Successful liver allograft inflow reconstruction with the right gastroepiploic vein
2016-04-11RafaelPinheiroRuyCruzJrLucasNacifMatheusVaneandLuizACAlbuquerquePauloBrazil
Rafael S Pinheiro, Ruy J Cruz Jr, Lucas S Nacif, Matheus F Vane and Luiz AC D’Albuquerque São Paulo, Brazil
Author Affiliations: Liver Transplant Division, Department of Gastroenterology, University of São Paulo School of Medicine, São Paulo, SP, Brazil (Pinheiro RS, Cruz RJ Jr, Nacif LS and D’Albuquerque LAC), and Department of Anesthesiology, University of São Paulo School of Medicine, São Paulo, SP, Brazil (Vane MF)
Successful liver allograft inflow reconstruction with the right gastroepiploic vein
Rafael S Pinheiro, Ruy J Cruz Jr, Lucas S Nacif, Matheus F Vane and Luiz AC D’Albuquerque São Paulo, Brazil
Author Affiliations: Liver Transplant Division, Department of Gastroenterology, University of São Paulo School of Medicine, São Paulo, SP, Brazil (Pinheiro RS, Cruz RJ Jr, Nacif LS and D’Albuquerque LAC), and Department of Anesthesiology, University of São Paulo School of Medicine, São Paulo, SP, Brazil (Vane MF)
Published online May 15, 2015.
ABSTRACT:Portal vein thrombosis is a common complication in cirrhotic patients. When portal vein thrombectomy is not a suitable option, a large collateral vessel can be used for allograft venous inflow reconstruction. We describe an unusual case of successful portal revascularization using the right gastroepiploic vein. The patient underwent a cadaveric orthotopic liver transplantation with end-to-end anastomosis of the portal vein to the right gastroepiploic vein. Six months after liver transplantation the patient is well with good liver function. The use of the right gastroepiploic vein for allograft venous reconstruction is feasible and safe, with a great advantage of avoiding the need of venous jump graft.
(Hepatobiliary Pancreat Dis Int 2016;15:106-107)
KEY WORDS:liver transplantation; vascular grafting; portal vein, cavernous transformation of; varicose veins; hypertension, portal
Introduction
Portal vein thrombosis is a common complication of cirrhosis, with a prevalence ranging from 10% to 25%.[1]Moreover, it is an independent risk factor for higher mortality after liver transplantation (LT).[2]Several surgical options are available to overcome this issue including thrombectomy, cavoportal hemitransposition, and multivisceral transplantation. The choice of the procedure depends on the extension of portomesenteric thrombosis. Usually, when thrombectomy is not suitable, a large collateral vessel can be used for allograft venous inflow reconstruction. We describe an unusual case of successful portal revascularization using the right gastroepiploic vein (RGEV) of recipients.
Clinical image
The recipient was a 54-year-old woman with end-stage liver disease secondary to non-alcoholic steatohepatitis. Pretransplant evaluation demonstrated a grade II chronic portal vein thrombosis.[3]A patent superior mesenteric vein (SMV) and a splenic vein with a large RGEV were also observed on the pre-operatory CT scan (Fig. 1). The patient underwent a cadaveric orthotopic liver transplantation with a model for end-stage liver disease score of 33. During the procurement, a long segment of SMV was procured in continuity with the portal vein. Additional venous grafts including iliac and jugular veins were also procured. During the dissection of the portal triad, the cavernomatous transformation of the portal vein was confirmed, and several small caliber venous collaterals were identified. The hepatic artery and bile duct were identified and deemed optimal for anastomosis. After a piggyback hepatectomy, the outflow allograft reconstruction was completed by an end-to-side cavo-cavostomy. The allograft SMV was brought anteriorly to the pancreas and behindthe distal antrum and pylorus. The RGEV was identified and clamped close to the take-off from infrapancreatic SMV. The RGEV was then transected and brought through a tunnel into the transverse colon. An end-to-end portal vein to RGEV anastomoses was performed (Fig. 2). Arterial and biliary reconstruction was completed. Before abdominal closure, a direct portal vein blood flow measurement (using VeriQ device; Medistim; Oslo, Norway) showed a flow of 1.07 L/min with a pulsatile index of 0.2.
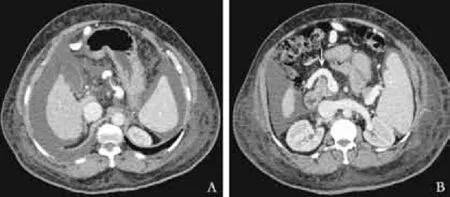
Fig. 1. Pre-operatory CT scan showing (A) a complete portal vein thrombosis and (B) the right gastroepiploic vein taking off from the superior mesenteric vein (arrow).

Fig. 2. A: Intra-operatory picture showing an end-to-end anastomosis of the allograft portal vein (red arrow) to the right gastroepiploic vein (green arrow). Large green arrow shows the distal part of the gastroepiploic vein. B: Posttransplant CT scan showing the right gastroepiploic vein (red arrow) anteriorly to the pancreas and behind the pylorus (green arrow).
Laboratory evaluation demonstrated that lactate and aminotransferases progressively drop to regular levels. Immediately after surgery, INR was 2.2, and at the first postoperative day it was 1.56. Follow-up Doppler showed a patent portal vein with a good flow. The patient later presented with a complicated cytomegalovirus infection infection with good response to antiviral treatment, and was discharged from the hospital on day 20. Now, 6 months after LT, the patient is well with good liver function.
Discussion
Portal vein thrombosis poses a technical challenge to liver transplantation surgeons. Preoperative multiphasic contrast enhanced CT or magnetic resonance imaging are the preferred method to guide operative strategy in patients with portal vein thrombosis. Their sensitivity for complete portal vein thrombosis ranges from 92% to 100%.[4]The main treatment of complex portal vein thrombosis during cadaveric liver transplantation is an anastomosis to a large collateral vein.
Other authors have also used collaterals for portal vein reconstruction including the coronary vein, pericholedochal, peripancreatic or perigastroesophageal varices.[5]Indeed, any sizable patent splanchnic tributary is a potential option. Usually, collaterals measuring at least 2 cm provide enough venous blood flow, although it must be tested before implanting the graft. Great caution should be taken when controlling and suturing these alternative vessels because they are thin-walled and can tear easily. Sometimes, an interposition graft is necessary to avoid traction, the iliac vein conduit is the preferred choice and its placement should be prior to hepatectomy to avoid longer warm ischemia time.[6]
Another advantage of using collaterals to portal reconstruction is the low rate of postoperative complications. The use of anticoagulants such as heparin in the early posttransplant course should be recommended, especially in cases employing interposition graft. Longterm postoperative anticoagulation is limited to patients with documented hypercoagulable states.[7]
In conclusion, we believe that the use of RGEV for allograft venous reconstruction is feasible and safe, with a great advantage of avoiding the need of venous jump graft.
Contributors: CRJ proposed the study. PRS, NLS and VMF collected the data, performed research and wrote the draft. CRJ and ALAC have been involved in revising the manuscript critically for important intellectual content, and have given final approval of the version to be published. PRS is the guarantor.
Funding: None.
Ethical approval: This paper was approved by the Institutional Review Board of FMUSP and the patient.
Competing interest: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
1 Nonami T, Yokoyama I, Iwatsuki S, Starzl TE. The incidence of portal vein thrombosis at liver transplantation. Hepatology 1992;16:1195-1198.
2 Rana A, Hardy MA, Halazun KJ, Woodland DC, Ratner LE, Samstein B, et al. Survival outcomes following liver transplantation (SOFT) score: a novel method to predict patient survival following liver transplantation. Am J Transplant 2008;8:2537-2546.
3 Yerdel MA, Gunson B, Mirza D, Karayalçin K, Olliff S, Buckels J, et al. Portal vein thrombosis in adults undergoing liver transplantation: risk factors, screening, management, and outcome. Transplantation 2000;69:1873-1881.
4 Rodríguez-Castro KI, Porte RJ, Nadal E, Germani G, Burra P, Senzolo M. Management of nonneoplastic portal vein thrombosis in the setting of liver transplantation: a systematic review. Transplantation 2012;94:1145-1153.
5 Alexopoulos SP, Thomas E, Berry E, Whang G, Matsuoka L. The portal vein-variceal anastomosis: an important technique for establishing portal vein inflow. Clin Transplant 2014;28:52-57.
6 Lai Q, Spoletini G, Pinheiro RS, Melandro F, Guglielmo N, Lerut J. From portal to splanchnic venous thrombosis: What surgeons should bear in mind. World J Hepatol 2014;6:549-558.
7 Francoz C, Valla D, Durand F. Portal vein thrombosis, cirrhosis, and liver transplantation. J Hepatol 2012;57:203-212.
Received August 20, 2014
Accepted after revision November 20, 2014
Letters to the Editor
The Editor welcomes submissions for possible publication in the Letters to the Editor section.
Letters commenting on an article published in the Journal or other interesting pieces will be considered if they are received within 6 weeks of the time the article was published. Authors of the article being commented on will be given an opportunity to offer a timely response to the letter. Authors of letters will be notified that the letter has been received. Unpublished letters cannot be returned.
doi:10.1016/S1499-3872(15)60369-1
Corresponding Author:Rafael S Pinheiro, MD, Liver Transplant Division, Department of Gastroenterology, University of São Paulo School of Medicine, Rua Dr. Enéas de Carvalho Aguiar, 255-suite 9113/9114, São Paulo, SP 05403-900, Brazil (Tel: +55-11-2661-3323; Fax: +55-11-2661-6250; Email: rsnpinheiro@gmail.com)
© 2016, Hepatobiliary Pancreat Dis Int. All rights reserved.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Ultrasound features of hepatocellular adenoma and the additional value of contrast-enhanced ultrasound
- External validation of PREPARE score in Turkish patients who underwent pancreatic surgery
- Circulating myeloid-derived suppressor cells in patients with pancreatic cancer
- Acute pancreatitis induced by transarterial chemoembolization: a single-center experience of over 1500 cases
- Silver-nanoparticle-coated biliary stent inhibits bacterial adhesion in bacterial cholangitis in swine
- Risk factors for postoperative bile leakage: a retrospective single-center analysis of 411 hepatectomies