A serum metabolomic analysis for diagnosis and biomarker discovery of primary biliary cirrhosis and autoimmune hepatitis
2015-02-08
Hangzhou, China
A serum metabolomic analysis for diagnosis and biomarker discovery of primary biliary cirrhosis and autoimmune hepatitis
Jiang-Shan Lian, Wei Liu, Shao-Rui Hao, De-Ying Chen, Yin-Yin Wang, Jian-Le Yang, Hong-Yu Jia and Jian-Rong Huang
Hangzhou, China
BACKGROUND: Because of the diversity of the clinical and laboratory manifestations, the diagnosis of autoimmune liver disease (AILD) remains a challenge in clinical practice. The value of metabolomics has been studied in the diagnosis of many diseases. The present study aimed to determine whether the metabolic profles, based on ultraperformance liquid chromatography-mass spectrometry (UPLC-MS), differed between autoimmune hepatitis (AIH) and primary biliary cirrhosis (PBC), to identify specifc metabolomic markers, and to establish a model for the diagnosis of AIH and PBC.
METHODS: Serum samples were collected from 20 patients with PBC, 19 patients with AIH, and 25 healthy individuals. UPLC-MS data of the samples were analyzed using principal component analysis, partial least squares discrimination analysis and orthogonal partial least squares discrimination analysis.
RESULTS: The partial least squares discrimination analysis model (R2Y=0.991, Q2=0.943) was established between the AIH and PBC groups and exhibited both sensitivity and specifcity of 100%. Five groups of biomarkers were identifed, including bile acids, free fatty acids, phosphatidylcholines, lysolecithins and sphingomyelin. Bile acids signifcantly increased in the AIH and PBC groups compared with the healthy control group. The other biomarkers decreased in the AIH andPBC groups compared with those in the healthy control group. In addition, the biomarkers were downregulated in the AIH group compared with the PBC group.
CONCLUSIONS: The biomarkers identifed revealed the pathophysiological changes in AILD and helped to discriminate between AIH and PBC. The predictability of this method suggests its potential application in the diagnosis of AILD.
(Hepatobiliary Pancreat Dis Int 2015;14:413-421)
autoimmune liver disease;
biomarkers;
metabolomics;
autoimmune hepatitis;
primary biliary cirrhosis;
overlap syndrome
Introduction
Autoimmune liver disease (AILD) is characterized by self-perpetuating infammation of the liver with indeterminated causes.[1]AILD includes autoimmune hepatitis (AIH), primary biliary cirrhosis (PBC), primary sclerosing cholangitis, and overlap syndrome (OS). AIH and PBC are two types of AILD with a higher incidence than PSC and OS.[2]The diagnosis of AILD is challenging due to diverse clinical and laboratory manifestations.[3,4]The diagnosis of AILD requires a combination of clinical features, abnormal liver biochemical patterns, auto-antibodies and abnormal liver histology.[4,5]However, liver biochemical patterns and auto-antibody levels are not pathogenic or required for disease.[6]Furthermore, atypical liver histology confounds the diagnosis.[7,8]Differentiating between AIH and PBC is diffcult because of non-specifc behaviors and the overlap of diseases, but the differentiation is important because the treatment regimens for AIH and PBC are different. Although PBC is currently treated with ursodeoxy-cholic acid,[9,10]AIH is mainly treated with prednisolone/ prednisone with or without azathioprine.[11]
In previous studies[12,13]on the diagnosis of AILD, proteomic analyses were performed to identify many auto-antibodies. However, auto-antibodies are insuffcient to diagnose AILD.[6,14,15]Antimitochondrial antibodies are present in >90% of PBC patients,[16-18]and no antibody is highly specifc in patients with AIH. Many scoring systems have been designed for the diagnosis of AILD. Three criteria for the diagnosis of AIH have been proposed by the International Autoimmune Hepatitis Group.[19-21]Compared with the revised criteria in 1999, which were primarily designed for research purposes, the simplifed scoring system has enhanced clinical applicability and practicability.[22]The revised original scoring system performs well in patients with few or atypical features of AIH, whereas the simplifed system is better at excluding the diagnosis in diseases with concurrent immune manifestations.[23]However, the specifcity of the revised original scoring system is not satisfactory, whereas the specifcity of the simplifed system is low. Furthermore, these scoring systems list liver biopsy results as a criterion. Although being a generally safe procedure, liver biopsy carries a risk of complications.[24]Therefore, developing new methods to detect AILD accurately is important.
With the development of high-throughput methods, "omic" studies have become important to elucidate biological processes. As the products of cellular adjustment processes, metabolites levels are regarded as the ultimate readouts for genetic or environmental changes in biological systems.[25,26]Metabolomic methods have been used for clinical diagnosis and drug discovery. Using these methods, researchers have discovered many specifc biomarkers and successfully diagnosed several diseases.[27-29]Previous studies used metabolomic methods for the diagnosis of biliary tract cancer, renal cell carcinoma, and diabetes mellitus.[30-32]These studies suggested that the accuracy and predictability of these methods can augment current diagnostic approaches. However, no study has characterized AILD using metabolomic methods.
Nuclear magnetic resonance spectroscopy and gas or liquid chromatography coupled to mass spectrometry (GC-MS and LC-MS, respectively) are common tools for metabolomic studies.[33,34]In contrast to nuclear magnetic resonance and GC-MS, LC-MS has higher resolution and sensitivity and is considered to be a powerful tool to obtain rapidly and effectively multiparametric metabolite profles from biological fuids.[35]In this study, we evaluated the feasibility of a metabolomic method to diagnose AILD. Our method was based on ultraperformance liquid chromatography (UPLC)-MS; we evaluated two common AILDs, AIH and PBC. This study aimed to determine whether the metabolic profles were different between AIH and PBC, to identify specifc metabolomic markers, and to establish a model for the diagnosis of AIH and PBC.
Methods
Study population
We selected 19 patients with AIH and 20 with PBC who were hospitalized at the First Affliated Hospital of Zhejiang University School of Medicine (Hangzhou, China) from March 2009 to December 2010. The study protocol was approved by the Ethics Committee of the hospital and written informed consent was provided by all enrolled patients. The patients with AIH were diagnosed according to the revised criteria proposed by the International Autoimmune Hepatitis Group in 1999. Their scores confrmed defnitely the diagnosis of AIH.[20]Patients with PBC were diagnosed according to the entry criteria for clinical trials of PBC based on the recommendations of the American Association for the Study of Liver Diseases.[36]Patients taking medication or supplements, or those with gallstones diseases or other factors that cause cholestatic abnormal liver profles were excluded. In both groups, patients with primary sclerosing cholangitis, OS (such as PBC and AIH or AIH and primary sclerosing cholangitis), hepatitis virus infection, HIV co-infection, hepatocellular carcinoma, or diabetes were excluded. Twenty-fve healthy persons who visited our hospital for physical check-ups were recruited as healthy controls. These individuals exhibited normal liver functions and had no evidence of disease. No statistically signifcant differences in age and gender were found among the PBC, AIH and control groups (Table 1, P>0.05).
Sample collection
At admission, before breakfast and initiation of drug treatment, blood was taken from 39 patients and 25 healthy individuals and centrifuged at 3600×g for 6 minutes at 4 ℃. Blood serum was transferred into tubes and stored at -80 ℃ until analysis.
Chemicals
Acetonitrile, isopropyl alcohol, formic acid, methanol, leucine enkephalin (HPLC grade), bile acid, sphingomyelin, lysophosphatidylcholine and fat acid standards were purchased from Sigma-Aldrich (St. Louis, MO, USA). Distilled water was fltered through a Milli-Q system (Millipore, Bedford, MA, USA).
UPLC-MS analysis
The serum samples were thawed at 4 ℃. Eight qual-ity control serum samples were prepared by mixing equal amounts of serum samples from 10 AIH patients, 10 PBC patients and 10 healthy controls. All serum samples were mixed with acetonitrile at a 1:3 ratio (v/v), shaken vigorously and centrifuged at 14 000 rpm for 20 minutes. The clear supernatants were placed into glass inserts in UPLC vials and randomized.

Table 1. Demographic and clinical data
Chromatography
Chromatographic separation was performed using the 100×2.1 mm ACQUITY 1.7 μm column (Waters, Milford, MA, USA) in the ACQUITY UPLC system. In the positive ion mode, the mobile phase A was water/ formic acid (99.9:0.1, v/v) and the mobile phase B was acetonitrile/isopropyl alcohol/formic acid (79.9:20:0.1, v/v). In the negative ion mode, the mobile phase A was water/formic acid (99.9:0.1, v/v) and the mobile phase B was methanol/formic acid (99.9:0.1, v/v). The column was maintained at 50 ℃. The composition of the mobile phase B was changed from 3% to 97% in 16 minutes, maintained for 5 minutes, reached 100% in 1 minute, and was held for 5 minutes. The temperature of the sample manager was set to 4 ℃, and the injection volume was 5 μL for each analysis. The column eluent was split to direct approximately 100 μL/min to the mass spectrometer.
MS
MS was performed using a Waters Q-TOF Premier (Waters MS Technologies, Manchester, UK) with positive and negative ion modes. The nebulization gas was released at 450 L/h at a temperature of 350 ℃. The cone gas was set to 50 L/h with a source temperature of 120 ℃. For the positive ion mode, the capillary voltage was 3.0 kV and the sampling cone voltage was set to 40 V. For the negative ion mode, the capillary voltage was set to 2.5 kV and the sampling cone voltage was set to 40 V. MS was performed in the V optics mode with 9000 resolution. The acquisition rate of data was set to 0.3 second with a 0.02-second inter-scan delay. All analyses were acquired using the lock spray to ensure accuracy and reproducibility. The instrument was previously calibrated with sodium formate. The lock mass spray for precise mass determination was set using leucine enkephalin at m/z 556.2771 at a concentration of 0.5 ng/μL in the positive ion mode and m/z 554.2615 in the negative ion mode. The lock spray frequency was set to 5 seconds, and the lock mass was averaged over 10 scans. Mass spectra were acquired over the scanning range of m/z 50-1000. Metabolites were identifed using LC-MS/MS. The product ions were detected over a scanning range of m/z 50-1000. The collision voltage was set between 5 and 60 V, and argon was used as the collision gas. Identifcation of the metabolites was confrmed by comparison with authentic standards.
Data processing
We used Mass Lynx version 4.1 software to pre-process the data including retention time and m/z that were obtained from UPLC-MS analysis. The data were aligned and normalized during this process. To refect the differences among the three groups, multivariate statistical analysis was performed using SIMCA-P+12.0. Pareto scaling was used in all of the models to avoid chemical noise. The data were exported and assessed using principal component analysis (PCA), partial least squares discrimination analysis (PLS-DA), and orthogonal partial least squares discrimination analysis (OPLS-DA). Potential biomarkers were selected according to the variable importance for project value, the loading plot, and the S-plot. SPSS version 16.0 was used for statistical analysis. For the identifcation of potential markers, the followingdatabases were used: HMDB (www.hmdb.ca), METLIN (metlin.scripps.edu), Mass Bank (http://www.massbank. jp/), Pub Chem (http://pubchem.ncbi.nlm.nih.gov/) and KEGG (www.genome.jp/kegg/ligand.html). The PLS-DA model was established to discriminate between AIH and PBC cohorts. The receiver operating characteristic (ROC) analysis was used to cross-validate predicted Y values, while verifying the robustness of the metabolomic model.
External validation
To evaluate the predictive ability of the PLS-DA model for new samples, 12 independent samples were used, including samples from four patients with AIH, four patients with PBC and four patients with AIH-PBC OS. The diagnostic criteria for AIH and PBC were the same as mentioned above. AIH-PBC OS was diagnosed according to the Paris Diagnostic Criteria.[37-39]Clinical characteristics of the samples used for external validation are summarized in Table 1. The sensitivity and specifcity of the PLS-DA model for the prediction of new samples were calculated.
Results
Validation of the analytical performance
A total of 64 samples taken from 20 patients with PBC, 19 patients with AIH and 25 healthy controls were analyzed in the positive and negative ion modes. The plots of PCA scores showed that the quality control samples were tightly clustered, confrming that our method was reproducible. Variations in marker metabolites were further observed in quality control samples, which were used to evaluate the overall performance of our method.[40]We calculated the coeffcient of variance (CV) of all markers identifed in quality control samples. The percentage CV ranged from 3.2% to 10.3% with a median CV of 6.7%, which showed satisfactory reproducibility (Table 2).
Serum metabolomics of AIH and PBC
A total of 3019 peaks of positive ions and 3129 peaks of negative ions were detected using MassLynx by the same acquisition method. The data were imported into SIMCA-P+12 for PCA. Plots of the scores of PCA with positive and negative ion modes are shown in Fig. 1A and B. In the positive ion mode, the patients and controls were separated exclusively. However, the AIH and PBC groups were not clearly separated, resulting in poor discrimination. In the negative ion mode, distinct clustering was observed between the patients and controls. Furthermore, AIH and PBC patients were separated into two distinct regions.
Despite limitations, PCA can provide an overview of the pre-processed data.[41]To better characterize theserum metabolite profle of AIH and PBC patients, supervised PLS-DA models were established based on the two disease groups with positive and negative ion modes. R2Y (cum) and Q2(cum) parameters, which indicated the ftness and predictability respectively, were used to evaluate the effcacy of the models. The results showed that the effcacy of the PLS-DA model using the positive ion mode was low (R2Y=0.492, Q2=0.292), indicating that the metabolomic profling of human blood did not display signifcant differences between PBC and AIH patients. Conversely, the model using the negative ion mode displayed good effcacy (R2Y=0.991, Q2=0.943) (Fig. 1C). This fnding prompted us to hypothesize that the two diseases are discernable using UPLC-MS with the negative ion mode. Therefore, the negative ion mode was used in our subsequent experiments.

Table 2. Identifed markers of the PBC and AIH groups
Marker identifcation
Analysis of PLS-DA S-plot (Fig. 1D) and the variable importance for projects indicated several discriminatory metabolites that differentiated between AIH and PBC samples. An independent samples t test was performed, and variables without signifcant differences were eliminated between the AIH and PBC groups (P>0.05). The molecular ionization form (protonated or sodiated) and fragments corresponding to theoretical and standard fragments were used in marker identifcation.[42]
One of the ions identifed from the loading plot as being responsible for the variance in the data set was the [M-CH3]-ion m/z 685.5319, eluting with a retention time of 16.41 minutes in the UPLC separation (Fig. 2A). According to its MS spectrum, the signal at m/z 685.5319 was derived from a [M+HCOOH-H]-ion m/z 747.5549 as well as [M-CH3]-ions generated by in-source fragmentation. MS/MS spectra of selected ion m/z 745.5549 were acquired to determine their fragmentation products and to confrm their structural assignments. MS/MS analysis of this [M+HCOOH-H]-ion m/z 745.5549 gave rise to the major ions m/z 168.0465 (demethylated phosphoryl choline), m/z 685.5319 ([M-CH3]-) and m/z 78.9639 (phosphoryl group) in the negative ion mode (Fig. 2B). The fragmentation pattern of the spectra obtained for sphingomyelin (SM) (d18:0/16:1) standard was similar to the MS/MS spectra (Fig. 2C). Thus, we identifed this compound as SM (d18:0/16:1). Using this method, we identifed fve groups of markers, including four bile acids (BAs), three free fatty acids (FFAs), nine phosphatidylcholines (PCs), two lysolecithins (LPCs) and SM (d18:0/16:1). Fig. 3 shows the serum levels of glycochenodeoxycholic acid, FFA, LPC-16:0, PC-16:0/16:0, and SM during the PBC, AIH and healthy control groups. Table 2 shows the detailed list of themarkers, and Fig. 1D indicates the identifed markers using red triangles.
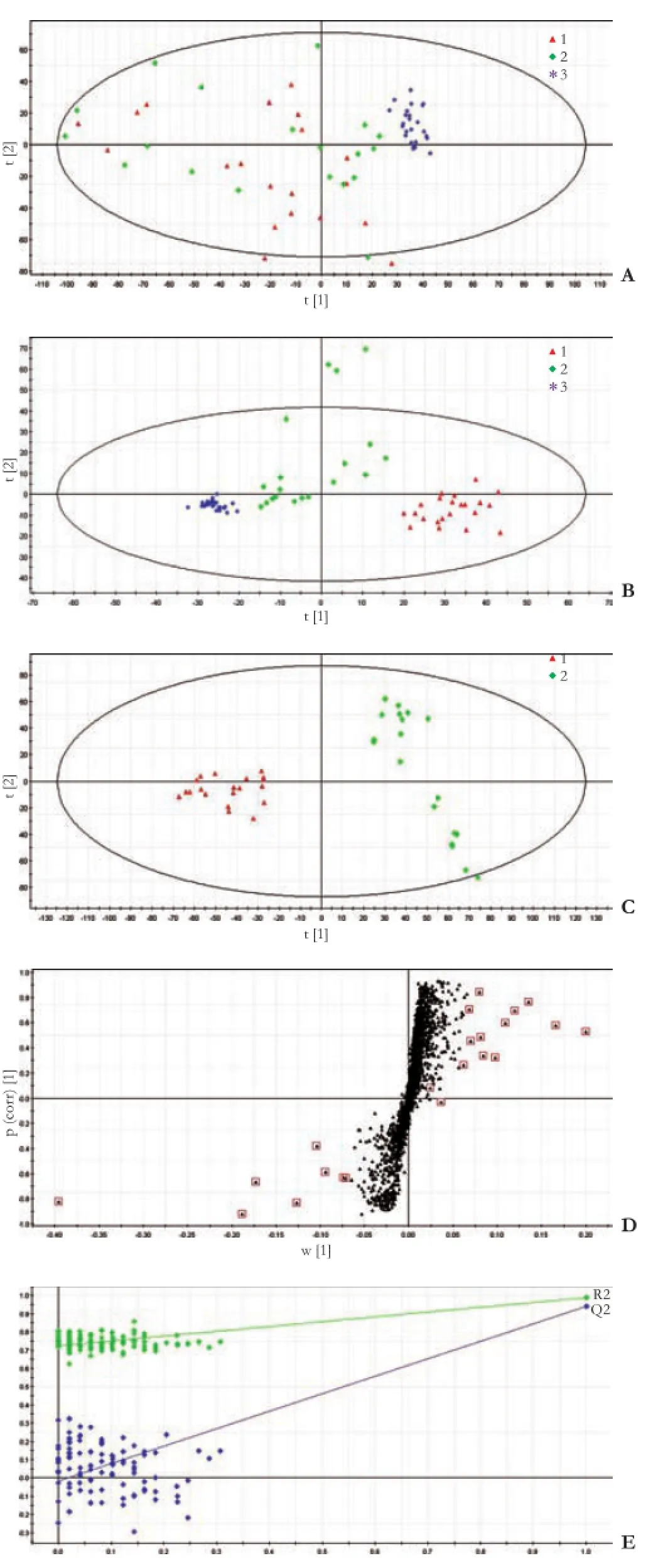
Fig. 1. A: plots of PCA with a positive ion mode. B; plots of PCA with a negative ion mode; C: scatter plots of PLS-DA with a negative model of serum from patients with PBC and AIH; D: loadings scatter plots of PLS-DA with a negative model; E: validation plot of the original PLS-DA with a negative model, which strongly indicates that the original model is valid and shows no signs of overftting. 1: patients with PBC; 2: patients with AIH; 3: quality control.

Fig. 2. A: A mass spectrum of ion m/z 685.5319; B: MS/MS spectra of selected ion m/z 745.5549; C: MS/MS spectra of SM (d18:0/16:1) standard.
Model effcacy

Fig. 3. Mean intensity of GCDCA (A), FFA (B), LPC (C), PC (D), and SM (E) in the PBC, AIH and healthy control groups. GCDCA: glycochenodeoxycholic acid; FFA: free fatty acid; LPC: lysolecithin; PC: phosphatidylcholine; SM: sphingomyelin; PBC: primary biliary cirrhosis; AIH: autoimmune hepatitis.
The goodness of ft (R2Y=0.991, Q2=0.943) of the original PLS-DA model and clustering of 100 Y-permutated models were visualized using a validation plot (Fig. 1E). The validation plot strongly indicated that the original model was valid and showed no signs of overftting. In addition, the area under the ROC curve of the PLS-DA model was calculated using cross-validated Y-predicted values, which were set to 1, and confrmed the validity of the model. A prediction value of Y≥0.5 was the optimal value for discrimination between the AIH and PBC groups with a sensitivity of 100% and a specifcity of 100%.
External validation
The AIH and PBC groups were used to examine the predictive ability of the PLS-DA model for each disease, with a sensitivity of 100% and a specifcity of 100% (Fig. 4).
Fig. 4. ROC curve determined with the cross-validated predicted Y-values.
Discussion
The prognosis of patients with AILD is poor, but it can be improved by adequate therapy.[43,44]Early diagnosis of AILD is particularly important; however, current diagnostic methods such as autoantibody detection have limited sensitivity and specifcity.[6]In our study, a PLSDA model was established using a highly reproducible UPLC-MS metabolomic method.
Low variations in the levels of peaks in quality control samples confrmed that our data were accurate and that our method was highly reproducible.[40]In the S-plots of PCA with the negative ion mode, the group clusters were denser than those observed with the positive ion mode. These results indicated that some potential markers that might be used to differentiate the samples could not be ionized with the positive mode. Consequently, we used the negative ion mode to differentiate between the two disease groups. The blood metabolic phenotypes generated by AIH and PBC were significantly different from each other using UPLC-MS. In the PLS-DA model, the R2Y and Q2values were 0.991 and 0.943, respectively. The area under the ROC curve was 1 with a sensitivity of 100% and a specifcity of 100%. This PLS-DA model accurately diagnosed AIH and PBC. The patients with AIH and PBC for external validation were correctly diagnosed by the PLS-DA model. These results confrmed the feasibility of the LC-MS-based serum metabolomic method for the diagnosis of PBC and AIH. Obviously, four samples of AIH-PBC OS for external validation did not integrate into any group in the T-predicted scatter plot of the PLS-DA model. This fnding indicated that this disease has a unique metabolic profle. However, further investigation with more samples is required to validate this presumption.
A simplifed OPLS-DA model was established using the identifed markers and the top fve variable importance for project value. These markers included glycochenodeoxycholic acid, FFA, LPC-16:0, PC-16:0/16:0, and SM. The R2Y and Q2values of the OPLS model were 0.872 and 0.810, respectively. The area under the ROC curve was 1 with a sensitivity of 100% and a specifcity of 100% respectively. This result showed that the simplifed model can also be used to diagnose AIH and PBC accurately.
In our study 5 groups of markers were identifed, suggesting two pathways that mediate AILD. The frst pathway mediates a metabolic disorder of BAs, whereas the second pathway mediates the derangement of lipid metabolism.
PBC is a chronic disease with unexplained liver interlobular bile duct damage. Cholestasis as a key feature of PBC is caused by ductal cholestasis in the early stages. Canalicular cholestasis is a secondary consequence of the outfow functional blockade.[4]All BAs showed the same trend in our study and the intensity distribution of glycochenodeoxycholic acid in the three groups was typical among the BAs identifed. As shown in Fig. 3A, glycochenodeoxycholic acid was signifcantly increased in the PBC group compared with that in the healthy control group. In contrast, serum glycochenodeoxycholic acid was mildly increased in the AIH group compared with that in the healthy control group. The mild increase of BA in AIH is caused by liver cell injury. When liver failure occurs, decreased hepatic clearance of BAs increases their serum level.[45]
The derangement of lipid metabolism in our study was characterized by decreased serum levels of FFA, LPC, PC and SM. All markers of the four groups showed the same trend (Fig. 3B-E). We noted that this derangement was alleviated in the AIH group compared with the PBC group. These results were similar to those of a previous study showing lithocholic acid (LCA)-dependent decreases in lipid levels.[46]The hepatic level of LCA was reported to elevate in patients with cholestatic liver disease.[47,48]Moreover, LCA decreased the levels of phospholipids, SM, FFAs, and triglycerides,[46,49,50]and it was detoxifed via hepatic biotransformation using two pathways. One is hydroxysteroid-sulfotransferase-mediated LCA sulfation, and the other is hydroxylation reaction that is catalyzed by the cytochrome P450 enzymes.[51,52]When liver function was damaged, liver biotransformation function decreased, including hydroxysteroidsulfotransferase-mediated LCA sulfation. Therefore, we assumed that higher levels of LCA might cause lipid metabolism disorders via the frst pathway in AIH and PBC. Previous studies[53,54]indicated that the activation of cytochrome P450 correlates with farnesoid X receptor. Mammalian farnesoid X receptor, which is a transcription regulatory factor in bile salt synthesis, is activatedby bile acids such as chenodeoxycholic acid or LCA.[50,55]The derangements of lipid metabolism are weakened in farnesoid X receptor-null mice compared with those in wild-type mice after LCA exposure.[6,52]As a cholestatic liver disease, the high level of BAs may induce farnesoid X receptor gene transcription in PBC. The level of BAs in AIH was lower than that of active farnesoid X receptor gene transcription (Fig. 3A). Therefore, we hypothesized that these pathways may lead to LCA poisoning in PBC patients, and that the frst pathway is predominantly active in PBC patients. This hypothesis may explain why lipid metabolism disorder was milder in patients with AIH than those with PBC. This assumption needs to be validated in further investigations.
In conclusion, our study showed that metabolomic methods were accurate for the diagnosis of AIH and PBC. This study was frst to use a metabolomic approach for the diagnosis of AILD; therefore follow-up investigations are required. We believed that these fndings will help to develop a dependable diagnostic tool based on metabolomic methods for the diagnosis of AILD.
Contributors:HJR designed the study. LJS and LW performed the majority of experiments. HSR, CDY, WYY, YJL and JHY provided analytical tools and were also involved in editing the manuscript. LJS and LW wrote the manuscript, and contributed equally to this study. HJR is the guarantor.
Funding:This study was supported by grants from the National Grand Program on Key Infectious Diseases (2012ZX10002-004) and the National Natural Science Foundation of China (81100286).
Ethical approval:Not needed.
Competing interest:No benefts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Czaja AJ. Autoimmune liver disease. Curr Opin Gastroenterol 2009;25:215-222.
2 Feld JJ, Heathcote EJ. Epidemiology of autoimmune liver disease. J Gastroenterol Hepatol 2003;18:1118-1128.
3 Mieli-Vergani G, Vergani D. Autoimmune paediatric liver disease. World J Gastroenterol 2008;14:3360-3367.
4 Poupon R. Primary biliary cirrhosis: a 2010 update. J Hepatol 2010;52:745-758.
5 Bayer EM, Schramm C, Kanzler S, Lohse AW. Autoimmune liver disease: diagnosis and therapy. Z Gastroenterol 2004;42: 19-30.
6 Bogdanos DP, Invernizzi P, Mackay IR, Vergani D. Autoimmune liver serology: current diagnostic and clinical challenges. World J Gastroenterol 2008;14:3374-3387.
7 Zen Y, Notsumata K, Tanaka N, Nakanuma Y. Hepatic centrilobular zonal necrosis with positive antinuclear antibody: a unique subtype or early disease of autoimmune hepatitis? Hum Pathol 2007;38:1669-1675.
8 Miyake Y, Iwasaki Y, Terada R, Onishi T, Okamoto R, Takaguchi K, et al. Clinical features of Japanese type 1 autoimmune hepatitis patients with zone III necrosis. Hepatol Res 2007;37: 801-805.
9 Heathcote EJ. Management of primary biliary cirrhosis. The American Association for the Study of Liver Diseases practice guidelines. Hepatology 2000;31:1005-1013.
10 European Association for the Study of the Liver. EASL Clinical Practice Guidelines: management of cholestatic liver diseases. J Hepatol 2009;51:237-267.
11 Lamers MM, van Oijen MG, Pronk M, Drenth JP. Treatment options for autoimmune hepatitis: a systematic review of randomized controlled trials. J Hepatol 2010;53:191-198.
12 Song Q, Liu G, Hu S, Zhang Y, Tao Y, Han Y, et al. Novel autoimmune hepatitis-specifc autoantigens identifed using protein microarray technology. J Proteome Res 2010;9:30-39.
13 Tahiri F, Le Naour F, Huguet S, Lai-Kuen R, Samuel D, Johanet C, et al. Identifcation of plasma membrane autoantigens in autoimmune hepatitis type 1 using a proteomics tool. Hepatology 2008;47:937-948.
14 Czaja AJ. Autoimmune liver disease. Curr Opin Gastroenterol 2008;24:298-305.
15 Bogdanos DP, Mieli-Vergani G, Vergani D. Autoantibodies and their antigens in autoimmune hepatitis. Semin Liver Dis 2009;29:241-253.
16 Michieletti P, Wanless IR, Katz A, Scheuer PJ, Yeaman SJ, Bassendine MF, et al. Antimitochondrial antibody negative primary biliary cirrhosis: a distinct syndrome of autoimmune cholangitis. Gut 1994;35:260-265.
17 Liu B, Shi XH, Zhang FC, Zhang W, Gao LX. Antimitochondrial antibody-negative primary biliary cirrhosis: a subset of primary biliary cirrhosis. Liver Int 2008;28:233-239.
18 Mendes F, Lindor KD. Antimitochondrial antibody-negative primary biliary cirrhosis. Gastroenterol Clin North Am 2008; 37:479-484.
19 Johnson PJ MI. Meeting report: International Autoimmune Hepatitis Group. Hepatology 1993;18:998-1005.
20 Alvarez F, Berg PA, Bianchi FB, Bianchi L, Burroughs AK, Cancado EL, et al. International Autoimmune Hepatitis Group Report: review of criteria for diagnosis of autoimmune hepatitis. J Hepatol 1999;31:929-938.
21 Hennes EM, Zeniya M, Czaja AJ, Parés A, Dalekos GN, Krawitt EL, et al. Simplifed criteria for the diagnosis of autoimmune hepatitis. Hepatology 2008;48:169-176.
22 Muratori P, Granito A, Pappas G, Muratori L. Validation of simplifed diagnostic criteria for autoimmune hepatitis in Italian patients. Hepatology 2009;49:1782-1783.
23 Czaja AJ. Performance parameters of the diagnostic scoring systems for autoimmune hepatitis. Hepatology 2008;48:1540-1548.
24 Denzer U, Helmreich-Becker I, Galle PR, Lohse AW. Liver assessment and biopsy in patients with marked coagulopathy: value of mini-laparoscopy and control of bleeding. Am J Gastroenterol 2003;98:893-900.
25 Clayton TA, Lindon JC, Cloarec O, Antti H, Charuel C, Hanton G, et al. Pharmaco-metabonomic phenotyping and personalized drug treatment. Nature 2006;440:1073-1077.
26 Blow N. Metabolomics: Biochemistry's new look. Nature 2008; 455:697-700.
27 Ellis DI, Dunn WB, Griffn JL, Allwood JW, Goodacre R. Metabolic fngerprinting as a diagnostic tool. Pharmacogenomics 2007;8:1243-1266.
28 Yin P, Wan D, Zhao C, Chen J, Zhao X, Wang W, et al. A metabonomic study of hepatitis B-induced liver cirrhosis and hepatocellular carcinoma by using RP-LC and HILIC coupled with mass spectrometry. Mol Biosyst 2009;5:868-876.
29 Sreekumar A, Poisson LM, Rajendiran TM, Khan AP, Cao Q, Yu J, et al. Metabolomic profles delineate potential role for sarcosine in prostate cancer progression. Nature 2009;457:910-914.
30 Wen H, Yoo SS, Kang J, Kim HG, Park JS, Jeong S, et al. A new NMR-based metabolomics approach for the diagnosis of biliary tract cancer. J Hepatol 2010;52:228-233.
31 Lin L, Huang Z, Gao Y, Yan X, Xing J, Hang W. LC-MS based serum metabonomic analysis for renal cell carcinoma diagnosis, staging, and biomarker discovery. J Proteome Res 2011;10: 1396-1405.
32 Zhang J, Yan L, Chen W, Lin L, Song X, Yan X, et al. Metabonomics research of diabetic nephropathy and type 2 diabetes mellitus based on UPLC-oaTOF-MS system. Anal Chim Acta 2009;650:16-22.
33 Montoliu I, Martin FP, Collino S, Rezzi S, Kochhar S. Multivariate modeling strategy for intercompartmental analysis of tissue and plasma 1H NMR spectrotypes. J Proteome Res 2009;8:2397-2406.
34 Yu K, Sheng G, Sheng J, Chen Y, Xu W, Liu X, et al. A metabonomic investigation on the biochemical perturbation in liver failure patients caused by hepatitis B virus. J Proteome Res 2007;6:2413-2419.
35 Zelena E, Dunn WB, Broadhurst D, Francis-McIntyre S, Carroll KM, Begley P, et al. Development of a robust and repeatable UPLC-MS method for the long-term metabolomic study of human serum. Anal Chem 2009;81:1357-1364.
36 Silveira MG, Brunt EM, Heathcote J, Gores GJ, Lindor KD, Mayo MJ. American Association for the Study of Liver Diseases endpoints conference: design and endpoints for clinical trials in primary biliary cirrhosis. Hepatology 2010;52:349-359.
37 Kuiper EM, Zondervan PE, van Buuren HR. Paris criteria are effective in diagnosis of primary biliary cirrhosis and autoimmune hepatitis overlap syndrome. Clin Gastroenterol Hepatol 2010;8:530-534.
38 Chazouillères O, Wendum D, Serfaty L, Montembault S, Rosmorduc O, Poupon R. Primary biliary cirrhosis-autoimmune hepatitis overlap syndrome: clinical features and response to therapy. Hepatology 1998;28:296-301.
39 Boberg KM, Chapman RW, Hirschfeld GM, Lohse AW, Manns MP, Schrumpf E; International Autoimmune Hepatitis Group. Overlap syndromes: the International Autoimmune Hepatitis Group (IAIHG) position statement on a controversial issue. J Hepatol 2011;54:374-385.
40 Want EJ, Wilson ID, Gika H, Theodoridis G, Plumb RS, Shockcor J, et al. Global metabolic profling procedures for urine using UPLC-MS. Nat Protoc 2010;5:1005-1018.
41 Boccard J, Veuthey JL, Rudaz S. Knowledge discovery in metabolomics: an overview of MS data handling. J Sep Sci 2010;33:290-304.
42 Lin L, Yu Q, Yan X, Hang W, Zheng J, Xing J, et al. Direct infusion mass spectrometry or liquid chromatography mass spectrometry for human metabonomics? A serum metabonomic study of kidney cancer. Analyst 2010;135:2970-2978.
43 Hohenester S, Oude-Elferink RP, Beuers U. Primary biliary cirrhosis. Semin Immunopathol 2009;31:283-307.
44 Wiegard C, Schramm C, Lohse AW. Scoring systems for the diagnosis of autoimmune hepatitis: past, present, and future. Semin Liver Dis 2009;29:254-261.
45 Vlahcevic ZR, Pandak WM, Stravitz RT. Regulation of bile acid biosynthesis. Gastroenterol Clin North Am 1999;28:1-25.
46 Matsubara T, Tanaka N, Patterson AD, Cho JY, Krausz KW, Gonzalez FJ. Lithocholic acid disrupts phospholipid and sphingolipid homeostasis leading to cholestasis in mice. Hepatology 2011;53:1282-1293.
47 Fischer S, Beuers U, Spengler U, Zwiebel FM, Koebe HG. Hepatic levels of bile acids in end-stage chronic cholestatic liver disease. Clin Chim Acta 1996;251:173-186.
48 Setchell KD, Rodrigues CM, Clerici C, Solinas A, Morelli A, Gartung C, et al. Bile acid concentrations in human and rat liver tissue and in hepatocyte nuclei. Gastroenterology 1997;112:226-235.
49 Boyer JL, Trauner M, Mennone A, Soroka CJ, Cai SY, Moustafa T, et al. Upregulation of a basolateral FXR-dependent bile acid effux transporter OSTalpha-OSTbeta in cholestasis in humans and rodents. Am J Physiol Gastrointest Liver Physiol 2006;290: G1124-1130.
50 Eloranta JJ, Kullak-Ublick GA. The role of FXR in disorders of bile acid homeostasis. Physiology (Bethesda) 2008;23:286-295.
51 Hofmann AF. Detoxifcation of lithocholic acid, a toxic bile acid: relevance to drug hepatotoxicity. Drug Metab Rev 2004;36: 703-722.
52 Kitada H, Miyata M, Nakamura T, Tozawa A, Honma W, Shimada M, et al. Protective role of hydroxysteroid sulfotransferase in lithocholic acid-induced liver toxicity. J Biol Chem 2003;278:17838-17844.
53 Akiyama TE, Gonzalez FJ. Regulation of P450 genes by liverenriched transcription factors and nuclear receptors. Biochim Biophys Acta 2003;1619:223-234.
54 Krasowski MD, Ni A, Hagey LR, Ekins S. Evolution of promiscuous nuclear hormone receptors: LXR, FXR, VDR, PXR, and CAR. Mol Cell Endocrinol 2011;334:39-48.
55 Jeffcoat R. Obesity-a perspective based on the biochemical interrelationship of lipids and carbohydrates. Med Hypotheses 2007;68:1159-1171.
Received August 7, 2014
Accepted after revision January 9, 2015
Author Affliations: Collaborative Innovation Center for Diagnosis and Treatment of Infectious Diseases; State Key Laboratory for Diagnosis and Treatment of Infectious Disease, First Affliated Hospital, Zhejiang University School of Medicine, Hangzhou 310003, China (Lian JS, Hao SR, Chen DY, Wang YY, Yang JL, Jia HY and Huang JR); Yantai City Hospital for Infectious Diseases, Yantai 264000, China (Liu W)
Jian-Rong Huang, MD, Collaborative Innovation Center for Diagnosis and Treatment of Infectious Diseases; State Key Laboratory for Diagnosis and Treatment of Infectious Disease, First Affliated Hospital, Zhejiang University School of Medicine, 79 Qingchun Road, Hangzhou 310003, China (Tel: +86-571-87236456; Email: hzhuangchina@sina.com)
© 2015, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(15)60393-9
Published online July 2, 2015.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Meetings and Courses
- A liver donor with double hepatic artery aneurysm: a saved graft
- Impact of venous thromboembolism on the natural history of pancreatic adenocarcinoma
- Pancreaticoduodenectomy with portal vein/superior mesenteric vein resection for patients with pancreatic cancer with venous invasion
- Influence of comorbidity on outcomes of older patients with acute pancreatitis based on a national administrative database
- The response of Golgi protein 73 to transcatheter arterial chemoembolization in patients with hepatocellular carcinoma may relate to the influence of certain chemotherapeutics
