少。有文献表明,30岁以前椎间盘即可发生退行性改变,而早期的椎间盘退变可以加速腰椎退变的进程[1]。Pfirrmann分级可以较好的反应椎间盘早期退变的过程,而椎间盘后方高信号区(high intensity zone,HIZ)通常提示纤维环撕裂,并与椎间盘膨出、突出形成下腰痛的主要原因。本研究以年轻人为对象,通过MRI观察腰椎间盘早期退行性改变的影像学特征,同时评价椎间盘Pfirrmann分级与HIZ、椎间盘膨出和突出的相关性,以引起临床对早期退行性改变的重视。
1 材料与方法
1.1 一般资料
回顾性分析2013年1月至2015年4月因下腰痛于我院行腰椎MRI检查的患者,共91例。入选标准:(1)患者因下腰痛就诊;(2)年龄小于30岁;(3)既往无明确腰部疾病病史,包括先天性病变、肿瘤、骨折、感染及手术病史;(4)能够配合完成MRI检查。其中有8例因不符合入选标准排除在外(4例为腰椎压缩骨折,1例为脊髓脊膜膨出,1例为腰椎结核、1例为术后蛛网膜粘连,1例为腰背部脓肿),最终入组83例,其中男50例,女33例,年龄16~30岁,平均年龄25岁。
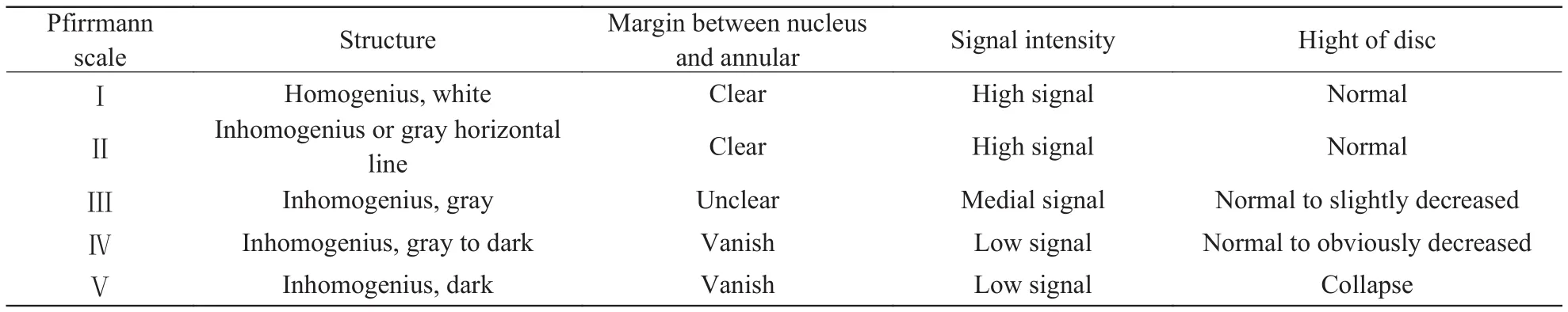
表1 Pfirrmann分级标准Tab. 1 Pfirrmann grading scale standard
1.2 检查方法
采用GE Signa Excite 1.5 T超导磁共振扫描仪,扫描序列及参数:矢状面T2 FRFSE TR 2420 ms,TE 112 ms,层厚5 mm;矢状面T1 FSE TR 460 ms,TE 11 ms 层厚5 mm;矢状面FS T2 FRFSE TR 2740 ms,TE 102 ms,层厚5 mm;横断面T2 FRFSE TR 4520 ms,TE 110 ms。
1.3 影像评价
扫描所得图像由2名有经验的放射科医师独立阅片,观察内容包括以下方面:(1)椎间盘信号及形态:在T2WI矢状面观察,椎间盘退变的分级采用Pfirrmann分级(Ⅰ~Ⅴ)(分级标准见表1)[2]。(2)椎间盘膨出及突出:椎间盘膨出定义为椎间盘在各个方向上大于椎体终板,向周围均匀膨隆,无局限性改变;椎间盘突出定义为局限性椎间盘组织移位超出椎间隙范围[3]。(3)椎间盘后方HIZ:结合T2WI及T2WI脂肪抑制序列矢状面像、T2WI轴面像观察,表现为椎间盘后方条状高信号。(4)椎体终板:按Modic等[4]得终板标准进行分型,正常:椎体终板信号正常,无改变;Ⅰ型:T1WI终板及邻近骨质为低信号,T2WI相对正常终板为高信号;Ⅱ型:T1WI比正常骨髓信号高,T2WI信号也升高,但不如T1 WI明显;Ⅲ型:T1 WI、T2WI信号均降低。(5)许莫氏结节:在T1WI及T2WI矢状面像观察。(6)其他发现病变结合图像做相应记录。
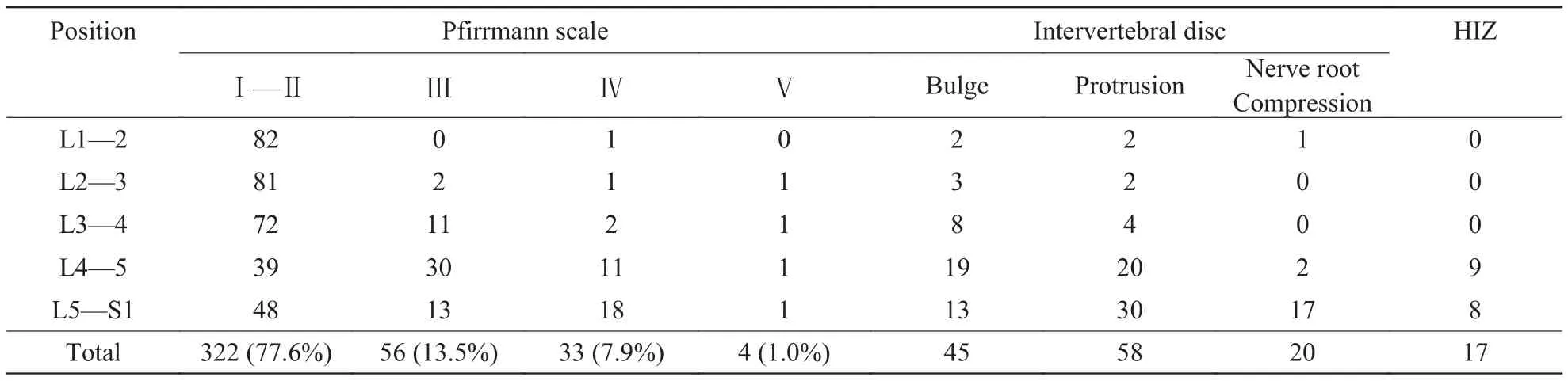
表2 Pfirrmann分级、椎间盘改变及HIZ在各椎间盘节段的分部Tab. 2 The distribution of Pfirrmann grading scale,intervertebral disc changes and HIZ in different levels of lumbar discs
2名医师记录结果一致的作为最终结果,不一致的由2名医师讨论,确定最终结果。
1.4 统计学处理
使用SPSS 22.0统计分析软件,采用Pearson多元相关方法分析腰椎不同退行性改变之间的相关性,以P<0.05为差异有统计学意义。
2 结果
2.1 影像学观察结果
83例患者,共415个椎间盘纳入最终结果。其中Pfirrmann分级Ⅰ~Ⅱ级退变322个(77.6%),Ⅲ级退变56个(13.5%),Ⅳ级退变33个(7.9%),Ⅴ级退变4个(1%);103个椎间盘出现膨出或突出;椎间盘膨出以L4~5椎间盘最多(42.2%),且多合并Ⅲ级退变(51.1%);椎间盘突出以L5~S1椎间盘最多(51.7%),且多合并Ⅳ级退变(46.6%); 17例患者出现HIZ,且均位于L4~5、L5~S1椎间盘水平;3例患者出现终板退变,位于L4、L5、S1椎体;12个椎体出现许莫氏结节,其腰椎各个椎体均有分布;2例患者出现腰椎滑脱。Pfirrmann分级、椎间盘改变及HIZ具体结果见表2,其影像学表现见图1~3,许莫氏结节观察结果见表3,椎体终板的观察结果见表4。
2.2 Pfirrmann分级、椎间盘膨出、椎间盘突出及HIZ的相关性分析
将Pfirrmann分级、椎间盘膨出、椎间盘突出及HIZ在L1/2~L5/S1五个椎间盘节段分别所累及的椎间盘数量作为观察指标做多元相关分析,分析结果显示:Pfirrmann Ⅲ级退变与椎间盘膨出有明显相关性(r=0.972,P=0.006),而与椎间盘突出无明显相关性(r=0.639,P =0.245);Pfirrmann Ⅳ级退变与椎间盘突出(r=0.999,P=0.000)及HIZ (r=0.919,P=0.028)有明显相关性,而与椎间盘膨出无明显相关性(r=0.769,P=0.128)。HIZ与椎间盘膨出(r=0.919,P=0.027)及突出(r=0.935,P=0.020)均有相关性。具体结果见图4。

表3 许莫氏结节在各椎体节段的分部Tab. 3 The distribution of Schmorl’s nodes in different levels of the lumbar
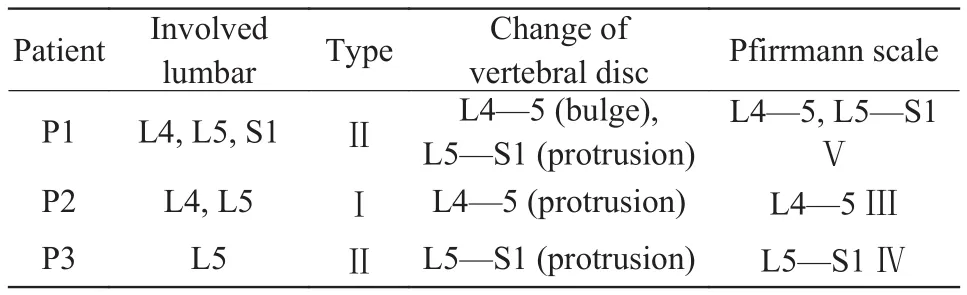
表4 3例患者(P1~P3)终板退变Tab. 4 The distribution of the Modic change in three patients (P1—P3)
3 讨论
儿童及青少年下腰痛的发病率随年龄增长逐步上升。目前国内外文献对椎间盘退行性改变的关注对象多为老年人,而对年轻患者关注较少。Zitting等[5]对青少年椎间盘突出的流行病学调查表明:对12 058名新生儿做随访观察,结果显示,15岁以前无一名观察对象因椎间盘突出住院,年龄增加至20岁时数量增加至0.1%~0.2%,有明显上升趋势;到28岁时,9.5%的男性和4.2%的女性因椎间盘突出入院。所以,年轻人腰椎退行性改变应当引起重视。诸多研究表明,现有的基础病变(微小病变,早期退行性改变等)会加速椎间盘退行性改变的进展[6-7]。所以及早发现椎间盘早期的退行性改变,或许对疾病的发展及预后有积极作用。因此,本研究以30岁以下人群作为研究对象,通过MRI成像观察腰椎早期退行性改变的不同方面,并探讨椎间盘早期的退行性改变与椎间盘膨出及突出的关系。
3.1 髓核退变与椎间盘膨出、突出的关系
髓核的退行性改变与腰痛有密切关系。髓核组织中含有大量蛋白聚糖与Ⅱ型胶原结合形成的网眼状结构,其内可储存大量水分子,以维持髓核内水合离子浓度的稳定性,保持髓核的凝胶状态及弹性,为椎间盘提供抵抗压缩的载荷能力[8]。所以,髓核的退行性改变通常发生较早。MRI以独特的成像优势,通过髓核内部水分的改变,可以清晰显示退行性变化的动态过程。目前存在多个以MRI为基础的椎间盘退变分级系统,其中Pfirrmann评分系统作为临床及科研被广泛接受[2-9],它可以较好的反应椎间盘早期的退行性改变。我们通过对415个椎间盘的观察发现,椎间盘处于Ⅰ~Ⅱ级退变者占77.6%,且L1/2~L3/4椎间盘占多数,提示年轻患者L1/2~L3/4节段椎间盘相对处于基本正常或水分刚刚开始丢失阶段;Ⅲ~Ⅳ级退变占21.4%,且大部分(69.9%)发生于L4~5、L5~S1椎间盘,提示髓核内水分丢失严重的区域位于L4~5、L5~S1椎间盘节段,部分髓核开始出现压缩改变;Ⅴ级退变少见,提示严重的髓核退变发生较少。因此,对于年轻患者而言,大部分椎间盘处于相对正常状态,退变相对严重的区域位于L4~5、L5~S1椎间盘,并处于Ⅲ~Ⅳ级退变这一关键时期。从中我们推测椎间盘早期退变始于L4~5、L5~S1椎间盘,并且年轻患者多处于退变的进展中,而未达到晚期的退变。
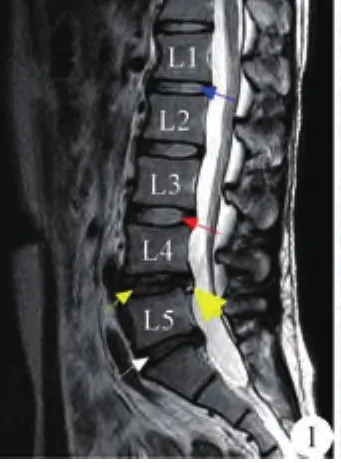
图1 男,29岁。L3~4椎间盘为Pfirrmann分级Ⅰ级,椎间盘为均匀高信号,髓核与纤维环分界清楚(红色箭头);L1~2椎间盘为Ⅱ级,椎间盘内出现横行低信号带,但髓核与纤维环边界清楚(蓝箭头);L4~5椎间盘为Ⅲ级,髓核信号为灰色,与纤维环分界不清,但高度无明显变化(黄色箭头);L5~S1椎间盘为Ⅳ级,髓核信号为灰色,椎间盘高度明显减低(白色箭头)。其中L4~5椎间盘后方可见HIZ(黄色粗箭头)Fig. 1 The pfirrmann grading scale of a 29-year-old male patient. L3—4 intervertebral disc shows uniform high signal intensity with a clear margin between the nucleus and annular (gradeⅠ). L1—2 intervertebral disc shows a horizontal low intensity band with a clear margin between the nucleus and annular (gradeⅡ). L4—5 intervertebral disc shows slightly low signal intensity with unclear margin between nucleus and annular and a normal interverteral height (gradeⅢ). L5—S1 intervertebral disc shows low signal intensity with abnormal intervertebral height (grade Ⅳ). A HIZ can be seen in the L4—5 level.
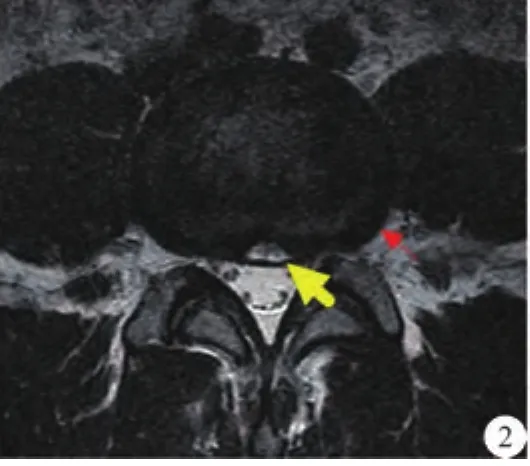
图2 同一患者横断面显示L4~5椎间盘后方HIZ(黄色粗箭头)。同时显示该椎间盘周围均匀膨出(红色细箭头),该椎间盘为Ⅲ级退变Fig. 2 Axial T2WI of the same patient shows the HIZ in L4—5 level with intervertebral disc bulge and grade Ⅲ disc degeneration.
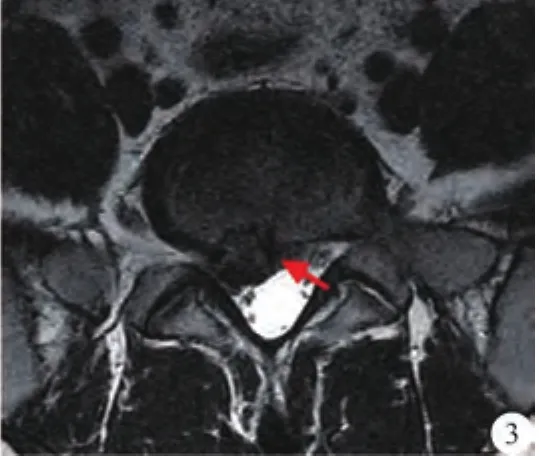
图3 同一患者L5~S1水平椎间盘突出(红色箭头显示为突出的髓核),该椎间盘为Ⅳ级退变Fig. 3 Axial T2WI shows the L4—5 intervertebral discprotrution with grade Ⅳ disc degeneration.
本组纳入研究的患者中,椎间盘膨出或突出的患者占有较高比例(62/89),椎间盘膨出和突出的部位多位于L4~5、L5~S1椎间盘,且椎间盘膨出以Ⅲ级退变比例最高,椎间盘突出以Ⅳ级退变比例最高。统计结果也表明,Ⅲ级退变与椎间盘膨出有明显相关性,Ⅳ级退变与椎间盘突出有明显相关性。所以我们推测PfirrmannⅢ级、Ⅳ级退变在椎间盘整体退变的发展中起关键作用,椎间盘Ⅲ~Ⅳ级退变提示髓核内水分丢失严重,椎间盘高度开始减低,提示髓核被压缩,而使其内压增大,容易使椎间盘膨出。但本研究中并非所有突出及膨出的椎间盘处于Ⅲ、Ⅳ级退变,部分为Ⅱ级退变,说明在髓核水分刚开始丢失时即出现膨出或突出,这可能与年轻患者不适当的运动或外伤有关。
3.2 HIZ与椎间盘膨出、突出的关系
HIZ首先由Aprill等[10]提出并定义,即MRI矢状面T2WI显示腰椎间盘后方小而圆的局限性高信号区。王子轩等[11]报道,椎间盘后方HIZ发病率约占31.7%,但其研究的对象以中老年患者为主。本研究83例年轻患者中,有17例出现HIZ,约占20.4%,表明年轻患者也有相当比例出现HIZ。Peng等[12]通过研究发现HIZ区域中正常组织被紊乱的富含毛细血管的肉芽组织取代,包括纤维母细胞及新生血管,并逐渐向外扩大,证明这是机体对破裂纤维环的修复作用。诸多研究证实HIZ是诊断椎间盘原性下腰痛的重要MRI征象。Olmarker[13]研究发现,疼痛诱发试验和疼痛阻止试验可以证实,纤维环的撕裂可以引起强烈的疼痛。这些疼痛主要归因于破坏的组织和炎性组织对敏感神经的刺激,移位的髓核内部的化学物质向周围弥散,可以加剧疼痛。Videman等[14]研究发现纤维环撕裂常发生于椎间盘退变的早期,并且与髓核的快速退变有关。Schmidt等[15]数学模型表明,未完全发生退行性改变的髓核富含水分,其内水压增高,纤维环在紧张的情况下容易发生破裂。本研究中HIZ出现的部位均位于L4~5、L5~S1椎间盘,并且Pfirrmann分级均为Ⅲ~Ⅳ级,并且HIZ与椎间盘膨出、椎间盘突出均有明显相关性,因此,椎间盘膨出、突出、纤维环撕裂与椎间盘Ⅲ~Ⅳ级退变密切相关。椎间盘Ⅲ~Ⅳ级退变提示髓核内水分丢失严重,椎间盘高度开始减低,提示髓核被压缩,而使其内压增大,同时椎间盘高度的变化,使垂直压力作用于纤维环的局部,而不是均匀的分布于纤维环周围,最终导致纤维环局部破裂,而纤维环的破口,又给髓核突出提供通道,最终导致一系列事件发生。所以,髓核内部水分的丢失可能为始动因素。Carragee等[16]研究也表明,不管是人类还是动物,如果在纤维环上人为的制造裂隙,这会导致加速细胞介导的退行性改变过程。说明,早期发现纤维环撕裂并及时干预治疗,对腰椎退行性改变的发展的控制有积极意义。

图4 以L1~S1五个椎间盘阶段的数量为观察对象,结果显示:Pfirrmann Ⅲ退变与椎间盘膨出有明显相关性;Pfirrmann Ⅳ级退变与椎间盘突出及HIZ有明显相关性。HIZ与椎间盘膨出及突出均有相关性Fig. 4 The curve diagram shows the pearson correlation between different aspects associated with disc degeneration. Grade Ⅲ degeneration was correlated well with intervertebral disc bulge. Grade Ⅳ degeneration was correlated with interverteral disc protrution and HIZ and HIZ has good correlation with both disc bulge and disc protrution.
3.3 终板退变
本研究中83例患者仅有3例(3.6%)出现终板退行性改变,而文献中张文煜等[ 1 7 ]研究中纳入1681例患者,有432例患者出现终板退变,其发生率约为25.6%,本研究明显低于张的研究。说明,年轻患者终板退行性改变发生率较低。本研究中3例终板退变仅为早期的Ⅰ型和Ⅱ型退变,无Ⅲ型退变,且均发生于椎间盘膨出或突出的椎体层面,相应椎间盘退变为Ⅲ~Ⅴ级,因此推测椎体终板退行性改变可能为相对晚期的改变。
3.4 许莫氏结节
本研究中5例出现许莫氏结节,累及12个椎体,其出现的部位在各个椎体都有发生,并且与L4~5、L5~S1膨出及突出不太相符,似乎与椎间盘Pfirrmann分级之间也无明显规律可循。潘希敏等[18]研究发现许莫氏结节广泛存在于各年龄组、各退变级别的腰椎间盘中,退变级别高的腰椎间盘并不意味着容易发生许莫氏结节,相反许莫氏结节的出现会加速间盘的退变。
综上所述,对于下腰痛的年轻患者,MRI可以清晰显示腰椎间盘退变的早期特征性改变,椎间盘Pfirrmann Ⅲ~Ⅳ退变为关键阶段,可能为椎间盘膨出或椎间盘突出的前期改变,同时椎间盘后方高信号的出现也可能会加速椎间盘膨出或突出的进展,在临床工作中应当及早发现并引起重视。
参考文献[References]
[1]Sharma A, Pilgram T, Wippold FJ. Association between annular tears and disk degeneration a longitudinal study. AJNR Am JNeuroradiol, 2009, 30(3): 500-506.
[2]Fang Y, Liu LX, Li JL, et al. Prelimary study of lumbar intertebral disc degeneration with magnetic resonance spectroscopy, T2 relaxation times and apparent diffusion coefficient. Chin J Magn Reson Imaging, 2011, 2(4): 278-282.方元, 刘兰祥, 李京龙, 等. 磁共振波谱成像、T2弛豫时间、扩散加权成像对腰椎间盘退变的初步研究. 磁共振成像, 2011, 2(4): 278-282.
[3]Jin ZY. Diagnostic imaging. Beijing: People’s medical publishing house, 2011, 545-546.金征宇. 医学影像学. 北京: 人民卫生出版社, 2011, 545-546.
[4]Modic MT, Steinberg PM, Ross JS, et al. Degenerative disk disease assessment of changes in vertebral body marrow with MR imaging. Radiology, 1988, 166(1 Pt 1): 193-199.
[5]Zitting P, Rantakallio P, Vanharanta H. Cumulative incidence of lumbar disc diseases leading to hospitalization up to the age of 28 years. Spine (Phila Pa 1976), 1998, 23(21): 2337-2343.
[6]Dang L, Liu Z. A review of current treatment for lumbar disc herniation in children and adolescents. Eur Spine J, 2010, 19(2): 205-214.
[7]Kumar R, Kumar V, Das NK, et al. Adolescent lumbar disc disease: findings and outcome. Childs Nerv Syst, 2007, 23(11): 1295-1299.
[8]Chen W, Yang SH, Lin SZ, et al. Expression of matrix aggrecanase 2 and a tissue inhibitor of metalloproteinases in degenerated intervertebral disc. Chin J Physical Med Rehabilit, 2014, 36(1): 21-24.陈微, 杨少华, 林世州, 等. 蛋白聚糖酶2与金属蛋白酶组织抑制剂3在腰椎间盘髓核退变中的表达及意义. 中华物理医学与康复杂志, 2014, 36(1): 21-24.
[9]Pfirrmann CW, Metzdorf A, Zanetti M, et al. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976), 2001, 26(17): 1873-1878.
[10]Aprill C, Bogduk N. High-intensity zone: a diagnositic sign of painful lumbar disc on magnetic resonance imaging. Br J Radiol, 1992, 65(773): 361-369.
[11]Wang ZX, Hu YG, Chen XM. Development and distribution of high-intensity zone in lumbar disc. Orthop J Chin, 2008, 16(1): 62-65.王子轩, 胡有谷, 陈祥民. 腰椎间盘局限性高信号区的发生与分布规律. 中国矫形外科杂志, 2008, 16(1): 62-65.
[12]Peng B, Hou S, Wu W, et al. The pathogenesis and clinical significance of a high -intensity zone (HIZ) of lumbar intervertebral disc on MR imaging in the patient with discogenic low back pain. Eur Spine J, 2006, 15(5): 583-587.
[13]Olmarker K. Puncture of a lumbar intervertebral disc induces changes in spontaneous pain behavior: an experimental study in rats. Spine (Phila Pa 1976), 2008, 33(8): 850-855.
[14]Videman T, Battie MC, Parent E, et al. Progression and determinants of quantitative magnetic resonance imaging measures of lumbar disc degeneration: a five-year follow-up of adult male monozygotic twins. Spine (Phila Pa 1976), 2008, 33(13): 1484-1490.
[15]Schmidt H, Kettler A, Rohlmann A, et al. The risk of disc prolapses with complex loading in different degrees of disc degeneration: a finite element analysis. Clin Biomech (Bristol, Avon), 2007, 22(9): 988-998.
[16]Carragee EJ, Don AS, Hurwitz EL, et al. 2009 ISSLS prize winner: does discography cause accelerated progression of degeneration changes in the lumbar disc: a ten-year matched cohort study. Spine (Phila Pa 1976), 2009, 34(21): 2338-2345.
[17]Zhang WY, Lian ZW, Liu J, et al. MRI findings and clinical significance of the lunmbar endplate osteochondritis.Chin J Magn Reson Imaging, 2010, 1(4): 286-290.张文煜, 廉宗澂, 刘筠, 等. 腰椎终板骨软骨炎的MRI表现与临床意义. 磁共振成像, 2010, 1(4): 286-290.
[18]Pan XM, Hu MY, Jiang B. UTE-T2mapping quantitative evaluation of lumbar cartilage endplate. Chin J Magn Reson Imaging, 2014, 5(2): 111-114.潘希敏, 胡美玉, 江波. 腰椎软骨终板的MR三维超短回波时间T2 mapping定量评价. 磁共振成像, 2014, 5(2): 111-114.
MR Imaging assessment of correlations between Pfirrmann’s grading system and lumbar disc bulge and lumbar disc protrution in young patients
ZHENG Zuo-feng, LI You-wei*, ZHANG Dong-po, MAO Lei
Department of Radiology, Beijing Chuiyangliu Hospital, Beijing 100022, China
*Correspondence to: Li YW, E-mail: lywhot@sohu.com
Received 3 Jan 2016, Accepted 15 Feb 2016
AbstractObjective: To find the MRI characteristics of the lumbar intervertebral disc degeneration in patients less than 30 years old with low back pain, and try to evaluate the correlations between Pfirrmann’s grading scale and intervertebral disc bugle and intervertebral disc protrution. Material and Methods: It is a cross-sectional and observational study. A total of 83 patients with low back pain performed lumbar MRI examination. All patients were less than 30 years old, of whom 50 were men and 33 were women, with mean age 25. All MR imaging were evaluated by two radiologists in the following aspects: signal intensity and morphology of the intervertebral discs, annular tear, intervertebral disc bulge, intervertebral disc protution, Modic changes and the Schmorl’s nodes. The intervertebral discs degeneration were evaluated through Pfirrmann’s classification system. The association between these different aspects were analyzed by Pearson multiple correlation. Results: A total of 415 intervertebral discs were examined, of which gradeⅠ—Ⅱ discs were 322 (77.6%), grade Ⅲ 56 (13.5%), grade Ⅳ 33 (7.9%) and grade Ⅴ 4 (1%). One hundred and three intervertebral discs were found with disc bulge and disc protrution, most of which were at disc L4—5 and L5—S1 level and werebook=204,ebook=51common in grade Ⅲ and grade Ⅳ degenerations. Seventeen patients were found with HIZ, and were all at disc L4—5 and L5—S1 level. Three patients were found with modic change. The statistic results show that grade Ⅲ degeneration were correlated well with disc bulge (r=0.972, P=0.006), but not with disc protrution (r=0.639, P=0.245) and the grade Ⅳ disc degeneration were correlated with disc protrution (r=0.999, P=0.000) and HIZ (r=0.919, P=0.028), but not with disc bulge (r=0.769, P=0.128). HIZ were correlated well with both disc bulge (r=0.919, P=0.027) and disc protrution (r=0.935, P=0.020). Conclusions: MRI is a good imaging modality for detecting the pathology character of disc degeneration in early stage. Grade and grade degenerations have close relationship with intervertebral disc bulge and protrution. It may have great clinical value to detect early changes of intervertebral disc degeneration in young patients.
Key wordsIntervertebral disk displacement; Magnetic resonance imaging; Young adult
DOI:10.12015/issn.1674-8034.2016.03.08
文献标识码:A
中图分类号:R445.2;R529.2
收稿日期:2016-01-03
通讯作者:
