Natural history of sensory nerve recovery after cutaneous nerve injury following foot and ankle surgery
2015-01-18LuBaiYanniHanWentaoZhangWeiHuangHongleiZhang
Lu Bai, Yan-ni Han, Wen-tao Zhang,*, Wei Huang, Hong-lei Zhang
1 Department of Sports Medicine, Shenzhen Hospital of Peking University, Shenzhen, Guangdong Province, China
2 Department of Medical Ultrasonics, Shenzhen Hospital of Peking University, Shenzhen, Guangdong Province, China
Natural history of sensory nerve recovery after cutaneous nerve injury following foot and ankle surgery
Lu Bai1, Yan-ni Han2, Wen-tao Zhang1,*, Wei Huang1, Hong-lei Zhang1
1 Department of Sports Medicine, Shenzhen Hospital of Peking University, Shenzhen, Guangdong Province, China
2 Department of Medical Ultrasonics, Shenzhen Hospital of Peking University, Shenzhen, Guangdong Province, China
Cutaneous nerve injury is the most common complication following foot and ankle surgery. However, clinical studies including long-term follow-up data after cutaneous nerve injury of the foot and ankle are lacking. In the current retrospective study, we analyzed the clinical data of 279 patients who underwent foot and ankle surgery. Subjects who suffered from apparent paresthesia in the cutaneous sensory nerve area after surgery were included in the study. Patients received oral vitamin B12and methylcobalamin. We examined fnal follow-up data of 17 patients, including seven with sural nerve injury, fve with superfcial peroneal nerve injury, and fve with plantar medial cutaneous nerve injury. We assessed nerve sensory function using the Medical Research Council Scale. Follow-up immediately, at 6 weeks, 3, 6 and 9 months, and 1 year after surgery demonstrated that sensory function was gradually restored in most patients within 6 months. However, recovery was slow at 9 months. There was no signifcant difference in sensory function between 9 months and 1 year after surgery. Painful neuromas occurred in four patients at 9 months to 1 year. The results demonstrated that the recovery of sensory function in patients with various cutaneous nerve injuries after foot and ankle surgery required at least 6 months.
nerve regeneration; natural history; cutaneous nerve injury; foot and ankle; sural nerve; superficial peroneal nerve; medial plantar nerve; neurosensory function; neural regeneration
Bai L, Han YN, Zhang WT, Huang W, Zhang HL (2015) Natural history of sensory nerve recovery after cutaneous nerve injury following foot and ankle surgery. Neural Regen Res 10(1):99-103.
Introduction
The foot and ankle have little soft-tissue coverage and abundant innervation. Cutaneous nerve injury is the most common complication of foot and ankle surgery (McMahon et al., 2011; Mercer et al., 2011; Hughes et al., 2014). However, the treatment and follow-up of foot and ankle problems in clinical practice have tended to concentrate on the original disease or injury (e.g., fractures and deformities), and the clinical treatment and recovery of cutaneous nerve injuries around the foot and ankle have been largely ignored. Cutaneous nerve injuries may thus result in local sensory abnormalities and the development of painful neuromas, associated with problems with wearing shoes or walking (Solomon, et al., 2001; Takao et al., 2001; Shim et al., 2014). Furthermore, abnormal sensation and neuroma formation may affect the patient’s quality of life and lead to an unsatisfactory outcome. However, no long-term observational and follow-up studies have investigated these issues, and the question of whether cutaneous nerve injuries recover completely over time, or if loss of sensation persists remains unanswered.
We conducted a 1-year follow-up, observational study in patients with cutaneous nerve injury caused by ankle surgery, to establish the pattern of recovery after cutaneous nerve injury of the ankle.
Subjects and Methods
Subjects
A total of 279 patients underwent angle surgery from August 2012 to July 2013. We assessed patients with local sensory disorders after surgery. Twenty-three patients were diagnosed with cutaneous nerve injury of the ankle and data were fnally obtained for 17 patients, including 13 men and 4 women, with an average age of 33.6 (25-61) years. These included seven cases with sural nerve injury, fve with superfcial peroneal nerve injury, and fve with medial plantar nerve injury.
Among the above patients with cutaneous nerve injury, 10 patients underwent open surgery and seven underwent minimally-invasive or arthroscopic surgery. Patient characteristics and details of their surgical treatment and cutaneous nerve injury are shown inTable 1.
Postoperative treatment
Patients with signifcant abnormal sensation in the cutaneous nerve region after surgery were diagnosed with cutaneous nerve injury.
Following a defnite diagnosis, patients received oral vitamin B12(Yuxing Biopharmaceutical Factory, Xingtai, Hebei Province, China) 2 µg, twice a day, and oral methylcobalamin (Weicai China Pharmaceutical Factory, Suzhou, JiangsuProvince, China) 0.5 mg, once a day, for 1 month.
Follow-up procedure
The Medical Research Council Scale was used to assess nerve sensory function in consecutive follow-up observations of patients immediately after surgery (Seddon, 1975), and at 6 weeks, 3, 6, and 9 months, and 1 year after surgery. All observations were completed by the same group of doctors. Hot and cold sensations were tested using two test tubes flled with hot and cold water, respectively. Discrimination between two points was tested using static two-point discrimination (S2PD) and movable two-point discrimination (M2PD) tests (Seddon, 1975). In this test, patients were asked to close their eyes and the needle tip of the tester was used to determine the extent of the sensory disorder. Both needle tips should contact the patient’s skin at the same time. The distance between the two needle tips was increased and the patient was asked if they could detect one or two points. If the patient could detect two individual points, the distance between them was reduced until the patient detected them as a single point. The Medical Research Council Scale was adopted to evaluate the patient’s nerve function, which was classifed into six levels from S0 to S4: S0, loss of single sensory innervation zone; S1, recovery of deep single sensory innervation zone; S2, certain recovery of pain and touch senses in the single superficial sensory innervation zone; S3, recovery of pain and touch senses in the single superficial sensory innervation zone and disappearance of hypersensitivity, S2PD (mm) > 15, M2PD (mm) > 8; S3+, feeling further recovered on the basis of S3 S2PD (mm) 6-15, M2PD (mm) 4-8; and S4, complete recovery S2PD (mm) 2-3, M2PD (mm) 2-5.
Neuroma detection
Patients with pain in the sensory-defect zone or local incision after surgery underwent ultrasound tests (Philips HD7XE, Amsterdam, Netherlands), conducted by the same doctor.
Statistical analysis
Statistical analysis was conducted using PASW 18.0 statistical software (SPSS, Chicago, IL, USA). All numerical data are summarized as the mean ± SD. Sensory nerve function was graded as numeration data and neurological recoveries at different follow-up observation periods and in different nerves were compared using rank sum tests (Wilcoxon’s test). The recovery of neurological function in relation to time was analyzed by Kaplan-Meier curves and chi-square tests. A value of P < 0.05 was considered statistically signifcant.
Results
One-year follow-up data in patients with cutaneous nerve injury after foot and ankle surgery
The Medical Research Council Scale was used to evaluate the recovery of sensory function in patients who had undergone surgery, after 6 weeks, 3, 6 and 9 months, and 1 year (Table 2). At 6 weeks after surgery, most sural nerves had only recovered to S2 level, while sensory function had almost returned to normal in a few patients with superfcial peroneal nerve and saphenous nerve injuries. Sural nerve sensation began to recover at 3 months after surgery, but there were no cases of complete recovery of sural nerve sensation. However, superfcial peroneal nerve function had returned to normal in a few cases, and saphenous nerve sensation had recovered to normal or close to normal levels in most cases. Hyperalgesia had started to disappear by 6 weeks after surgery in most patients, and had largely disappeared at 3 months after surgery, except in patients with painful neuromas.
All the involved nerves eventually healed, but recovery was slower after 9 months. There was no significant difference in Medical Research Council Scale between 9 months and 1 year (Z = −0.919, P = 0.358) (Table 3).
There were no signifcant differences among the different nerve-injury groups in terms of nerve recovery (Table 4). However, while residual sensation had recovered well in patients with saphenous and superfcial peroneal nerve injuries at 6 months after surgery, some patients with sural nerve injury still experienced some loss of function, with painful neuromas, palpable subcutaneous induration, and distinct local radiation discomfort and pain. By 9 months and 1 year after surgery, neurological function was significantly recovered compared with immediately after surgery; sensory function had returned to almost normal in most patients with saphenous and superfcial peroneal nerve injuries, but recovery of sural sensory nerve function was unsatisfactory in one patient. Two patients with painful neuromas experienced numbness and radiation-like pain. One patient with superficial peroneal nerve injury and one patient with saphenous nerve injury suffered from neuromas, which could be removed by surgery.
Recovery sensory function in patients with cutaneous nerve injury after foot and ankle surgery
Nerve function gradually recovered over time, as demonstrated by Kaplan-Meier analysis. Three months after surgery appeared to be an important time point. There were no significant differences between different nerve-injury groups (χ2= 1.123, P = 0.571) (Figure 1), and the curves for superfcial peroneal nerve and saphenous nerve recovery overlapped and showed similar variation trends.
Discussion
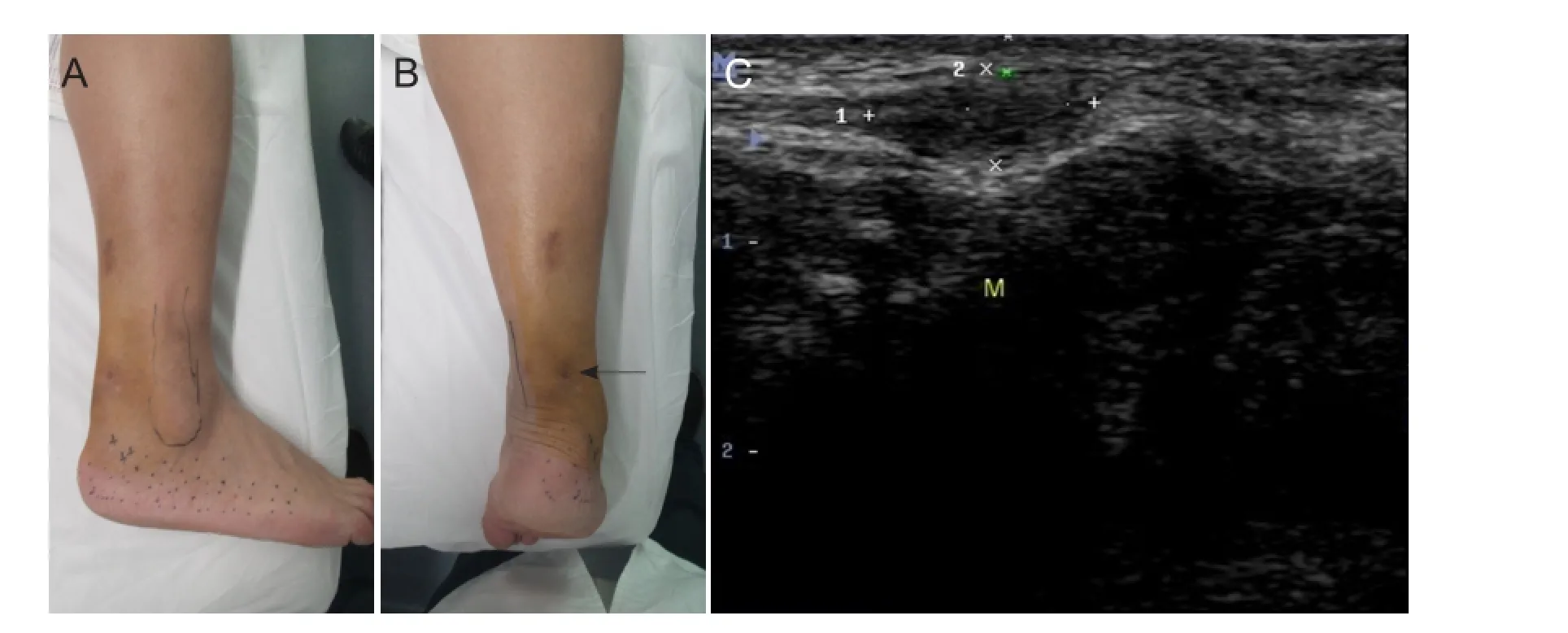
Figure 2 A 46-year-old male patient undergoing percutaneous tendon suture surgery after right tendon fracture.

Figure 1 Kaplan-Meier curves for patients with different nerve injuries during 1-year follow-up.
Cutaneous nerve injury is common after ankle surgery as a result of incision, contusion, or entrapment caused by suture ligation (Solomon et al., 2001; O’Neill et al., 2007; McMahon et al., 2011; Hughes et al., 2014). Local, painful neuromas may develop in some cases (Shim et al., 2014). There are two reasons for these complications. Firstly, the surgical incision may include the distribution area of the cutaneous nerve. Redfern et al. (2003) studied 56 patients who underwent open reduction and internal fixation and 64 who received conservative treatment with plaster fxation for ankle joint fractures. Over a 2-year follow-up period, 15% cases were affected by symptoms of superficial peroneal nerve injury, such as local pain. Using a posterolateral surgical approach to the ankle was an effective technique for protecting the superfcial peroneal nerve (Redfern et al., 2003). Furthermore, anatomical studies demonstrated that the superficial peroneal nerve may often be injured during open reduction and internal fxation of the lateral malleolus in open reduction procedures. For instance, in the case of type B superficial peroneal nerves, according to the Blair & Botte classifcation, the dorsal nerve branch passes obliquely through the lateral malleolus (Halm and Schepers 2012). This presents a risk of superfcial peroneal nerve injury when adopting a lateral approach for lateral malleolus fracture fxation. In relation to the approach for ankle arthroscopy surgery, the anteromedial approach may damage the superfcial peroneal nerve and risk damaging the dorsalis pedis branch of the saphenous nerve (Takao et al., 2001; Ucerler et al., 2007; Hughes et al., 2014). However, sural nerve injury is more common in closed percutaneous Achilles tendon suture surgery; while the sutures pass through both sides of the tendon, the stitches or puncture may involve the sural nerve (McMahon et al., 2011). Shim et al. (2014) verifed that the symptoms could not be relieved by conservative treatment, and surgical removal was necessary in patients with painful neuroma of the medial dorsal cutaneous nerve. In the current study, we observed no improvement following conservative treatment in four patients (two cases of sural nerve injury, one case of superfcial peroneal nerve injury and one case of saphenous nerve injury). The cutaneous nerve pathway around the ankle is superficial and neuromas may form relatively easily. These lead to signifcant symptoms that are diffcult to relieve by conservative therapy, and surgical treatment is therefore recommended (Figure 2).
Cutaneous nerve injury of the ankle has been reported as a complication of foot and ankle surgery in many clinical papers. However, observations of neurologic function after the injury are often neglected in favor of clinical observations of the primary problem (e.g., fracture or deformity correction). Previous studies on the treatment of peripheral nerve injuries have tended to concentrate on the recovery and restoration of function after motor nerve injury, while the natural history and observational follow-up of cutaneous nerve injuries are often neglected. Previous follow-up observations of cutaneous nerve injury of the ankle have included observations of donor-site injuries after sural nerve grafting. Abnormal sensation at the donor site disappeared by 3 months after transplantation, with residual sensation disorder in the middle of the dorsalis pedis and the front side of the ankle (Buntic et al., 2002). Gideroglu et al. (2005) conducted a 1-year follow-up observation of sensation recovery after saphenous nerve flap surgery, and concluded that although sensation recovered in all patients, it only recovered to the same level as the uninjured side in three cases (3/14). This suggests that not only is the recovery period for cutaneous nerve injury of the ankle long, but that a lack of sensation may persist. In the current study, patients in all
groups experienced abnormal sensation in the cutaneous nerve innervation region for at least 6 weeks, after which, hyperpathia appeared during the recovery of sensory function. The duration of saphenous nerve hyperpathia was short (no longer than 1 month), but that of the sural nerve was relatively long (at least 2 months). After 3 months, the sensation disorders were gradually relieved, and returned to normal in some cases. Among the three nerve-injury groups, sural nerve recovery was slowest, with the presence of painful neuromas in its innervation zone. However, sensation in the above cutaneous nerve injury region gradually recovered to normal by 6 months to 1 year after surgery. This differs from the situation following complete nerve transection injury or harvesting of the cutaneous nerve for transplantation, because the injury may only be caused by excessive traction or contusion, allowing complete recovery in some cases. In the case of motor nerve injury, recovery is closely related to the distance between the nerve injury and the target organ (dominant muscle). Based on axonal regeneration, sensory nerves may be expected to follow a corresponding regeneration law. However, clinical follow-up observations have confrmed that recovery after cutaneous nerve injury in the ankle usually starts at 4-6 weeks, and complete recovery usually requires 6 months or longer.

Table 1 Clinical data for patients with cutaneous nerve injuries
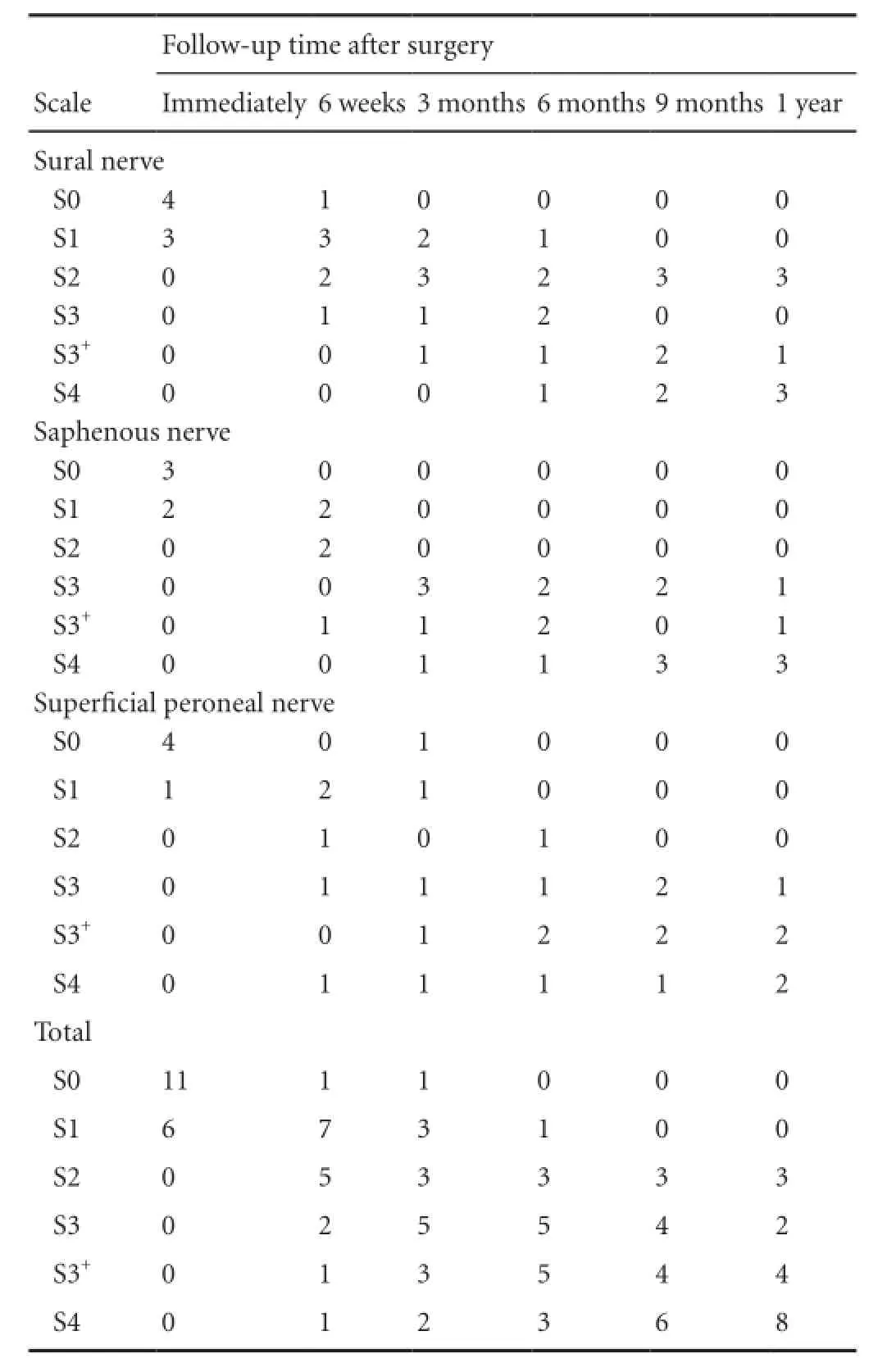
Table 2 Medical Research Council Scale ratings for patients (n) with different types of nerve injury at different follow-up time

Table 3 Nerve recovery at different follow-up times (Wilcoxon's test)

Table 4 Nerve recovery in different nerve-injury groups (Wilcoxon' stest)
According to the Kaplan-Meier curves, complete recovery after cutaneous nerve injury usually took from 6-9 months. Comparison of the superficial peroneal, sural, and saphenous nerves suggested that recovery was fastest in the superfcial peroneal nerve, possibly because of the promoting effects of the ramus communicans and the nerve distribution region. According to anatomical studies, the rami communicantes of the sural nerve and superfcial peroneal nerve are abundant in the anterolateral part of the dorsalis pedis and metapedes (Nagabhooshana et al., 2009). Drizenko et al. (2004) demonstrated that 58% of rami communicantes were located approximately 4-5 cm from the lateral malleolus in 55 cases. Some recent anatomical studies have shown that the superfcial peroneal nerve often has a deep branch that may play a role in restoring sensation in the foot (Tzika et al., 2012). Nevertheless, rami communicantes also exist among different trunks of the cutaneous nerve, resulting in different clinical presentations after cutaneous nerve injury of the ankle.
This study has two main limitations. Firstly, we did not relate the cutaneous nerve injury in the ankle to a functional evaluation of the ankle, mainly because of differences in the patients’ original diseases and injuries, and in surgical treatments. Secondly, in patients with painful neuromas, surgical removal was performed 1 year after the original surgery, and further follow-up observations were required to assess the recovery of neurological function after surgery.
Author contributions:LB and WTZ designed the study. LB, YNH, and WH performed experiments. HLZ analyzed the data. LB wrote the paper. All authors approved the final version of the paper.
Conficts of interest:None declared.
Buntic RF, Buncke HJ, Kind GM, Chin BT, Ruebeck D, Buncke GM (2002) The harvest and clinical application of the superfcial peroneal sensory nerve for grafting motor and sensory nerve defects. Plast Reconstr Surg 109:145-151.
Drizenko A, Demondion X, Luyckx F, Mestdagh H, Cassagnaud X (2004) The communicating branches between the sural and superficial peroneal nerves in the foot: a review of 55 cases. Surg Radiol Anat 26:447-452.
Gideroglu K, Gunduz O, Ofuoglu D, Akoz T (2005) Sensorial donor site morbidity after saphenous neurocutaneous flap. Scand J Plast Reconstr Surg Hand Surg 39:302-307.
Halm J, Schepers T (2012) Damage to the superficial peroneal nerve in operative treatment of fbula fractures: straight to the bone? Case report and review of the literature. J Foot Ankle Surg 51:684-686.
Hughes AM, Gosling O, McKenzie J, Amirfeyz R, Winson IG (2014) Arthroscopic triple fusion joint preparation using two lateral portals: a cadaveric study to evaluate efficacy and safety. Foot Ankle Surg 20:135-139.
McMahon SE, Smith TO, Hing CB, Smith B (2011) A meta-analysis of randomised controlled trials comparing conventional to minimally invasive approaches for repair of an achilles tendon rupture. Foot Ankle Surg 17:211-217.
Mercer D, Morrell NT, Fitzpatrick J, Silva S, Child Z, Miller R, DeCoster TA (2011) The course of the distal saphenous nerve: a cadaveric investigation and clinical implications. Iowa Orthop J 31:231-235.
Nagabhooshana S, Vollala VR, Rodrigues V, Rao M (2009) Anomalous superfcial peroneal nerve and variant cutaneous innervation of the sural nerve on the dorsum of the foot: a case report. Cases J 2:197.
O’Neill PJ, Parks BG, Walsh R, Simmons LM, Miller SD (2007) Excursion and strain of the superficial peroneal nerve during inversion ankle sprain. J Bone Joint Surg Am 89:979-986.
Redfern DJ, Sauve PS, Sakellariou A (2003) Investigation of incidence of superficial peroneal nerve injury following ankle fracture. Foot Ankle Int 24:771-774.
Seddon H (1975) Results of repair of the nerves. Edinburgh: Churchill Livingstone, UK.
Shim JS, Lee JH, Han SH, Kim M, Lee HJ, Min K (2014) Neuroma of medial dorsal cutaneous nerve of superfcial peroneal nerve after ankle arthroscopy. PM R 6:849-852.
Solomon LB, Ferris L, Tedman R, Henneberg M (2001) Surgical anatomy of the sural and superfcial fbular nerves with an emphasis on the approach to the lateral malleolus. J Anat 199:717-723.
Takao M, Ochi M, Shu N, Uchio Y, Naito K, Tobita M, Matsusaki M, Kawasaki K (2001) A case of superfcial peroneal nerve injury during ankle arthroscopy. Arthroscopy 17:403-404.
Tzika M, Paraskevas GK, Kitsoulis P (2012). The accessory deep peroneal nerve: a review of the literature. Foot (Edinb) 22:232-234.
Ucerler H, kiz AA, Uygur M (2007) A cadaver study on preserving peroneal nerves during ankle arthroscopy. Foot Ankle Int 28:1172-1178.
Copyedited by Furness S, Wysong S, Wang J, Qiu Y, Li CH, Song LP, Zhao M
*Correspondence to: Wen-tao Zhang, M.D., zhangwt2007@sina.cn.
10.4103/1673-5374.150713
http://www.nrronline.org/
Accepted: 2014-12-27
杂志排行
中国神经再生研究(英文版)的其它文章
- Neural Regeneration Research (NRR) Instructions for Authors (2015)
- Hypersensitivity of vascular alpha-adrenoceptor responsiveness: a possible inducer of pain in neuropathic states
- Neural regeneration after peripheral nerve injury repair is a system remodelling process of interaction between nerves and terminal effector
- Acute carbon monoxide poisoning and delayed neurological sequelae: a potential neuroprotection bundle therapy
- Prediabetes and type 2 diabetes implication in central proliferation and neurogenesis
- Clinical strategies to enhance nerve regeneration