Relationship between intubation rate and continuous positive airway pressure therapy in the prehospital setting
2015-02-07
Department of Emergency Medicine and Department of Medicine Division of Pulmonary Disease, Hackensack University Medical Center, 30 prospect Ave Hackensack N.J., 07601, USA
Relationship between intubation rate and continuous positive airway pressure therapy in the prehospital setting
Nigel Knox, Ogedegbe Chinwe, Nyirenda Themba, Feldman Joseph, Ashtyani Hormoz
Department of Emergency Medicine and Department of Medicine Division of Pulmonary Disease, Hackensack University Medical Center, 30 prospect Ave Hackensack N.J., 07601, USA
BACKGROUND:To determine whether the prehospital use of continuous positive airway pressure (CPAP) therapy is associated with a reduced rate of endotracheal intubation in patients with an acute respiratory disorder brought to the emergency department (ED).
METHODS:We reviewed medical records of patients with acute respiratory distress who had been treated with CPAP in the Mobile Intensive Care Unit (MICU) from January 2010 to December 2011. These records were compared with those of patients who received standardized care without CPAP in the MICU from January 2004 to December 2004. Categorical variables were summarized as frequencies and compared between groups using Fisher's exact test or the Chi-square test. Continuous variables were summarized as medians (interquartile range), and comparison between the groups was made using Wilcoxon's rank-sum test. The relationship between CPAP and intubation rate was determined using multivariable logistic regression analysis of propensity scores. The results were presented as odds ratio (OR), 95% confidence interval (CI), andPvalue for test effect. The adequacy of the model was calibrated using Hosmer and Lemeshow's goodness-of-f t test.P<0.05 was considered statistically signif cant.
RESULTS:The records of 785 patients were reviewed. Of the 215 patients treated with CPAP in the MICU, 13% were intubated after admission. In contrast, of the 570 patients who did not receive CPAP, 28% were intubated after ED admission. Unadjusted logistic regression analysis showed that patients who had been treated with CPAP were less likely to be intubated than those without CPAP treatment (OR=0.37, 95%CI, 0.24–0.57,P<0.0001). With propensity scores adjusted, multivariate logistic regression analysis showed that CPAP treatment was associated with a 62% reduction of intubation (OR=0.384, 95%CI, 0.25–0.60,P≤0.0001).
CONCLUSIONS:In patients with acute respiratory disorder, there was a relationship between CPAP therapy and the decreased intubation rate. CPAP therapy was feasible in prehospital management of patients with respiratory distress.
Continuous positive airway pressure; Critical care; Early intervention; Emergency service; Intubation
INTRODUCTION
Continuous positive airway pressure (CPAP) therapy for sleep apnea was initiated in the 1980s.[1]Since then this therapy has been widely used for certain acute respiratory disorders. It also can significantly increase the survival rates of patients with chronic obstructive pulmonary disease (COPD)[2]and those with neuromuscular disorders.[3]In immunocompromized patients in the emergency department (ED) and ICU, CPAP is used as a therapeutic device for COPD exacerbation, congestive heart failure, post-extubation airway maintenance, and hypoxemic respiratory failure. CPAP decreases the rate of intubation.[4–6]Yet, there are few reports on the expansion of CPAP into the prehospital setting.
Because of the adverse results of intubation and sedation and paralysis that often require pre/ post intubation, the preventive step should be taken at the emergency medical service (EMS) stage. Ventilatory support via early application of CPAP can be an important factor improving outcomes in patients with acute respiratory diseases.[7]The reduction in endotracheal intubation after early respiratory support may lead to the prevention of long-term complications such as discomfort, nosocomial infection, tracheal stenosis, tracheomalacia, and inadvertent extubation.
Apart from the long-term adverse effects of intubation/mechanical ventilation, there are a number of significant concerns regarding emergency tracheal intubation.[8]Unlike intubation in a controlled setting such as operating room, emergency intubations are often carried out by paramedics (less experienced personnel) on patients in uncontrollable conditions. This setting creates more adverse results such as hemodynamic instability, pneumothorax, pulmonary aspiration, and esophageal intubation, which contribute significantly to hypoxemia, regurgitation, aspiration, bradycardia, cardiac dysrhythmias, and cardiac arrest.[9–11]
To achieve a more controlled environment in preparation for intubation, sedation/analgesia is required but it itself is associated with numerous adverse results.[12]Endotracheal intubation requires heavy sedation with neuromuscular blocking agents in critical care settings to facilitate endotracheal tube tolerance and mechanical ventilation synchronization. All of these components are subjected to their own individual complications, such as hypotension, critical care neuromyopathy, aspiration and prolonged sedation and toxic metabolic encephalopathy, which in combination may lead to a potentially dangerous treatment option which is preferably avoided.[12]
In association with the health risks discussed, the financial costs are also substantial. When an intubated patient stayed in the hospital for more than 4.5 days, additional costs would be $11 000.[13]A randomized trial[14]showed that patients with acute respiratory failure in the inpatient setting are less likely to have endotracheal intubation when CPAP is added to standard therapy.
CPAP induces adverse effects,including pneumothorax, periorbital ecchymosis, sinusitis, epistaxis, aerophagia, impeding cough, difficulty with clearance of respiratory secretions, skin abrasion/ lacerations, and hypotension. However, to avoid infections, prolonged ICU stay, and increased mortality after intubation[15,16]may far outweigh the potential complications of CPAP.
In this retrospective cohort study, we identified whether CPAP therapy could be broadened further in the prehospital setting and whether CPAP was associated with a decreased rate of subsequent complications after intubation. The study incorporated the paramedic/ EMS evaluation, CPAP treatment, and the clinical outcome of patients in the ED of a large tertiary care teaching hospital, as well as reports on prehospital CPAP treatment.[17,18]The study setting allowed the varied effects of CPAP to be further recognized using a larger sample size. With a larger population being reviewed, this study allowed for better control over the multiple variables, given its utilization of the same protocols, paramedics, ED team, and hospital staff.
While it was not a set goal of the study, following completion of the study it appeared evident that the training of the emergency medical service teams in CPAP device use, and application could easily be achieved.
METHODS
Study design
In this retrospective cohort study, we compared the rate of intubation in patients with acute respiratory distress treated with CPAP from 2010 to 2011.
Setting
The study was conducted in a 775-bed private tertiary care teaching hospital located in New Jersey, USA.
Methods and measurement
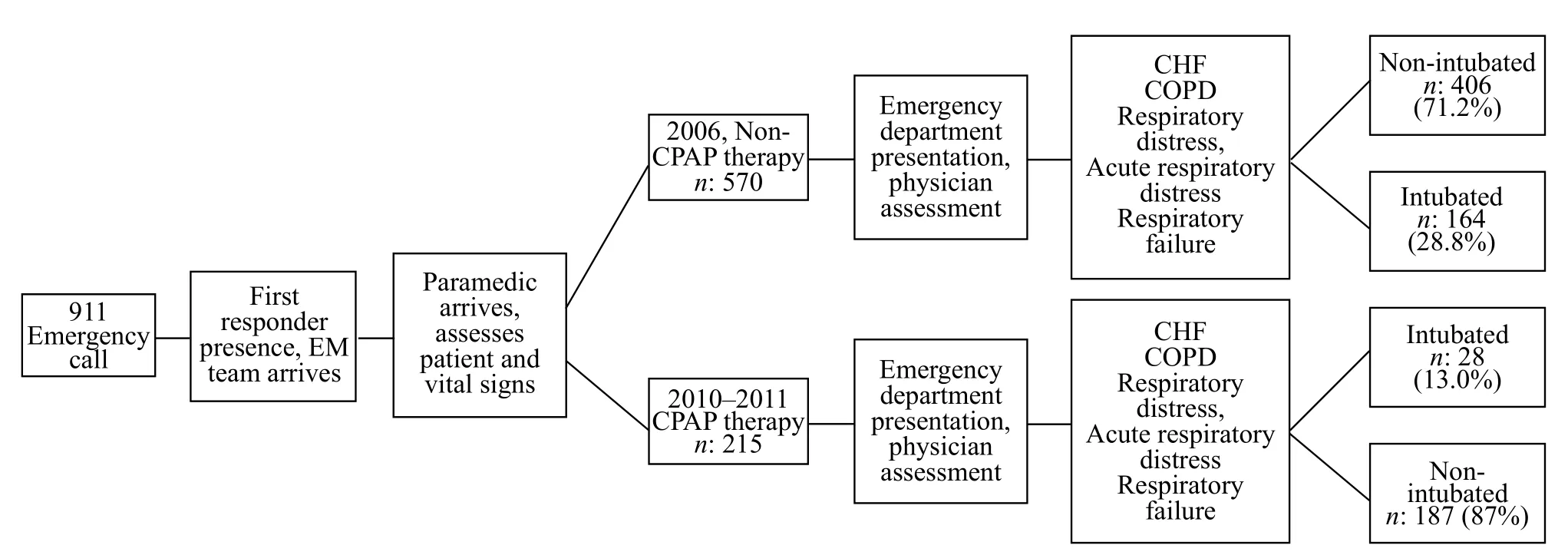
Figure 1. Development of f rst responders assessment and therapy.
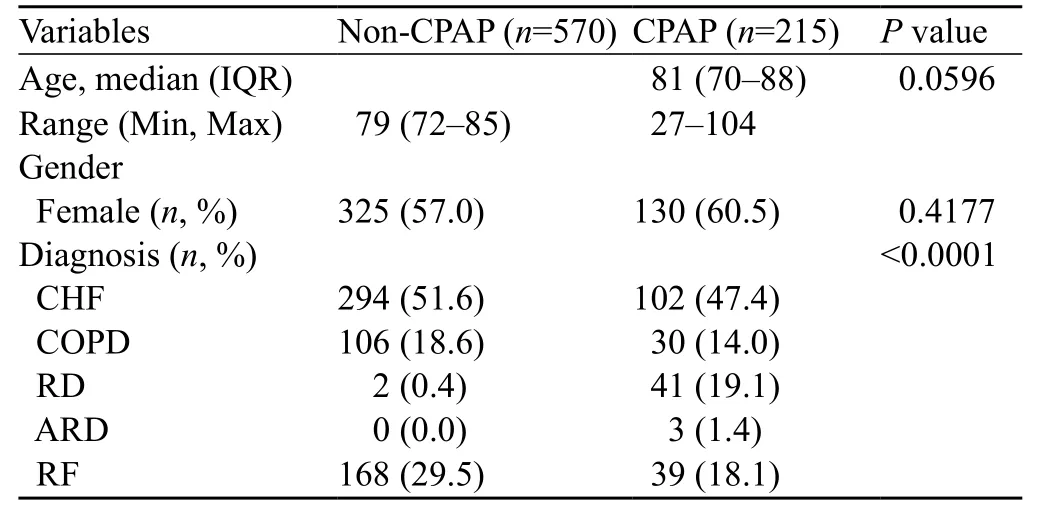
Table 1. Baseline characteristics of patients with acute respiratory disorders
To identify the relationship between CPAP treatment in a prehospital setting and intubation rate upon ED admission, we retrospectively analyzed the data of patients who were treated with CPAP before hospitalization. The data were compared with those from patients who received standard care without CPAP therapy (Figure 1).
We reviewed the records of CPAP prehospital use, and found that the medical institution's primary paramedic unit had been using CPAP as a therapeutic device since 2006. Using this information we derived the data of CPAP use from Paramedic's records of patients who underwent CPAP ventilation due to respiratory distress at the scene or en route during the period of January 1, 2010 to December 30, 2011 (Table 1). These records revealed that 215 patients had received CPAP in the prehospital setting. To minimize confounding variability, patients who had a history of CPAP use or were intubated at the scene were excluded from the study. The collected paramedic information was then correlated with the medical institution's medical records to ascertain patient data, such as age, sex, diagnosis on admission, and whether they had been intubated after admission. Following the collection of the data of the CPAP treatment group, primary diagnostic categories on admission were created for all patients involved in the study. The categories included chronic obstructive pulmonary disease exacerbation (COPD), congestive heart failure (CHF), respiratory distress (RD), acute respiratory distress (ARD), and respiratory failure (RF). The categorization of patients in ARD was one that the field team made upon initial impression, following the recognition of patients requiring respiratory assistance, regardless of the underlying etiology (Figure 2).

Figure 2. Preliminary diagnosis for groups at time of admission.
The comparison of the control group was based upon the data derived from the institution's medical records. The records pertained to patients with the primary diagnoses on admission who had not received CPAP therapy before being admitted to the ED by the EMS. To prevent any overlapping time period or pilot trials of CPAP treatment, the data of the control group were collected from January 1, 2004 to December 31, 2004. This was approximately 2 years before the use of CPAP by paramedic units in New Jersey.
The records of 1 408 patients correlated with their diagnosis during this period. The records wereindividually assessed to ascertain whether the patients had been transported via ambulance services, and whether they had been categorized into the predetermined diagnostic categories. In the 1 408 patients 570 patients had received EMS, and were divided into the above categories. Like the CPAP group, the control group was reviewed to determine whether the patients had been intubated after ED admission. For this study intubation criterion was within 72 hours post ED admission. After data collection by a primary investigator, random patient charts from both the control and CPAP groups were rechecked by co-investigators.
Statistical analysis
Given a few outlier elderly patients, the age of the patients did not follow the normal distribution for the given patient sample data, as evidenced by the Shapiro-Wilk test. Further, the data were skewed due to the presence of extremely small values. Therefore, all summaries consisted of median [interquartile range (IQR): 25th–75thpercentiles], and age was compared between the CPAP and control (no CPAP) groups using a nonparametric test, two-sided Wilcoxon's rank-sum test. Categorical responses were presented as frequencies (percentages). Binary responses of the two groups were compared using Fisher's exact test or the Chi-square test.
The risk of intubation was examined using logistic regression analysis after the patients with and without CPAP treatment during EMS were admitted to the ED. Further, multivariable logistic regression analysis was used to adjust the effects that were significant in univariable analysis. The results of the logistic regression analysis were presented as odds ratio (OR), 95% confidence interval (CI) and P value. In order to circumvent the problem of imbalance of the CPAP and control groups, propensity scores were used to adjust the three covariates collected in this study. A propensity score indicated the conditional probability of receiving CPAP, given a set of covariates, i.e. age, gender and diagnosis. In a nonrandomized study like the current retrospective chart review, self-selection bias can be addressed by matching the subjects in each group based on the propensity scores using logistic regression analysis. The rationale for this approach is that subject with equal or nearly equal propensity scores tend to have similar distribution in covariates. This property was validated in the study by examining the distribution of the propensity scores for the CPAP and control groups. The adequacy of the propensity score adjusted multivariable logistic regression analysis was calibrated using Hosmer and Lemeshow's goodnessof-f t test. P<0.05 was considered statistically signif cant. Data analysis was conducted using SAS version 9.2 (SAS Institute Inc., Cary, NC, USA).
RESULTS
Analysis of the data revealed that the diagnostic categories of RF, respiratory failure, RD, and respiratory distress were not equally distributed in the patients. This is likely due to the assignment of diagnostic categories from the pre-set International Classif cation of Diseases (ICD) coding system. Given these assigned diagnoses, there is likely to be overlap noted across the similar categories. However, this skewed distribution was accounted for through the use of propensity scores.
In 330 male patients, 87 (26.4%) were intubated, but in 455 female patients,105 (23.1%) were intubated (P=0.3131). In 396 patients with CHF, 52 (13.1%) were intubated; in 136 COPD patients, 8 (5.9%) were intubated; in 43 patients with RD, 6 (14 %) were intubated; in 3 ARD patients none was intubated; and in 207 patients with RF 126 (60.9%) were intubated. There was a significant difference between diagnoses (P<0.0001). In 215 EMS patients treated with CPAP before hospitalization, 28 (13.0%) were intubated after admission. But in 570 EMS patients treated with CPAP, 164 (28.8%) were intubated after admission to the ED. There was a significant difference in intubation rates between the EMS patients treated with CPAP before hospitalization and those who treated with no CPAP (P<0.0001).
Univariable logistic regression (Table 2) analysis showed that the CPAP-treated patients had a decreased intubation risk of 37% compared with those whodid not have CPAP treatment. Diagnoses also had a signif cant effect on the risk for intubation. The pair wise comparison of the diagnoses showed that CHF, COPD and RD with ORs (0.097, 0.040 and 0.104, respectively) were signif cantly lower than RF. Moreover, patient age was a statistically significant risk factor for intubation. Hosmer and Lemeshow's test showed that diagnosis model was not a good f t although there was a signif cant association (P<0.0001). After the ARD group was removed from the diagnosis, the analysis produced a good fit (P=1.000) by the Hosmer and Lemeshow's test. The ARD group was removed from the logistic regression analysis given since there was very small frequency (n=3 in CPAP group) or 0 frequency in the non-CPAP treatment group. The removal of diagnosis category ensured a model of the other diagnosis categories, which had a good fit and significant association.

Table 2. Logistic regression analysis evaluating risk of intubation in emergency medicine patients treated with CPAP vs. non-CPAP
A multivariable logistic regression analysis (Table 3) using propensity scores to adjust age, sex and diagnosis (CHF, COPD, and RF) demonstrated that the risk of intubation in EMS patients treated with CPAP was reduced more significantly than that in those who were not treated with CPAP (OR=0.383; 95% CI: 0.246 to 0.596) (P<0.001). The propensity scores were stratified into 3 groups, a variable which reported a significant association with the risk of intubation (OR=0.569, 95% CI: 0.459 to 0.704, P<0.0001). The CPAP and non-CPAP treatment groups were balanced with respect to the covariates: age, gender and diagnosis, based on the distribution of propensity scores. The Hosmer and Lemeshow test indicated that this model was a good fit (Chi-square test=8.075, df=4, P=0.0888).
The logistic regression analysis of risk for intubation in this retrospective study demonstrated that there was a correlation between CPAP treatment in EMS before hospitalization and a decreased intubation rate of 62% (OR 0.348, 95% CI: 0.246 to 0.596). Further, propensity scores were used to adjust age, sex and diagnosis, with a reduction of risk for intubation (66%) after CPAP treatment prehospitalization (OR 0.34, 95% CI: 0.199 to 0.593). In addition to a small number of patientswith respiratory distress/acute respiratory distress, the distributions between the CPAP and non-CPAP groups were ill balanced compared with the other diagnosis groups. This may be due to the lack of controls in the selection that is inherent in retrospective studies. This issue was addressed in the present study using propensity scores.

Table 3. Multivariable Logistic regression analysis evaluating risk of intubation in emergency medicine patients treated with CPAP vs. non-CPAP
DISCUSSION
In patients with acute respiratory disorders, a correlation can be observed between the early use of CPAP in EMS before hospitalization and a decreased intubation rate upon admission to the ED. The results of this study showed that CPAP is effective in certain conditions and should be considered as an early intervention for respiratory disorders. No deleterious effects were due to the early CPAP use. These findings are important as they not only highlight the efficacy of CPAP but also the important role the EMS plays in providing this early intervention. Currently, EMS training is limited to acute care of emergencies before availability of hospital resources.
To achieve a broader acceptance of prehospital use of CPAP, initial steps should be taken for paramedic training by trained physicians, leading eventually to the expansion of the EMS scope. The CPAP training is limited to a 2-hour session. In CPAP settings, empirical titration is used to reduce patients discomfort and improve oxygen saturation, and a pressure of 8–10 mmHg is used at the initiation of the treatment. The lack of exposure and training may lead to apprehension of CPAP as a therapeutic tool.
As the demand for ED services has continued to increase, ED crowding and EMS diversion have become a substantial problem.[16]With the crude model of "sustain and transport" used by previous paramedic teams, an answer to the growing ED demand may be given in an alternative model of care at the paramedic level.[22]The development of extended care paramedic (ECP) protocols in conjunction with ALS technique and device advancement as seen in our study may be an effective way for the management of the ED admission issues.
With increasing numbers of paramedic units playing the ECP roles, it is possible to create a multi-site study which would recognize whether the level of success is geographically independent, and allow other institutions to apply CPAP in their emergency service.
In addition to expanding the location and the number of sites, the study can develop further by expanding theoutcome focus. This study was limited in its outcome categories. The researchers primarily focused on identifying intubation rates, as an outcome. However, further development in this aspect may broaden the outlook and the variability in CPAP use. The outcome of future similar studies may see the intubation timeline increased beyond the 3-day limitation, which in turn may provide a better understanding of the long-term post-CPAP effects. With the limited settings extended into a multi-site study, the advanced evidence-based approach would help identify practices that would be expected to improve safety on a national level.[23]
With successful results demonstrating the effectiveness of a basic affordable device on a respiratory disorder and its associated outcomes, it is plausible that further training and application should be indicated in all paramedic/ EMS training in the future. Hopefully, this initiative will improve outcomes in this group of patients.
LIMITATIONS
Based upon two periods in 6 years apart, we reviewed the development of care provided by the paramedic teams. Paramedic interview revealed no substantial changes in training, protocols, and equipment according to the records between the periods, which were recognized as a limitation.
Another limitation was that the variable dependent data were accumulated primarily from the medical center's primary paramedic unit, as opposed to the control data that had been collected from the records consisting of numerous external paramedic teams transporting to the ED. The different service providers could lead to variance in the patient management, with the independent EMS/paramedic clinical approach, and competence possibly playing an important part in the outcome. However, ALS techniques and guidelines are standard training for paramedic teams and would not vary greatly, especially in units within the same region/state. To further prevent any overlapping data, it was ascertained from EMS records that there are no reports of CPAP use in the MICU setting in the extended geographical area of the study before 2006. Paramedic units involved in the study transported both groups of patients directly to the ED, thus limiting possible confounding factors.
Patient information was sometimes limited in paramedic reports. The ambiguity in the records regarding patient's condition, prehospital treatment, or mode of transportation to the ED led to elimination of some data from the study. The removed patients in this study were equally distributed from both CPAP and non-CPAP groups.
ACKNOWLEDGEMENTS
I would like to thank Patricia Knox, Dennis Doody, David Omuwogu, Helen Carter, Kala Maharaj, Cynthia Hassler, Carole Chen, Vladimir Rosario, and Keith Brigley for their contributions to this project.
Funding:No funding provided for this project.
Ethical approval:IRB approval. Consent and HIPAA waiver granted.
Conflicts of interest:The authors have no competing interests relevant to the present study.
Contributors:Knox N, Ashtyani H, Ogedegbe C, and Feldman J concept and designed the study. Knox N, Ashtyani H, Ogedegbe C, and Nyirenda T collected the data. Knox N, Ashtyani H, Ogedegbe C, Feldman J and Nyirenda T analyzed and interpreted the data. Knox N, Ashtyani H, Ogedegbe C, and Nyirenda T drafted the manuscript. Knox N, Ashtyani H, and Ogedegbe C revised the paper.
1 Sullivan C. Inventive pioneer of sleep medicine. Lancet 2011; 377: 1485.
2 Budweiser S, Hitzl AP, Jörres RA, Heinemann F, Arzt M, Schroll S, et al. Impact of noninvasive home ventilation on long-term survival in chronic hypercapnic COPD: a prospective observational study. Int J Clin Pract 2007; 61: 1516–1522.
3 Baydur A, Layne E, Aral H, Krishnareddy N, Topacio R, Frederick G, et al. Long term non-invasive ventilation in the community for patients with musculoskeletal disorders: a 46 year experience and review. Thorax 2000; 55: 4–11.
4 Aboussouan LS, Ricaurte B. Noninvasive positive pressure ventilation: increasing use in acute care. Cleve Clin J Med 2010; 77: 307–316. doi: 10.3949/ccjm.77a.09145.
5 Antro C, Merico F, Urbino R, Gai V. Non-invasive ventilation as a first-line treatment for acute respiratory failure: "real life" experience in the emergency department. Emerg Med J 2005; 22: 772–777.
6 Pendergraft TB, Stanford RH, Beasley R, Stempel DA, Roberts C, Mc Laughlin T. Rates and characteristics of intensive care unit admissions and intubations among asthma related hospitalizations. Ann Allergy Asthma Immunol 2004; 93: 29–35.
7 Brochard L. Mechanical ventilation: invasive versus noninvasive. Eur Respir J Suppl 2003; 47: 31s–37s.
8 Schwartz DE, Matthay MA, Cohen NH. Death and other complications of emergency airway management in critically ill adults: a prospective investigation of 297 tracheal intubations. Anesthesiology 1995; 82: 367–376.
9 Mort TC. Esophageal intubation with indirect clinical tests during emergency tracheal intubation: a report on patient morbidity. J Clin Anesth 2005; 17: 255–262.
10 Mort TC. Complications of emergency tracheal intubation: hemodynamic alterations - Part I. J Intensive Care Med 2007; 22: 157–165.
11 Mort TC. Complications of emergency tracheal intubation: immediate airway-related consequences: Part II. J Intensive Care Med 2007; 22: 208–215.
12 Reynolds SF, Heffner J. Airway management of the critically ill patient: rapid-sequence intubation. Chest 2005; 127: 1397–1412.
13 Bhatti NI, Mohyuddin A, Reaven N, Funk SE, Laeeq K, Pandian V, et al. Cost analysis of intubation-related tracheal injury using a national database. Otolaryngol Head Neck Surg 2010; 143: 31–36.
14 Keenan SP, Sinuff T, Cook DJ, Hill NS. Does noninvasive positive pressure ventilation improve outcome in acute hypoxemic respiratory failure? A systematic review. Crit Care Med 2004; 32: 2516–2523.
15 Squadrone E, Frigerio P, Fogliati C, Gregoretti C, Conti G, Antonelli M, et al. Noninvasive vs. invasive ventilation in COPD patients with severe acute respiratory failure deemed to require ventilatory assistance. Crit Care Med 2004; 32: 2516–2523.
16 Girou E, Schortgen F, Delclaux C, Brun-Buisson C, Blot F, Lefort Y, et al. Association of noninvasive ventilation with nosocomial infections and survival in critically ill patients. JAMA 2000; 284: 2361–2367.
17 Garuti G, Bandiera G, Cattaruzza MS, Gelati L, Osborn JF, Toscani S, et al. Out of hospital helmet CPAP in acute respiratory failure reduces mortality. Monaldi Arch Chest Dis 2010; 73: 145–151.
18 Warner GS. Evaluation of the effect of prehospital application of continuous positive airway pressure therapy in acute respiratory distress. Prehosp Disaster Med 2010; 25: 87–91.
19 Moskop JC, Sklar DP, Geiderman JM, Schears RM, Bookman KJ. Emergency department crowding, part 1—concept, causes, and moral consequences. Ann Emerg Med 2009; 53: 605–611. Epub 2008 Nov 22.
20 Finn JC, Fatovich DM, Arendts G, Mountain D, Tohira H, Williams TA, et al. Evidence-based paramedic models of care to reduce unnecessary emergency department attendance –feasibility and safety. BMC Emerg Med 2013; 13: 13.
21 Hoyle S, Swain AH, Fake P, Larsen PD. Introduction of an extended care paramedic model in New Zealand. Emerg Med Australas 2012; 24: 652–656.
22 Kramer N, Meyer TJ, Meharg J, Cece RD, Hill NS. Randomized, prospective trial of noninvasive positive pressure ventilation in acute respiratory failure. Am J Respir Crit Care Med 1995; 151: 1799–1806.
23 Shojania KG, Duncan BW, McDonald KM, Wachter RM, Markowitz AJ. Making health care safer: a critical analysis of patient safety practices. Evid Rep Technol Assess (Summ) 2001; (43): i–x, 1–668.
Received July 2, 2014
Accepted after revision January 6, 2015
Nigel Knox, Email: nigelknoxny@yahoo.com
World J Emerg Med 2015;6(1):60–66
10.5847/wjem.j.1920–8642.2015.01.011
杂志排行
World journal of emergency medicine的其它文章
- The role of regulatory T cells in immune dysfunction during sepsis
- Instructions for Authors
- Lingual angioedema after alteplase treatment in a patient with acute ischemic stroke
- Regulatory effects of hydrogen sulf de on alveolar epithelial cell endoplasmic reticulum stress in rats with acute lung injury
- Acute intoxication cases admitted to the emergency department of a university hospital
- Trauma patterns in patients attending the Emergency Department of Jazan General Hospital, Saudi Arabia