Meta-analysis about Western Medicine combined with activating blood drugs on modulating blood glucose and lipids in diabetic patients
2016-03-27HungSuping黄苏萍QiuCixi邱彩霞LinMioxin林妙娴ChenLonghui陈龙辉YnQunfng颜群芳ChenChoyun陈超云WngSimei王思梅YeMengjie叶梦捷ZhengHulin郑沪琳KngWenqin康文倩HungBowei黄博威HengXinpei衡先培
Hung Suping(黄苏萍), Qiu Cixi(邱彩霞),b, Lin Mioxin(林妙娴), Chen Longhui(陈龙辉), Yn Qunfng(颜群芳), Chen Choyun(陈超云), Wng Simei(王思梅), Ye Mengjie(叶梦捷), Zheng Hulin(郑沪琳), Kng Wenqin(康文倩), Hung Bowei(黄博威), n Heng Xinpei(衡先培)
a:Fujian University of Traditional Chinese Medicine, Fuzhou 350122, China
b:The People’s Hospital Affiliated to Fujian University of Traditional Chinese Medicine, Fuzhou 350004, China
c:Xiamen Heshan Street Community Health Service Center, Xiamen 361015, China
d:Pi-Wei Institute, Guangzhou University of Chinese Medicine, Guangzhou 510405, China
Meta-analysis about Western Medicine combined with activating blood drugs on modulating blood glucose and lipids in diabetic patients
Huang Suping(黄苏萍)a, Qiu Caixia(邱彩霞)a,b, Lin Miaoxian(林妙娴)c, Chen Longhui(陈龙辉)d, Yan Qunfang(颜群芳)a, Chen Chaoyun(陈超云)a, Wang Simei(王思梅)a, Ye Mengjie(叶梦捷)a, Zheng Hulin(郑沪琳)a, Kang Wenqian(康文倩)a, Huang Bowei(黄博威)a, and Heng Xianpei(衡先培)b*
a:Fujian University of Traditional Chinese Medicine, Fuzhou 350122, China
b:The People’s Hospital Affiliated to Fujian University of Traditional Chinese Medicine, Fuzhou 350004, China
c:Xiamen Heshan Street Community Health Service Center, Xiamen 361015, China
d:Pi-Wei Institute, Guangzhou University of Chinese Medicine, Guangzhou 510405, China
OBJECTIVE:To assess the ef f ect of activating blood drugs (AB drugs) on blood glucose and lipid levels of diabetic patients.
Diabetes mellitus; Activating blood drugs; Chinese herbal medicine; Blood glucose; Blood lipid; System evaluation
INTRODUCTION
The prevalence of diabetes mellitus (DM) is increasing rapidly across the world. The latest data from the international diabetes federation (IDF) showed the number of diabetic patients has reached 371 million, accounting for about 8.3% of the global population. IDF then predicted that there would be at least 552 million diabetic patients by 2030. In other words, one out of ten people would suf f er from DM then1.
The main hazard of DM is vasculopathy. Atherosis, which is induced by metabolic disorder of carbohydrates and lipids, has been proved to be the primary vasculopathy and the leading cause of disability and even death among diabetic patients2. Accumulating evidence suggests that AB drugs have curative effect on vasculopathy in DM3-5which seems to benefit from their modulating ef f ects on blood glucose and lipid.
The mechanism of DM was closely related with thrombogenesis in Traditional Chinese Medicine theory, AB drugs have effect on melting thrombus and rebuilding normalcycle of blood. The traditional theory happened to have the same view with the modern ones. DM led to unbalance of lipid metabolism and stimulated blood vessels release various inflammatory factors and high viscosity led to embolism in Modern medicine theory. So scholars used improving blood cycle and protecting vessels drugs in clinical treatment.
The objective of this systematic review is to assess the evidence from RCTs of AB drugs for modulating blood glucose and lipid in DM.
METHODS
Data sources
Databases searched from their respective inceptions through May 2016 included MEDLINE, Cochrane library and Embase and 3 Chinese databases (Chinese Biomedical Literature Database, China National Knowledge Infrastructure and Database for Chinese Technical Periodicals). Two authors (QIU Cai-xia and LIN Miao-xian) independently searched the literature. The Medline search terms were (diabetes mellitus[MeSH Terms]) AND (herb* OR plant* OR TCM OR traditional Chinese medicine OR Complementary or Alternative OR supplementary OR extract*[Title/Abstract]) AND (Randomized Controlled Trial or RCT OR Clinical Trial). We adapted this search strategy for searches of Embase (using Emtree terms), CBM, CNKI, and VIP. We also searched the references of relevant studies.
Study selection
All RCTs comparing AB drugs alone/plus conventional western medicine with the same conventional western medicine alone/plus placebo in participants with diabetic patients who met the recognised diagnostic criteria.Six outcome measures considered for inclusion were changes in FBG, HbA1c, TG, TC, LDL-c and HDL-c. RCTs were excluded if they failed to of f er outcome measures which could ref l ect changes in blood glucose or lipids.
Quality evaluation
Use Review System risk bias assessment which contains 7 aspects: (a) Random sequence generation(selection bias); (b) Allocation concealment (selection bias); (c) Blinding of participants and personnel (performance bias); (d) Blinding of outcome assessment (detection bias); (e) Incomplete outcome data (attrition bias); (f) Selective reporting(reporting bias); (g) Other bias. All the bias assessment were completed independently by dif f erent researchers and decided by an expert of EBM.
Data extraction
All articles were read by two independent authors (QIU Cai-xia and LIN Miao-xian), and data from the articles were validated and extracted. The extracted data included: (a) the baseline between experimental group and control group, (b) study design, inclusion and exclusion criteria, duration of study and follow-up visit, interventions, and outcome measurements, and (c) indicators of the methodological quality of included trials (eg, randomization).
Statistical analysis
The Cochrane Collaboration’s software [Review Manager (RevMan) Version 5.2 for windows] was introduced to perform meta-analysis. Odds ratio (OR) or relative risk (RR) was applied as statistic for count data, and weighted mean dif f erence (WMD) or standardized mean dif f erence (SMD) for measurement data. 95% confidence interval (CI) was for interval estimation. The heterogeneity among included trials was analyzed byChi-square. The fi xed ef f ect model was applied when statistical homogeneity (P>0.1,I2<50%) was detected, however, the random effect model was applied instead when statistical heterogeneity (P<0.1,I2>50%) existed. Moreover, the heterogeneous sources would be traced and subset analysis would be done. When the heterogeneity was too large, however, the descriptive analysis would be introduced. The sensitivity analysis was conducted when heterogeneity came from low quality trials. Publication bias was analyzed by funnel plot.
RESULTS
Study identif i cation
A total of 58,669 published articles were initially identified (46,652 Chinese publications and 12,017 English publications). Most of the identif i ed publications were excluded and eventually 7 publications met the inclusion criteria (Flowchart of publication selection is shown in Figure 1).

Figure 1. Flowchart of publication selection process
Methodological quality of included studies
The present study included 7 RCTs, which were considered of high quality (Figure 2 and 3).

Figure 2. Risk of bias graph
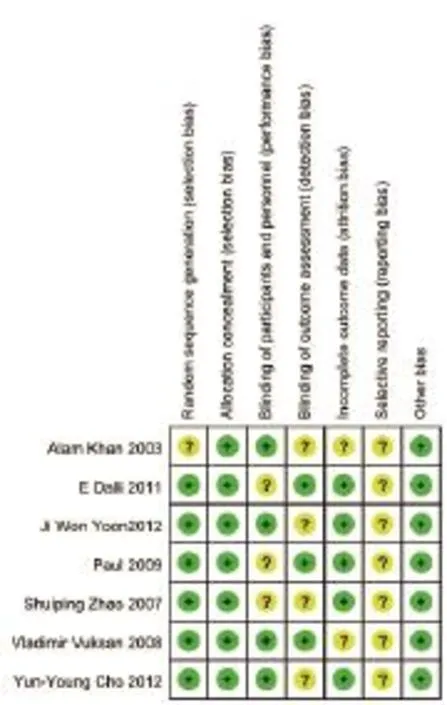
Figure 3. Risk of bias summary
Baseline of included studies
7 included RCTs showed no signif i cant dif f erence (P>0.05) in sex, age, blood pressure, body mass index (BMI), and diabetes duration. Table 1 lists the baseline of included studies (Table 1, Baseline of the including references6-12.

Table 1. Baseline of the including references
Outcomes
Changes in blood glucose
4RCTs tested Western medicine combined with AB drugs on FBG compared with Western medicine or placebo. The metaanalysis showed favorable effect (n=167, -0.79mmol/L FBG, 95% CI:-0.89 to -0.70,P<0.00001; heterogeneity:Chi2=2.89,P=0.41,I2=0%, Figure 4).
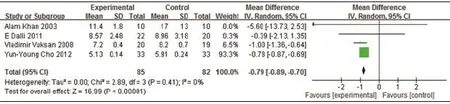
Figure 4. Meta-Analysis of Western Medicine combined with AB drugs for lowering FBG
3RCTs tested Western medicine combined with AB drugs on HbA1c compared with Western medicine or placebo. The metaanalysis failed to report favorable ef f ect (n=196, -0.4% HbA1c, 95% CI: -1.09 to 0.29, P<0.26; heterogeneity: Chi2=43.77, P=P<0.00001, I2=95%, Figure 5).
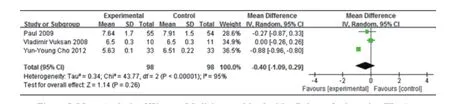
Figure 5. Meta-Analysis of Western Medicine combined with AB drugs for lowering HbA1c
Changes in blood lipids
4 RCTs tested Western medicine combined with AB drugs on TG compared with Western medicine or placebo. The metaanalysis failed to report favorable effect (n=193, -0.18mmol/L TG, 95% CI: -0.68 to 0.32, P=0.48; heterogeneity: Chi2=24.10, P<0.0001, I2=88%, Figure 6).

Figure 6. Meta-Analysis of Western Medicine combined with AB drugs for lowering TG
4 RCTs tested Western medicine combined with AB drugs on TC compared with Western medicine or placebo. The metaanalysis showed favorable effect (n=193, -0.45mmol/L TC, 95% CI: -0.71 to -0.19, P=0.0008; heterogeneity: Chi2=40.65, P<0.00001, I2=93%, Figure 7).

Figure 7. Meta-Analysis of Western Medicine combined with AB drugs for lowering TC
3RCTs tested Western medicine combined with AB drugs on LDL-c compared with Western medicine or placebo. The metaanalysis showed a favorable effect (n=653,-0.63mmol/L LDL-c, 95% CI: -0.92 to -0.34, P<0.0001; heterogeneity: Chi2=5.77, P=0.06, I2=65%, Figure 8).
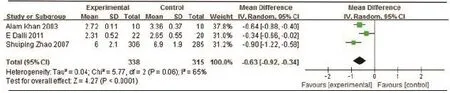
Figure 8. Meta-Analysis of Western Medicine combined with AB drugs for lowering LDL-c
3RCTs tested Western medicine combined with AB drugs on HDL-c compared with Western medicine or placebo. The metaanalysis showed favorable effect (n=173, 0.10mmol/L HDL-c, 95% CI: 0.08 to 0.12, P<0.00001; heterogeneity: Chi2=0.86, P=0.65, I2=0%, Figure 9).
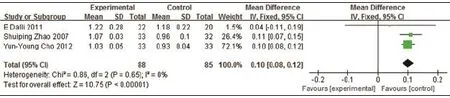
Figure 9. Meta-Analysis of Western Medicine combined with AB drugs for rising HDL-c
Safety
In the included RCTs, little toxic and side-ef f ect were observed during trial period. Abnormity was also not seen in blood routine examination, urine routine examination, liver function test, or kidney function test before and after drug treatment.
Publication bias evaluation
RevMan 5.2software was applied to draw funnel plot. We drew 6 funnel plots for evaluating publication bias for FBG, HbA1c, TG, TC, LDL-c and HDL-c, respectively. All the scatters displayed symmetrical distribution, which indicated low publication bias.
Sensitive analysis
We performed meta-analysis after excluding low quality studies. No obvious fl uctuation was observed, which indicated low sensitivity and reliable outcomes.
DISCUSSION
In the present study, we included 7 high quality RCTs. These RCTs investigated Cinnamon, Cholestin, Korean red ginseng, Crataegus laevigata, and Sajabalssuk, which are categorized as AB drugs according to TCM theory. Meta-analysis showed beneficial effects of Western medicine combined with the AB drugs in modulating blood glucose and lipids of diabetic patients compared with Western medicine or placebo.
Among the 7 RCTs, the study of Zhao demonstrated the largest project in which the diabetic patients were recruited from 65 research centers in 19 provinces across China7. In the study, blood TC, TG and LDL-C were signif i cantly reduced after Xuezhikang therapy. Xuezhikang, an extract of cholestin, has been approved for marketing by Food and Drug Administration of USA. It was recorded in Compendium of Materia Medica that cholestin could activate blood and remove stasis. In 1979, a Japanese researcher, Akira Endo, for the fi rst time isolated an active ingredient, named monacolin-K, from cholestin which could act as an inhibitor of cholesterol synthesis14. Interestingly, chemical analysis then showed that monacolin-K and lovastatin were identical. In the biosynthesis of cholesterol, HMG-CoA reductase enzyme was the key to the speed of cholesterol synthesis. Monacolins were competitive inhibitors of HMG-CoA reductase enzyme so that they were effective in reducing or blocking the endogenous synthesis of cholesterol.
Cinnamon was mostly investigated in the present meta-analysis. Alam Khan and colleagues demonstrated that the daily intake of 1, 3 or 6 g of cinnamon capsules for 40 days signif i cantly reduced FBG, TG, LDL-c, and TC in patients with type 2 diabetes6. The long-term effect of cinnamon on blood glucose and lipids, however, was not evidenced from this study. Interestingly, Paul Crawford investigated daily intake of 1 g cinnamon capsule for 90 days and found that cinnamon lowered HbA1c 0.83% compared with usual care alone lowering 0.37%9. This indicated longterm intake of cinnamon might be useful for lowering HbA1c in diabetic patients. Studies showed that cinnamon could improve insulin sensitivity and secretion13. The antioxidant ingredients, polyphenols of flavanol, contained in cinnamon could improve glycemic stability and reduce insulin resistance. Some other active ingredients could also improve insulin sensitivity and thus benef i t glucose metabolism13.
Panax ginseng, which was widely used in TCM hospitals, was considered as an AB drug. Twelve weeks of supplementation with Korean red ginseng (Panax ginseng) improved glucose and insulin regulation safely in a RCT with 19 diabetic participants8. Another research group demonstrated that 8-week treatment with ginsam, a vinegar extract from Panax ginseng, signif i cantly reduced HbA1c level in a RCT with 72 diabetic patient11. Together, the 2 RCTs indicated that Panax ginseng (and/or its extract) was effective in modulating glycemic levels even examined on a relatively long period of time. Another 2 AB drugs, Crataegus laevigata and Sajabalssuk, were also investigated. A research group showed that treatment for 6 months with a micronized flower and leaf preparation of Crataegus laevigata (400mg three times a day) signif i cantly decreased LDL-c in a RCT with 49 diabetic patients10. Nine-week treatment with Sajabalssuk extract (3g/day) signif i cantly lowered FBG, HbA1c and TC, and improved HDL-c compared to placebo and positive control12.
We failed to report signif i cant dif f erence between treatment and control groups in the effects of lowering blood HbA1c. HbA1c is a form of hemoglobin that is widely measured in clinics to monitor the average plasma glucose levels over prolonged periods of time. It serves as a marker for average blood glucose levels over the previous 3 months prior to the measurement. Out of the 7 included RCTS, 4 studies investigated changes of HbA1c towards treatment. However, most of the intervention duration seemed no more than 3 months, which might explain the reason why we failed to observe benef i cial ef f ects of Western medicine combined with AB drugs in lowering HbA1c. Thus we argued that the upcoming RCTs should prolong intervention duration for more than 3 months if they measure changes of HbA1c.
In conclusion, the present study indicated that AB drugs might probably show beneficial effects in modulating blood glucose and lipids of diabetic patients. Compared with control group, difference of FBG, TC, LDH-c and HDL-c, except HbA1c and TG, reached significant levels in treatment group. Notably, the benef i cial ef f ects of AB drugs were evidenced from RCTs which didn’t examine the drugs’ long-term ef f ects. Thus we expect future research would investigate the long-term ef f ects of AB drugs in modulating blood glucose and lipids of diabetic patients.
REFERENCES
1 International Diabetes Federation. Number of people with diabetes (20-79 years), 2013. Available at: http://www. idf.org/diabetesatlas/data-visualisations. Accessed at 14 November, 2013.
2 Gorokhova SG, Atamanova MA. Characteristics of erythrocytes and hemoglobin in patients with ischemic heart disease and type 2 diabetes mellitus. Terapevticheskii arkhiv, 2008,80(10):16-21.
3 YJ. X. Supplement qi, activating blood and eliminating phlegm in the application of the diabetes vascular lesions. Liaoning Journal of Traditional Chinese Medicine (Chin),2009(36):2089-2090.
4 Guo JR LH, Liang CY, et al. Effect of Three Bloodactivating and Stasis-resolving Medicines on Type 2 Diabetic Rats. Chinese Journal of Experimental Traditional Medical Formulas (Chin),2012(18):220-223.
5 Wang L GX. Treatment experience from the blood stasis of Liu Tonghua in diabetes. Journal of Traditional Chinese Medicine (Chin), 2011(52):35-36.
6 Khan A, Safdar M, Ali Khan MM, Khattak KN, Anderson RA. Cinnamon improves glucose and lipids of people with type 2 diabetes. Diabetes care,2003(26):3215-3218.
7 Zhao SP, Lu ZL, Du BM, et al. Xuezhikang, an extract of cholestin, reduces cardiovascular events in type 2 diabetes patients with coronary heart disease: subgroup analysis of patients with type 2 diabetes from China coronary secondary prevention study (CCSPS). Journal of cardiovascular pharmacology,2007(49):81-84.
8 Vladimir Vuksan, Mi-Kyung Sung John L, Sievenpiper, et al. Korean red ginseng (Panax ginseng) improves glucose and insulin regulation in well-controlled, type 2 diabetes: Results of a randomized, double-blind, placebo-controlled study of efficacy and safety Nutrition. Metabolism & Cardiovascular Diseases,2008 (18): 46-56.
9 Paul Crawford. Effectiveness of Cinnamon for Lowering Hemoglobin A1C in Patients with Type 2 Diabetes: A Randomized, Controlled Trial. JABFM,2009,22(5):507-512.
10 Dalli E, Colomer E, Tormos MC, et al. Crataegus laevigata decreases neutrophil elastase and has hypolipidemic ef f ect: a randomized, double-blind, placebo-controlled trial. Phytomedicine: international journal of phytotherapy and phytopharmacology,2011(18):769-775.
11 Ji Won Yoon, Seon Mee Kang, Jason L Vassy, et al. Efficacy and safety of ginsam, a vinegar extract from Panax ginseng, in type 2 diabetic patients: Results of a double-blind, placebo-controlled study. Journal of Diabetes Investigation, 2012,6(2):309-317.
12 Yun-Young Cho, Nam-In Baek c, Hae-Gon Chung,et al. Randomized controlled trial of Sajabalssuk (Artemisia princeps Pampanini)to treat pre-diabetes.European Journal of Integrative Medicine,2012(4):e299-e308.
13 Anderson, Richard A. Chromium and polyphenols from cinnamon inprove insulin sensitivity. Proceedings of the Nutrition Society,2008,67(1):48-53.
14 Endo A, Monacolin K. A new hypocholesterolemic agent produced by a Monascus species. The Journal of Antibiotics,1979,32(8):852-854.
(Accepted: June 7, 2016)
Funding: Natural Science Foundation of China (81173179); Major project of Fujian Science and technology (2014Y0063); Natural Science Foundation of Fujian Province (2012J01392)
*Correspondence author: E-mail:hengxianpei@hotmail. com; Mobile phone:+86-13067366157
METHODS:Systematic searches were conducted on 6 electronic databases and the search time was cut off in May 2016. Randomized controlled trials (RCTs) were included if they investigated diabetic patients who received Western medicine combined with AB drugs in the experimental groups and solitary usage of corresponding Western medicine or placebo in the control groups. 6 outcome measures, which were considered as inclusion, were changes in fasting blood glucose (FBG), glycosylated haemoglobin A1c (HbA1c), total triglyceride (TG), total cholesterol (TC), low density lipoprotein cholesterol (LDL-c) and high density lipoprotein cholesterol (HDL-c). The literature quality was assessed by Cochrane score for risk of bias in Review Manager 5.2, as well as meta-analysis was performed.RESULTS:7 RCTs comprising 999 patients met all inclusion criteria. Meta-analysis showed beneficial effects of Western medicine combined with AB drugs on modulating FBG, TC, LDL-c and HDL-c compared with Western medicine or placebo (P<0.05), while no dif f erence was observed in HbA1c, and TG (P>0.05). To some extent, the therapeutic effects of Western medicine combined with AB drugs were better than that of solitary usage of Western medicine or placebo. Besides, AB drugs were safe and reliable with little toxic and side-ef f ects.
CONCLUSIONS:The meta-analysis suggests benef i cial ef f ects of Western medicine combined with AB drugs on modulating blood glucose and lipids in diabetic patients.
杂志排行
World Journal of Integrated Traditional and Western Medicine的其它文章
- A randomized, controlled trial of Shutangluo fang in treating painful diabetic peripheral neuropathy
- Clinical ef f ects of acupoints moxibustion therapy on postsurgical gastroparesis syndrome after resection of esophageal cardia cancer
- A medical understanding on the wuxing theory in cell
- Analysis of the features of TCM and western medicine in the diagnosis and treatment of subclinical hypothyroidism characteristics
- INSTRUCTION FOR AUTHORS
