Prognostic value of CD4+CD25+Tregs as a valuable biomarker for patients with sepsis in ICU
2015-02-07
Emergency Department, Changzheng Hospital, Second Military Medical Univercity, Shanghai 200003, China
Prognostic value of CD4+CD25+Tregs as a valuable biomarker for patients with sepsis in ICU
Kun Chen, Qiu-xiang Zhou, Hong-wei Shan, Wen-fang Li, Zhao-fen Lin
Emergency Department, Changzheng Hospital, Second Military Medical Univercity, Shanghai 200003, China
BACKGROUND:Sepsis is a common complication of infections, burns, traumas, surgeries, poisonings, and post-cardiopulmonary resuscitation. The present study aimed to investigate prognostic value of CD4+CD25+regulatory T cells (Treg) in peripheral blood of patients with sepsis.
METHODS:Periphery blood from 28 patients diagnosed with sepsis was collected on day 1 and 7 after hospitalization in the ICU of Shanghai Changzheng Hospital between December 2013 to April 2014. The blood was used for analyses of Treg ratio using flow cytometry and for analyses of blood routine test, C-reactive protein (CRP), bilirubin, procalcitonin (PCT), and coagulation. APACHE II and sequential organ failure assessment (SOFA) scores were also investigated. The results were compared between two outcome groups of survival or death to evaluate prognostic value for sepsis.
RESULTS:The patients had an average age of 60.36±15.03 years, APACHE II score 16.68±7.00, and SOFA score 7.18±3.78. Among the 28 patients, 12 had severe trauma (42.9%), 10 had septic shock (35.7%), and 9 (32.2%) died. The median ratio of Tregs was 2.10% (0.80%, 3.10%) in the survival group vs. 1.80% (1.15%, 3.65%) in the death group (Z=–0.148,P=0.883) on day 1; however it was signif cantly changed to 0.90% (0.30%, 2.80%) vs. 5.70% (2.60%, 8.30%) (Z=–2.905,P=0.004).
CONCLUSION:With better prospects for clinical application, dynamic monitoring of Tregs ratio in peripheral blood has potential value in predicting prognosis of sepsis.
CD4+CD25+regulatory T cells; Sepsis; Prognosis; Biomarker; APACHE; SOFA; Procalcitonin
INTRODUCTION
Sepsis is a common complication of infections, burns, traumas, surgeries, poisonings, and postcardiopulmonary resuscitation. The incidence rate of sepsis is increasing by 1.5%–8.0% annually and its mortality is as high as 30%–70%.[1,2]
The clinical outcome of sepsis due to infectioninduced systemic excessive inflammatory response is largely dependent on the status of host immune function.[3]During disease progress, sepsis is often accompanied with immune disorders due to dysfunction of T cell subsets including regulatory T cells (Tregs). Tregs as a mature T cell subset play an important role in adaptive immunity to pathogens and autoantigens.[4,5]Activation of Tregs, especially CD4+CD25+Tregs via TCR stimulation can suppress the body's excessive inflammatory response through inhibition of activation and proliferation of effect T cells, and of antibody production by B cells.[6,7]
Many studies on CD4+CD25+Tregs have focused on signal transductions, but few on its application in clinical use. In this study, we investigated the clinical application of CD4+CD25+Tregs in peripheral blood as a potential biomarker in evaluating prognosis of patients with sepsis.
METHODS
Experimental design
Twenty-eight patients with sepsis were observed inShanghai Changzheng Hospital from December 2013 to April 2014. The severity of the patients was evaluated according to the acute physiology and chronic health evaluation II (APACHE II) and sequential organ failure assessment (SOFA) scores. Blood samples from the patients were analyzed by flow cytometry for CD4+CD25+Tregs. Other related indicators were monitored daily and the worst value in a day was used for analysis.
Criteria of patient selection
Based on 2001 Critically Ill Society, European Society of Critical Care, American College of Chest Physicians, American Thoracic Society, and the Surgical Infection Society International Conference on the definition of systemic infection developed standards (ACCP, SCCM2001), we set up the inclusion criteria. Patients were included if two or more the following items met: 1) body temperature higher than 38 °C or lower than 36 °C; 2) heart rate greater than 90 beats/ minute; 3) respiratory rate greater than 30 beats/minute, or PaCO2less than 32 mmHg; 4) WBC in peripheral blood greater than 12×109/L or less than 4.0×109/L, or immature granulocytes more than 10%.
The exclusion criteria for patients included: age younger than 18 years; epilepsy; any autoimmune diseases; long-term use of immunosuppressive agents; active bleeding; acute left ventricular failure caused by pulmonary edema.
Collection of blood sample
Blood samples were collected on day 1 and day 7 after hospitalization and treated with heparin. Lymphocytes were isolated and analyzed by flow cytometry for CD4+CD25+Tregs ratio. Blood was tested for liver and kidney function, blood clotting, electrolytes, PCT, and endotoxins. If repeated tests occurred in the same day, then the worst value was subjected to further analysis. An etiological test was also conducted on the f rst day in the ICU.
Analysis of ratio of Tregs in peripheral blood by f ow cytometry
All blood samples were analyzed within 30 minutes after collection by flow cytometry according to the instructions of FACS Canto (BD Biosciences, USA) detection and BD FACSDiva software.
Statistical analysis
Normal distribution of measurement data uses mean ±SD and independent sample t test was used to compare the survival group and death group.
Non-normal distribution of measurement data was expressed by the median [M (25th, 75th)], and the Mann-Whitney U test and Wilcoxon's nonparametric test were performed between the two groups.
A P value<0.05 was considered statistically signif cant. SPSS19.0 software (SPSS Corp, Chicago, IL, USA) was used for data analysis.
RESULTS
Patient information
In the 28 patients aged 60.36±15.03 years, the average time in ICU was 23.50 (12.25 to 31.75) days. Their APACHE II and SOFA scores on day 1 were 16.68±7.00 and 7.18±3.78 respectively. In this series, 12 (42.9%) patients had severe trauma, 10 (35.7%) had septic shock, and 9 patients (32.2%) died. The major sites of infection of the patients were the lungs (17 patients), bloodstream (10), abdomen (4), urinary tract (3), skin and soft tissue (2), and others (3). Pathogens including gram-negative bacteria and fungi in specimens of body f uids were observed in 22 and 10 patients respecitively (Table 1).
Comparison of general blood tests between the survival and death groups
Blood coagulation reaction D-dimer and endotoxin values on day 7 were statistically higher, and platelets were significant lower in the death group than in the survival group (all P<0.05) (Table 2). Procalcitonin was signif cantlyhigher on day 1 and day 7 in the death group (P<0.05).
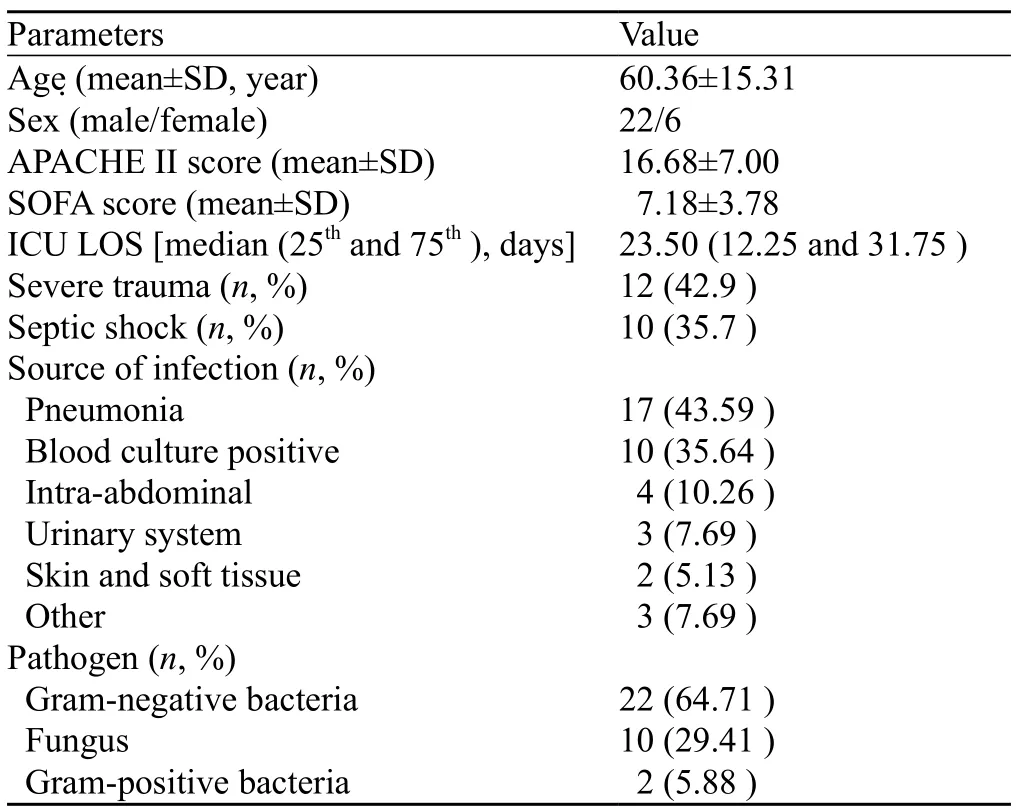
Table 1. The characteristics of patients with sepsis (n=28)
CD4+CD25+Tregs in the survival or death group
The ratios of CD4+CD25+Tregs in peripheral blood on day 1 between the two groups were similar. However, they were significantly changed on day 7 to 0.90% (0.30%, 2.80%) in the survival group vs. 5.70% (2.60%, 8.30%) in the death group (P<0.05). The difference between day 7 and day 1 (Δ_Treg d7–d1) in the two outcome groups was also statistically signif cant (P<0.05) (Table 3).
DISCUSSION
It is important to diagnose and treat sepsis patients as early as possible in order to achieve favorable clinical outcomes.[8]Therefore, it is pivotal to accurately predict prognosis of sepsis patients at different stages and to help optimize treatment options. There are few well-established scoring tools including APACHE II score, improved early warning score (modified early warning score, MEWS), and SOFA score,[9]which have been useful in predicting clinical outcomes. However, it is believed that more effort is needed to f nd predictive biomarkers at earlier stages such as early changes in immune status in sepsis patients, because immune response has been one of the key factors for the pathogenesis of sepsis.[10]In patients with sepsis, immune status is not always in a positive static status,[11]but negative regulation mechanism in the progress of sepsis also plays an important role.[12]As one of the most important peripheral immune cells, CD4+CD25+Treg cells are involved in immune responses in patients with sepsis. The main cause of early death of patients with sepsis is early excessive activation of the immune system to release large amounts of cytokines (cytokine storm) that damage multi-organ systems.[13,14]Later deaths are due to reduced antibody-dependent cell-mediated cytotoxicity (ADCC), immunosuppression, decreased ability to clear pathogens,[5]and increased function of CD4+CD25+Tregs suppressing activation of effect T cells.[11,15]
Our study has shown that the median ratio of CD4+CD25+Tregs in peripheral blood on day 1 between the survival and death groups are comparable with 2.10% (0.80%, 3.10%) vs. 1.80% (1.15%, 3.65%). After a week of treatment in the ICU, the ratio was 0.90% (0.30%, 2.80%) vs. 5.70% (2.60%, 8.30%) (Z=–2.905, P=0.004), with a significantly higher value in the death group than in the survival group. This was supported by the evidence that increased CD4+CD25+Tregs may contribute to the worse outcome by suppressing activation of effect T cells even during the treatment. The difference between the two groups [Δ_Tregs (d7–d1)] was also signif cant, with –0.40% (–1.70%, –0.10%) in the survival group vs. 1.90% (1.55%, 5.10%) in the death group (Z=–3.351, P=0.001). The reason for this phenomenon may be due to various factors such as traumas, infections, and differences in immune activation in patients. The difference in Δ_Tregs (d7–d1) reflected changes in immune function of patients in a week of disease progress and treatment effects. CD4+CD25+Tregs median ratio on day 7 and Δ_Tregs (d7–d1) have indicated their prognostic values as valuable biomarkers in sepsis patients.
In addition, the present study also found that median procalcitonin (PCT) was signif cantly different between the survival and death groups, with 1.84 ng/mL (0.39 ng/mL, 6.28 ng/mL) in the survival group vs. 8.47 ng/mL (5.59 ng/mL, 14.15 ng/mL) (Z=–2.730, P=0.006) on day 1 and 0.74 ng/mL (0.21 ng/mL, 2.00 ng/mL) vs. 8.10 ng/ mL (4.42 ng/mL, 9.27 ng/mL) (Z=–3.424, P=0.001) on day 7. The concept of PCT clearance for assessing the prognosis of sepsis introduces the dynamic change ofPCT that is more meaningful than the absolute value of PCT.[14,16,17]Our study has shown similar results.

Table 2. Comparison of platelet, PCT, endotoxin, D-dimer between the survival and death groups
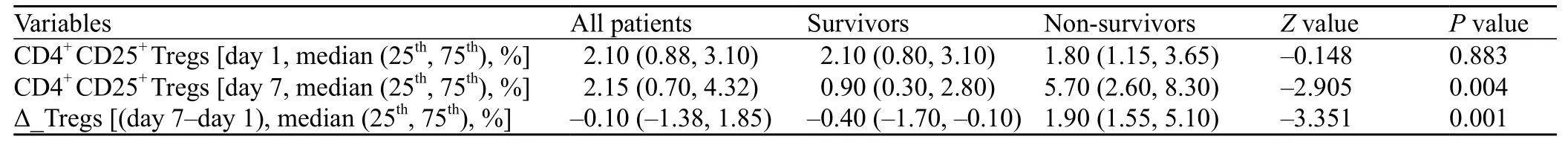
Table 3. Comparison of CD4+CD25+Tregs ratio between the survival and death groups
Analysis of endotoxins showed that median values on day 7 are also significantly different between the two groups as 0.1240 EU/mL (0.0443 EU/mL, 0.2320 EU/ mL) vs. 0.4813 EU/mL (0.2387 EU/mL, 0.7412 EU/mL) (Z=–2.583, P=0.010). The results are consistent with the published literature.[18]Reaction of D-dimer coagulation and platelets between the two groups showed a signif cant difference on day 7, but not day 1, suggesting supplemental values of these indicators for prognosis in sepsis.[19–21]These changes in PCT, endotoxins, D-dimer coagulation and platelets are useful indicators in monitoring progress of sepsis and provide guidance for timely treatment.
Our study incorporated a small number of cases that are admitted to the ICU but not to general wards in a single study center, therefore sepsis patients in this study had APACHE II scores and SOFA scores that were relatively higher. However, further studies with a larger sample size are needed.
In conclusion, The changes in ratio of CD4+CD25+Treg cells in peripheral blood of patients with sepsis are associated with clinical outcomes such as survival or death. CD4+CD25+Treg cells may offer a possible biomarker to be able to accurately assess prognosis of sepsis patients.
Funding:None.
Ethical approval:The ethical approval was obtained from Changzheng Hospital, the Second Militory Medical Univercity, Shanghai, China.
Conf icts of interest:We do not have any conf icts of interest.
Contributors:Chen K, Zhou QX and Shan HW contributed equally to this article. Shan HW and Lin ZF designed the trial and collected the data. Chen K and Zhou QX analyzed the data and drafted the manuscript. Chen K, Zhou QX and Li WF collected the data and revise the article.
1 Jones BL, Smith SM. Choice of crystalloid and mortality in sepsis—all in the timing? Crit Care Med 2014; 42: e796.
2 Barochia AV, Cui X, Eichacker PQ. The surviving sepsis campaign's revised sepsis bundles. Curr Infect Dis Rep 2013; 15: 385–393.
3 Chen XH, Yin YJ, Zhang JX. Sepsis and immune response. World J Emerg Med 2011; 2: 88–92.
4 Leng FY, Liu JL, Liu ZJ, Yin JY, Qu HP. Increased proportion of CD4(+)CD25(+)Foxp3(+) regulatory T cells during early-stage sepsis in ICU patients. J Microbiol Immunol Infect 2013; 46: 338–344.
5 Kuhlhorn F, Rath M, Schmoeckel K, Cziupka K, Nguyen HH, Hildebrandt P, et al. Foxp3+regulatory T cells are required for recovery from severe sepsis. PloS One 2013; 8: e65109.
6 Almansa R, Wain J, Tamayo E, Andaluz-Ojeda D, Martin-Loeches I, Ramirez P, et al. Immunological monitoring to prevent and treat sepsis. Crit Care 2013; 17: 109.
7 Zahran AM, Elsayh KI. CD4+CD25+High Foxp3+regulatory T cells, B lymphocytes, and T lymphocytes in patients with acute ITP in Assiut Children Hospital. Clin Appl Thromb Hemost 2014; 20: 61–67.
8 Geier F, Popp S, Greve Y, Achterberg A, Glockner E, Ziegler R, et al. Severity illness scoring systems for early identif cation and prediction of in-hospital mortality in patients with suspected sepsis presenting to the emergency department. Wien Klin Wochenschr 2013; 125: 508–515.
9 Macdonald SP, Arendts G, Fatovich DM, Brown SG. Comparison of PIRO, SOFA, and MEDS scores for predicting mortality in emergency department patients with severe sepsis and septic shock. Acad Emerg Med 2014; 21: 1257–1263.
10 Wang H, Wei Y, Zeng Y, Qin Y, Xiong B, Qin G, et al. The association of polymorphisms of TLR4 and CD14 genes with susceptibility to sepsis in a Chinese Population. BMC Med Genet 2014; 15: 123.
11 Liu QY, Yao YM. Inf ammatory response and immune regulation of high mobility group box-1 protein in treatment of sepsis. World J Emerg Med 2010; 1: 93–98.
12 Luan YY, Yao YM, Sheng ZY. Update on the immunological pathway of negative regulation in acute insults and sepsis. J Interferon Cytokine Res 2012; 32: 288–298.
13 Gentile LF, Moldawer LL. HMGB1 as a therapeutic target for sepsis: it's all in the timing! Expert Opin Ther Targets 2014; 18: 243–245.
14 Huber-Lang M, Barratt-Due A, Pischke SE, Sandanger O, Nilsson PH, Nunn MA, et al. Double blockade of CD14 and complement C5 abolishes the cytokine storm and improves morbidity and survival in polymicrobial sepsis in mice. J Immunol 2014; 192: 5324–5331.
15 Chang RM, Wen LQ, Chang JX, Fu YR, Jiang ZP, Chen S. Repair of damaged intestinal mucosa in a mouse model of sepsis. World J Emerg Med 2013; 4: 223–228.
16 Verma N, Kapoor S, Rao D, Sharma S, Arora A. PCT as a prognostic marker in cardiac patients with neutropenic sepsis: two case reports. Indian J Clin Biochem 2014; 29: 107–111.
17 Tamura M, Watanabe M, Nakajima A, Kurai D, Ishii H, Takata S, et al. Serial quantif cation of procalcitonin (PCT) predicts clinical outcome and prognosis in patients with community-acquired pneumonia (CAP). J Infect Chemother 2014; 20: 97–103.
18 Zu H, Li Q, Huang P. Expression of treg subsets on intestinal T cell immunity and endotoxin translocation in porcine sepsis after severe burns. Cell Biochem Biophys 2014; 70: 1699–1704.
19 Ding H, Cao XY, Ma XG, Zhou WJ.Endothelial cell injury with inflammatory cytokine and coagulation in patients with sepsis. World J Emerg Med 2013; 4: 285–289.
20 Varol E. Platelet volume evaluation in patients with sepsis: associated factors should be considered. Afr Health Sci 2014;14: 492–493.
21 McLaughlin J, Ramachandran R, Kaynar A, Shapiro S, Angus D, Malik A. Regulation of endothelial function by coagulation proteases in sepsis. Crit Care 2011; 15: P251.
Received September 15, 2014
Accepted after revision January 10, 2015
Zhao-fen Lin, Email: linzhaofen@sina.com
World J Emerg Med 2015;6(1):40–43
10.5847/wjem.j.1920–8642.2015.01.007
杂志排行
World journal of emergency medicine的其它文章
- Evaluation of a simulation-based workshop on clinical performance for emergency physicians and nurses
- Ultrasound diagnosis of malaria: examination of the spleen, liver, and optic nerve sheath diameter
- Embryonic natural orif ce transluminal endoscopic surgery in the treatment of severe acute pancreatitis complicated by abdominal compartment syndrome
- Effect of low-dose glucocorticoid on corticosteroid insuff cient patients with acute exacerbation of chronic obstructive pulmonary disease
- Effect of harmless acute pancreatitis score, red cell distribution width and neutrophil/lymphocyte ratio on the mortality of patients with nontraumatic acute pancreatitis at the emergency department
- The risk of wound infection after simple hand laceration
