Cancer of the Liver Italian Program score helps identify potential candidates for transarterial chemoembolization in patients with Barcelona Clinic Liver Cancer stage C
2016-04-28LiLiChunYanGouJingYingLiRehmatullahAchakzaiandXiuHuiLiBeijingChina
Li Li,Chun-Yan Gou,Jing-Ying Li,Rehmatullah Achakzai and Xiu-Hui LiBeijing,China
Cancer of the Liver Italian Program score helps identify potential candidates for transarterial chemoembolization in patients with Barcelona Clinic Liver Cancer stage C
Li Li,Chun-Yan Gou,Jing-Ying Li,Rehmatullah Achakzai and Xiu-Hui Li
Beijing,China
BACKGROUND:The Barcelona Clinic Liver Cancer(BCLC)staging system for hepatocellular carcinoma(HCC)recommends transarterial chemoembolization(TACE)as the first line therapy for stage B patients and sorafenib treatment for stage C patients.However,stage C patients exhibit variations in terms of tumor burden,liver function,and extrahepatic metastasis,which could potentially affect disease outcome.Here,we assessed whether the Cancer of the Liver Italian Program(CLIP)scores can help identify stage C patients likely to benefit from TACE.
METHODS:Out of 295 BCLC stage C HCC patients enrolled between January 2009 and December 2011,those with platelet counts >30×109cells/L,total bilirubin <51 µmoL/L,and an unobstructed main portal vein were scheduled for TACE(n=195).The remaining patients received best supportive care(BSC,n=100).All the patients were followed up for symptoms,performance status,and Child-Pugh classification scores every 4 weeks until death or December 2013.The prognosis of each group was evaluated by using the log-rank test and Cox-Mantel test.
RESULTS:The median overall survival(OS)was 6 months [95% confidence interval(CI):4.64-7.36].The OS was 9 months for the TACE group and 4 months for the BSC group.The TACE group had a longer OS than the BSC subgroup for CLIP scores 0-2 [13 months(95% CI:8.55-17.45)vs 4 months(95% CI:0.00-10.96),P=0.001].No significant differences were found between the TACE and BSC groups for CLIP scores 3-5.The CLIP score and treatment methods were found to be independent prognostic factors.
CONCLUSIONS:BCLC stage C HCC patients exhibit definite disease heterogeneity and can be reclassified by using the CLIP scoring system.Moreover,patients with CLIP scores 0-2 are likely to benefit from TACE.However,additional studies with long-term follow-up will be required to validate these findings.
(Hepatobiliary Pancreat Dis Int 2016;15:152-157)
KEY WORDS:hepatocellular carcinoma;
BCLC staging system;
CLIP scoring system;
transarterial chemoembolization
Author Affiliations:Department of Combined TCM and Western Medicine,Beijing You’an Hospital(Li L,Gou CY,Li JY and Li XH)and International School(Achakzai R),Capital Medical University,Beijing 100069,China Corresponding Author:Xiu-Hui Li,MD,Department of Combined TCM and Western Medicine,Beijing You’an Hospital,Capital Medical University,No.8,Xi Tou Tiao,You’anmen Wai,Fengtai District,Beijing 100069,China(Fax:+86-10-63296491;Email:lixiuhui@sohu.com)
© 2016,Hepatobiliary Pancreat Dis Int.All rights reserved.
Published online February 24,2016.
Introduction
H epatocellular carcinoma(HCC)is the fifth most common cancer and the third leading cause of cancer-related deaths worldwide.[1,2]According to the practice guidelines of the American Association for the Study of Liver Diseases(AASLD)for HCC,the Barcelona Clinic Liver Cancer(BCLC)system is the only staging system that can match patient groups to therapies across the continuum of disease heterogeneity seen with HCC.[3,4]Based on the BCLC staging system,transarterial chemoembolization(TACE)is recommended as the first line non-curative therapy for patients with large or multifocal HCC without vascular invasion or extrahepatic metastasis(BCLC stage B),whereas sorafenib is recommended as first line therapy for advanced(BCLC stage C)HCC patients requiring liver function protection who are less likely to benefit from curative therapy or TACE.[5-7]
However,sorafenib is not always available for some HCC patients due to financial limitations,especially in developing countries.In Asian countries,TACE has been widely used for patients with unresectable HCC,including those with portal vein thrombosis and extrahepatic metastasis,because of its good survival benefit and over-all safety for selected patients.[8-13]Tumor burden,liver function,portal vein invasion,and extrahepatic metastasis vary among BCLC stage C patients.This heterogeneity suggests different prognostic outcomes in these patients and the possibility that there are different strata of BCLC stage C patients with variable prognosis and requiring different optimal therapies.
In this study,we analyzed the overall survival(OS)and prognostic factors of BCLC stage C patients with HCC and found that the Cancer of the Liver Italian Program(CLIP)scoring system could more accurately stratify the patients with different outcomes.[15]
Methods
Patients
We enrolled 295 HCC patients who were initially classified into BCLC stage C between January 2009 and December 2011.The diagnosis of HCC was made according to the AASLD guidelines.[5]
The inclusion criteria were:(1)Eastern Cooperative Oncology Group(ECOG)performance status of 1-2;(2)liver function reserve of class A-B on Child-Pugh classification;(3)Okuda stage 1-2;(4)portal vein tumor thrombosis and/or extrahepatic metastasis;and(5)patients treated with TACE or supportive treatment.Patients with a secondary malignancy or with severe organ function failure were excluded.OS was calculated from the date of enrollment till the date of death or December 31,2013.Gender,age,etiology,Child-Pugh class,CLIP score,tumor size,type,and extent,portal vein tumor thrombosis,extrahepatic metastasis,platelet count,serum aspartate aminotransferase(AST),and serum alpha-fetoprotein(AFP)level were included as baseline variables.
The study protocol was approved by the Ethics Committee of Beijing You’an Hospital,Capital Medical University and adhered to the Declaration of Helsinki.Because of the retrospective nature of the study,written informed consent was waived off by the approval of the institutional review board.
Treatment
On the basis of our experience,patients with platelet count >30×109cells/L,total bilirubin <51 µmoL/L,and a main portal vein that was not completely obstructed by tumor thrombosis were scheduled for TACE.The patients were reevaluated after 3 to 4 weeks;in the interim,they were given symptomatic treatment as required.TACE would be repeated in the event of a residual tumor or if tumor recurrence was confirmed by computed tomography(CT)or magnetic resonance imaging(MRI)during follow-up.Patients who refused to undergo TACE or those who were not considered as suitable candidates for TACE were given symptomatic treatment or best supportive care(BSC).
TACE
Overall,195 patients underwent TACE.First,angiography was performed to identify the targeted feeding arteries of the tumor.The catheter was advanced to the hepatic artery and then to the lobar and segmental branches to facilitate maximum selectivity.A combination of chemotherapeutic agents and iodized oil was injected into the arteries,and a gelatin sponge was used to embolize the feeding artery.Doxorubicin(50 mg/m2)or 5-fluorouracil(500 mg/m2)was used as chemotherapeutic agent.The quantities of the iodized oil and sizes of the gelatin sponges used to embolize the tumors were decided by two senior interventional physicians at our center based on the tumor sizes.
Follow-up
The patients were followed up for symptoms,ECOG performance status,and Child-Pugh classification with a physical examination every 4 weeks.They underwent enhanced MRI and CT scanning every 4 to 8 weeks until death or the end point of follow-up,December 31,2013.
Statistical analysis
All data were analyzed with the SPSS statistical software(IBM SPSS Statistics 21).Disease-specific survival was analyzed using the Kaplan-Meier method.The logrank test was used to analyze differences in survival.Multivariate analysis was performed using the Cox proportional hazards model with forward stepwise selection.A P value of <0.05 was considered statistically significant.
Results
Baseline characteristics of TACE and no-TACE patient Of the 295 patients,195(66.1%)received TACE(TACE group)and 100(33.9%)received symptomatic treatment or BSC(BSC group).TACE was repeated in 91 of the 195 patients;the median session of TACE procedures per patient was 2(range 1-8).Baseline characteristics of the patients are shown in Table 1.Gender,age,etiology,tumor size,extent,metastasis,platelet count,and the levels of AST and AFP were not significantly different between the two groups(Table 1).The baseline Child-Pugh class,CLIP score,portosytemic shunt,and portal vein invasion status were significantly different between the two groups,with patients in the BSC group having a moreadvanced disease status compared with the TACE group.

Table 1.Baseline variables of the patients with BCLC stage C HCC(n,%)
Analysis of prognosis
The median OS was 6 months [95% confidence interval(CI):4.64-7.36] for all patients(Fig.1).The 1- and 2-year OS rates were 32.9% and 12.8%,respectively(P=0.001).
In the Cox regression test,univariate analysis showed that the median OS was significantly longer in the TACE group than in the BSC group(9 vs 4 months,respectively;P=0.001;Table 2,Fig.2).Additionally,OS was significantly correlated with CLIP score(OS,12 months and 5 months for score 0-2 and score 3-5,respectively,P=0.001;Table 2,Fig.3),extent of tumor(OS,8 months and 4 months for ≤50% and >50%,respectively,P=0.001),portal vein thrombosis(OS,4 months and 7 months for groups with and without portal vein thrombosis,respectively,P<0.001),Child-Pugh class(OS,9 months and 4 months for class A and B,respectively,P=0.001),and AFP level(OS,8 months and 5 months for <400 ng/mL and ≥400 ng/mL,respectively,P=0.035)(Table 2).

Fig.1.Kaplan-Meier curve of patients with BCLC stage C HCC.The median OS was 6 months(95% confidence interval:4.64-7.36,n=295).

Fig.2.Kaplan-Meier curves for different treatment subgroups.The overall survival in the TACE group(median OS:9 months,n=195)was significantly longer than in the BSC group(median OS:4 months,n=100).
Multivariate analysis,excluding the influence of con-founding factors,identified both the treatment method and CLIP score as independent prognostic factors for longer OS(P=0.001 in both cases;Table 3).
Of note,subgroup analyses showed that patients with CLIP scores of 0-2 obtained more benefit from TACE than from BSC(P=0.001);the median OS was 13 months(95% CI:8.55-17.45)and 4 months(95% CI:0.00-10.96)in the TACE and BSC groups,respectively(Table 4,Fig.4A).In patients with CLIP scores of 3-5,however,there was no significant difference between the TACE and BSC groups;the median OS was 5 months and 4 months respectively for the two groups(Table 4,Fig.4B).
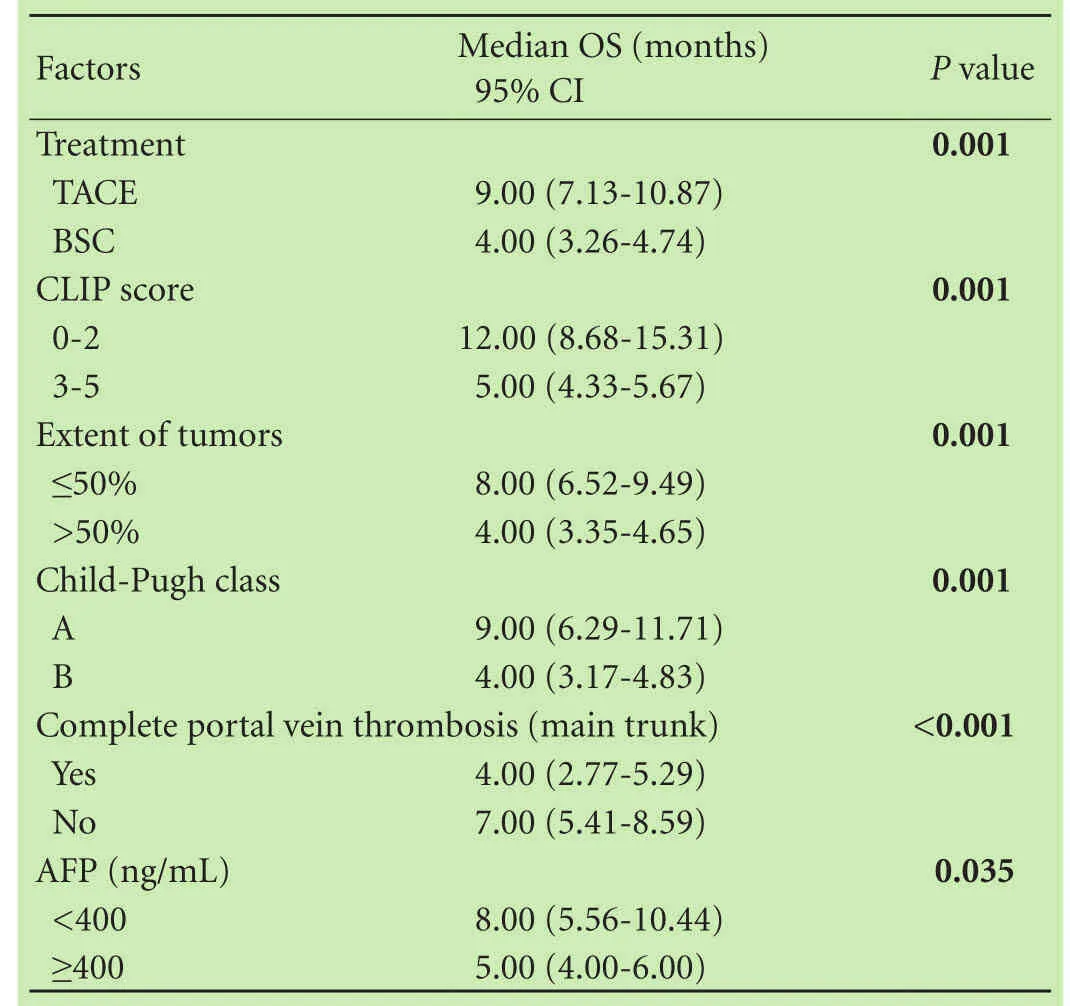
Table 2.Univariate analysis for patients survival with BCLC stage C HCC
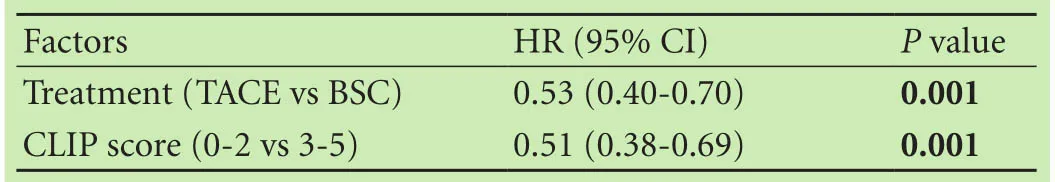
Table 3.Multivariate analysis for patients survival with BCLC stage C HCC
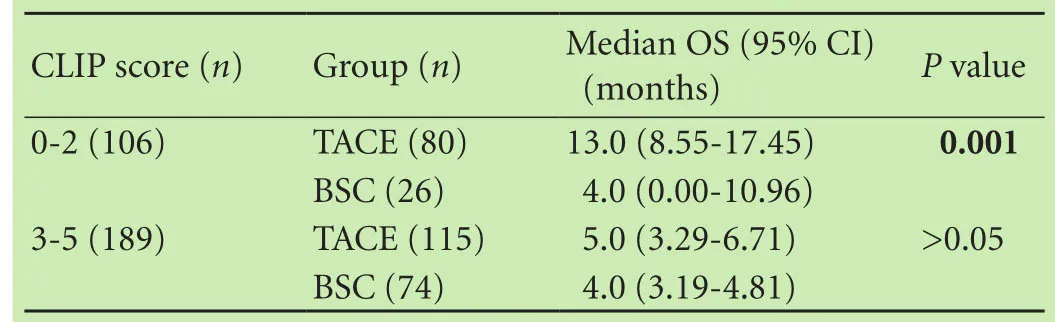
Table 4.Patients survival in the subgroups
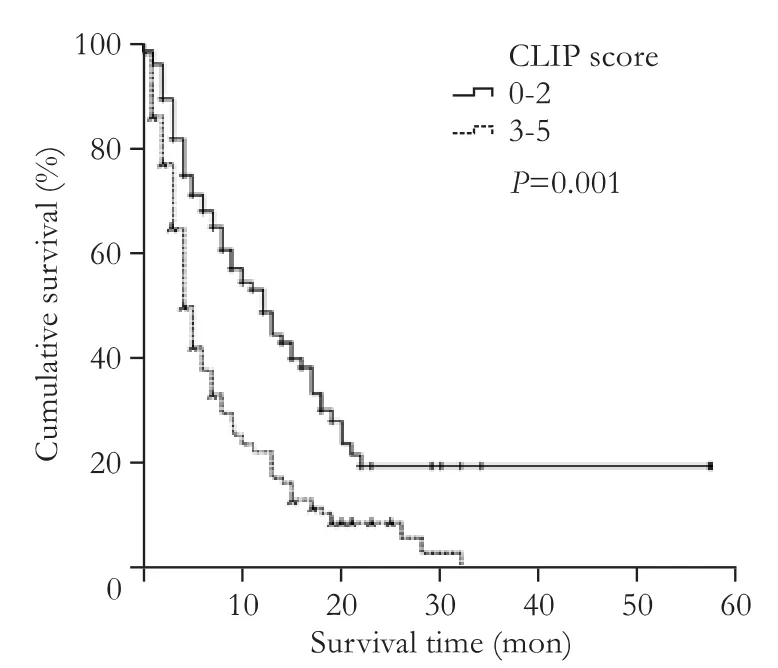
Fig.3.Kaplan-Meier curves for patients of different CLIP score subgroups.The overall survival in the CLIP 0-2 group(median OS:12 months,n=106)was significantly longer than that in the CLIP 3-5 group(median OS:5 months,n=189).
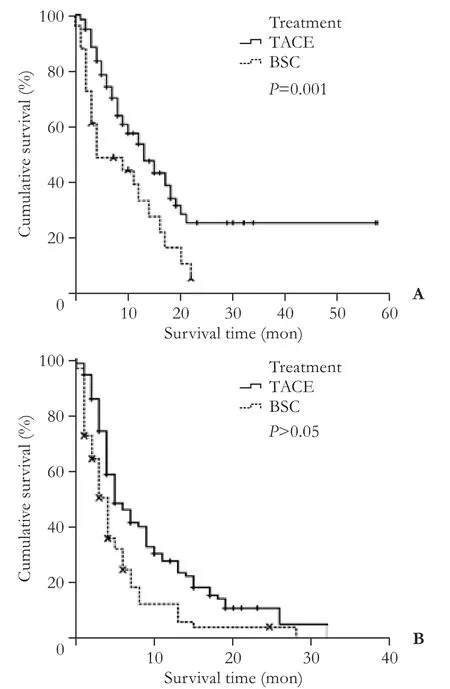
Fig.4.Kaplan-Meier curves for different treatment subgroups categorized on the basis of CLIP scores.A:Kaplan-Meier curves for different treatment subgroups in patients with CLIP scores 0-2.These patients derived more benefit from TACE(median OS:13 months,n=80)than from BSC case(median OS:4 months,n=26).B:Kaplan-Meier curves for different treatment subgroups in patients with CLIP scores of 3-5.In this patient population,there was no significant difference between TACE(median OS:5 months,n=115)and BSC subgroups(median OS:4 months,n=74).
Complications
The incidence of complications was 82.05%(n=160)in the TACE group.The most common treatment-related complications were fever,abdominal pain,or temporary liver function deterioration.Two(1.02%)patients with CLIP scores of 4 and 5 experienced an irreversible deterioration of liver function and died of liver failure approximately 1 and 2 months after TACE,respectively.
Discussion
While several staging systems have been developed for HCC,there is no consensus on a universal accepted and optimal staging system that best predicts prognosis in HCC patients.[15-17]The heterogeneity in prevalence and etiology of HCC in different populations results in the inaccuracy of one staging system used in a population different from where it was developed.[17]
The BCLC staging broadly classifies nonsurgical HCC as stage B(intermediate)or stage C(advanced);BCLC stage C patients have symptomatic tumors(ECOG performance status test,1-2),portal vein tumor invasion,or extrahepatic spread.[4]However,BCLC stage C HCC is known to include a heterogeneous group of patients with heterogeneous prognosis.[18]Patients in our study also showed heterogeneity in several baseline characteristics such as Child-Pugh class,CLIP score,portosystemic shunt,and portal vein invasion status,while other variables such as tumor size,extent,metastasis,and AFP levels were similar between the two study groups.
While the BCLC staging classification recommends sorafenib as the first line therapy for BCLC stage C patients,[5-7]access to sorafenib is often limited in developing countries and TACE has been recommended and widely used as palliative therapy in China[19]and other Asian countries.[8-13]Studies[11-13]have shown that TACE provides good survival benefit and overall safety for selected patients with advanced HCC.Our study also showed a significantly longer overall survival(median OS,13 months)in patients treated with TACE compared with those treated with BSC(median OS,4 months).These results support TACE as a treatment strategy in advanced-stage HCC.
Studies[20-23]have identified different prognostic factors for overall survival in BCLC stage C HCC patients.An Austrian study identified Child-Pugh class as the only independent prognostic factor in a group of advanced HCC patients treated by TACE or sorafenib.[20]A Japanese study[21]identified degree of liver damage,TNM stage,and AFP levels,and two Chinese studies[22,23]identified tumor lesion numbers,Child-Pugh class,metastasis,and portal vein invasion,as the independent prognostic factors in advanced HCC treated by TACE.In the present study,we identified that both the treatment method and CLIP score were independent prognostic factors for overall survival in the studied patients.Patients with CLIP 0-2 tumors had a longer OS than those with CLIP 3-5 tumors.Our results suggested that a CLIP score of 0-2 corresponds to better outcome than a higher score,and patients with a low CLIP score may still benefit from active therapy.
Careful patient selection is known to be crucial for the success of TACE.[20]We found that TACE treatment significantly improved the OS in CLIP 0-2 patients compared with those with higher CLIP scores.Our findings supported that BCLC stage C patients have disease heterogeneity and could be further classified into different strata according to outcomes.Thus,the CLIP scoring system can be used as a useful tool to stratify patients with BCLC stage C HCC.CLIP classification is easy to perform;it considers Child-Pugh class,tumor morphological type,tumor extent,portal vein invasion,and serum AFP levels.CLIP classification thus inherently includes several independent prognostic determinants of HCC and has been shown to possess a higher predictive power than the Okuda classification.[15,24]Our findings also confirm that TACE is an effective therapy for BCLC stage C patients with a CLIP score of 0-2.[16]In this study,we identified the subgroup that could get the maximum benefit from TACE among BCLC stage C HCC patients.Further,TACE related complications observed in this study were comparable to that observed in previous studies suggesting that TACE is generally safe for patients even with advanced HCC.[11,25]
The main limitations of our study are its retrospective nature and the fact that environmental factors,such as socioeconomic status and alcohol abuse,which affect the prognosis of HCC,were not taken into consideration.Moreover,the results of this study represent the outcomes of a single center in China and may not be universally applicable.
In conclusion,BCLC stage C patients have disease heterogeneity and can be reclassified using the CLIP scoring system.Patients with CLIP scores 0-2 tend to have better overall survival and are better candidates for TACE.Future studies involving a randomized prospective design and longer follow-up durations are needed to verify whether implementation of different treatment modalities on the basis of CLIP scores result in overall improvement.The CLIP score may also be explored as a tool to identify patients with advanced HCC in clinical trials.
Contributors:LXH proposed the study.LL and GCY performed the research and wrote the first draft.LJY and AR collected andanalyzed the data.All authors contributed to the design and interpretation of the study and to further drafts.LXH is the guarantor.Funding:This study was supported by grants from You’an Liver disease/AIDS funding(2011),and the National Science &Technology Pillar Program during the 12th Five-year Plan Period(2013BAI13B04).
Ethical approval:The study protocol was approved by the Ethics Committee of Beijing You’an Hospital,Capital Medical University and adhered to the Declaration of Helsinki.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
1 Parkin DM.Global cancer statistics in the year 2000.Lancet Oncol 2001;2:533-543.
2 El-Serag HB,Rudolph KL.Hepatocellular carcinoma:epidemiology and molecular carcinogenesis.Gastroenterology 2007;132:2557-2576.
3 Bruix J,Sherman M;Practice Guidelines Committee,American Association for the Study of Liver Diseases.Management of hepatocellular carcinoma.Hepatology 2005;42:1208-1236.
4 Llovet JM,Brú C,Bruix J.Prognosis of hepatocellular carcinoma:the BCLC staging classification.Semin Liver Dis 1999;19:329-338.
5 Bruix J,Sherman M;American Association for the Study of Liver Diseases.Management of hepatocellular carcinoma:an update.Hepatology 2011;53:1020-1022.
6 Bruix J,Llovet JM.Prognostic prediction and treatment strategy in hepatocellular carcinoma.Hepatology 2002;35:519-524.
7 Heng-jun G,Yao-jun Z,Min-shan C,Mei-xian C,Jun-ting H,Li X,et al.Rationality and effectiveness of transarterial chemoembolization as an initial treatment for BCLC B stage HBV-related hepatocellular carcinoma.Liver Int 2014;34:612-620.
8 Luo J,Guo RP,Lai EC,Zhang YJ,Lau WY,Chen MS,et al.Transarterial chemoembolization for unresectable hepatocellular carcinoma with portal vein tumor thrombosis:a prospective comparative study.Ann Surg Oncol 2011;18:413-420.
9 Xue TC,Xie XY,Zhang L,Yin X,Zhang BH,Ren ZG.Transarterial chemoembolization for hepatocellular carcinoma with portal vein tumor thrombus:a meta-analysis.BMC Gastroenterol 2013;13:60.
10 Niu ZJ,Ma YL,Kang P,Ou SQ,Meng ZB,Li ZK,et al.Transarterial chemoembolization compared with conservative treatment for advanced hepatocellular carcinoma with portal vein tumor thrombus:using a new classification.Med Oncol 2012;29:2992-2997.
11 Lee HS,Kim JS,Choi IJ,Chung JW,Park JH,Kim CY.The safety and efficacy of transcatheter arterial chemoembolization in the treatment of patients with hepatocellular carcinoma and main portal vein obstruction.A prospective controlled study.Cancer 1997;79:2087-2094.
12 Kim KM,Kim JH,Park IS,Ko GY,Yoon HK,Sung KB,et al.Reappraisal of repeated transarterial chemoembolization in the treatment of hepatocellular carcinoma with portal vein invasion.J Gastroenterol Hepatol 2009;24:806-814.
13 Yoo DJ,Kim KM,Jin YJ,Shim JH,Ko GY,Yoon HK,et al.Clinical outcome of 251 patients with extrahepatic metastasis at initial diagnosis of hepatocellular carcinoma:does transarterial chemoembolization improve survival in these patients? J Gastroenterol Hepatol 2011;26:145-154.
14 The Cancer of the Liver Italian Progran(CLIP)Investigators.A new prognostic system for hepatocellular carcinoma:a retrospective study of 435 patients:the Cancer of the Liver Italian Program(CLIP)investigators.Hepatology 1998;28:751-755.
15 Huitzil-Melendez FD,Capanu M,O’Reilly EM,Duffy A,Gansukh B,Saltz LL,et al.Advanced hepatocellular carcinoma:which staging systems best predict prognosis? J Clin Oncol 2010;28:2889-2895.
16 Farinati F,Rinaldi M,Gianni S,Naccarato R.How should patients with hepatocellular carcinoma be staged? Validation of a new prognostic system.Cancer 2000;89:2266-2273.
17 Italian Association for the Study of the Liver(AISF);AISF Expert Panel;AISF Coordinating Committee,Bolondi L,Cillo U,Colombo M,et al.Position paper of the Italian Association for the Study of the Liver(AISF):the multidisciplinary clinical approach to hepatocellular carcinoma.Dig Liver Dis 2013;45:712-723.
18 Llovet JM,Di Bisceglie AM,Bruix J,Kramer BS,Lencioni R,Zhu AX,et al.Design and endpoints of clinical trials in hepatocellular carcinoma.J Natl Cancer Inst 2008;100:698-711.
19 China MoHotPsRo.Diagnosis,management,and treatment of hepatocellular carcinoma(V2011).J Clinical Hepatol 2011;11:1141-1159.
20 Pinter M,Hucke F,Graziadei I,Vogel W,Maieron A,Königsberg R,et al.Advanced-stage hepatocellular carcinoma:transarterial chemoembolization versus sorafenib.Radiology 2012;263:590-599.
21 Takayasu K,Arii S,Ikai I,Omata M,Okita K,Ichida T,et al.Prospective cohort study of transarterial chemoembolization for unresectable hepatocellular carcinoma in 8510 patients.Gastroenterology 2006;131:461-469.
22 Liu L,Zhang C,Zhao Y,Qi X,Chen H,Bai W,et al.Transarterial chemoembolization for the treatment of advanced hepatocellular carcinoma with portal vein tumor thrombosis:prognostic factors in a single-center study of 188 patients.Biomed Res Int 2014;2014:194278.
23 Xiao J,Li G,Lin S,He K,Lai H,Mo X,et al.Prognostic factors of hepatocellular carcinoma patients treated by transarterial chemoembolization.Int J Clin Exp Pathol 2014;7:1114-1123.
24 Okuda K,Ohtsuki T,Obata H,Tomimatsu M,Okazaki N,Haregawwa H,et al.Natural history of hepatocellular carcinoma and prognosis in relation to treatment.Cancer 1985;56:918-928.
25 Kim JH,Yoon HK,Kim SY,Kim KM,Ko GY,Gwon DI,et al.Transcatheter arterial chemoembolization vs.chemoinfusion for unresectable hepatocellular carcinoma in patients with major portal vein thrombosis.Aliment Pharmacol Ther 2009;29:1291-1298.
Received April 29,2015
Accepted after revision December 8,2015
doi:10.1016/S1499-3872(16)60070-X
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- OIder age at first birth is a risk factor for pancreatic cancer:a meta-anaIysis
- Pathologic response to preoperative transarterial chemoembolization for resectable hepatocellular carcinoma may not predict recurrence after liver resection
- Role of microRNA in liver regeneration
- An unusual case of prolonged post-endoscopic retrograde cholangiopancreatography jaundice
- Surgical treatment of synchronous colorectal liver and lung metastases:the usefulness of thoracophrenolaparotomy for single stage resection
- Monocyte chemoattractant protein-1,transforming growth factor-β1,nerve growth factor,resistin and hyaluronic acid as serum markers:comparison between recurrent acute and chronic pancreatitis
