ERCC1和Ki67表达与乳腺癌患者含铂类化疗方案敏感性的关系
2015-01-05魏昕杨举伦
魏昕,杨举伦
(1.遵义医药高等专科学校病理教研室,遵义 563000;2.成都军区昆明总医院病理科,昆明 650000)
·药物与临床·
ERCC1和Ki67表达与乳腺癌患者含铂类化疗方案敏感性的关系
魏昕1,杨举伦2
(1.遵义医药高等专科学校病理教研室,遵义 563000;2.成都军区昆明总医院病理科,昆明 650000)
目的 探讨核苷酸切除修复交叉互补基因1(ERCC1)和Ki67的表达与乳腺癌患者含铂类化学治疗(化疗)方案敏感性的关系。方法 经病理学确诊乳腺癌患者129例,均行紫杉醇和卡铂联合化疗方案。吉西他滨1 000 mg·(m2)-1,静脉滴注30 min,第1,8天;顺铂25 mg·(m2)-1,静脉滴注,第1~3天;21 d为1个周期,化疗6个周期。采用免疫组化分析患者肿瘤组织中ERCC1和Ki67的表达,并比较ERCC1和Ki67不同表达水平的患者对铂类化疗方案的敏感性和对铂类方案化疗患者生存的影响。结果 129例患者中,ERCC1-Ki67-患者18例,临床有效率88.89%,3年累积生存率83.33%;ERCC1+Ki67-患者24例,临床有效率50.00%,3年累积生存率62.50%;ERCC1-Ki67+患者33例,临床有效率54.55%,3年累积生存率60.60%;ERCC1+Ki67+54例,临床有效率22.78%,3年累积生存率31.48%。与ERCC1-Ki67-组比较,ERCC1+Ki67-组、ERCC1-Ki67+组和ERCC1+Ki67+组患者对顺铂为基础的化疗方案的临床有效率明显下降(P<0.05)。ERCC1+Ki67+组较ERCC1+Ki67-组和ERCC1-Ki67+组也显著下降(P<0.05)。与ERCC1+Ki67-组和ERCC1-Ki67+组比较,ERCC1+Ki67+组患者3年累积生存率明显下降(P<0.05),而ERCC1+Ki67-组和ERCC1-Ki67+组比较差异无统计学意义(P>0.05)。ERCC1+Ki67-组和ERCC1-Ki67+组患者3年累积生存率明显低于ERCC1-Ki67-组(P<0.05)。结论 ERCC1和Ki67在乳腺癌组织中表达水平较高,与患者铂类化疗药物的临床有效率密切相关。
化学治疗药物;癌,乳腺;切除修复交叉互补基因1(ERCC1);Ki67;化学治疗敏感性
乳腺癌是临床常见的肿瘤,也是严重威胁女性健康的恶性肿瘤之一[1]。化学治疗(化疗)仍然是治疗乳腺癌的主要手段之一,但是在临床实践中发现,部分患者对化疗药物不敏感,严重影响临床治疗效果[2-3]。化疗耐药相关的基因是目前关注的焦点和热点。其中核苷酸切除修复交叉互补基因1(Excision repair cross complementation group 1,ERCC1)是核苷酸修复过程中关键的基因,其在维持核苷酸修复中发挥重要作用,但是其过表达能使化疗药物损伤的脱氧核糖核苷酸迅速修复,进而达不到抑制肿瘤细胞生长的作用[4-5]。Ki67是一种细胞基质内抗原,其可直接反映肿瘤细胞的增殖状况[6-7]。目前研究显示,ERCC1和Ki67与鼻咽癌、非小细胞肺癌、卵巢癌以及结直肠癌的化疗耐药性有关[8-10]。关于两者基因在乳腺癌组织中的表达情况以及与患者铂类药物的化疗敏感性、生存率之间的关系,笔者尚未见报道。本研究以ERCC1和Ki67蛋白的表达情况进行正交分组,探讨不同表达水平蛋白对患者化疗耐药和生存的影响。
1 资料与方法
1.1 临床资料 以成都军区昆明总医院2008年6月—2012年6月收治的初治三阴性乳腺癌患者129例为研究对象。所有患者均经体格检查、B超、CT、MRI和局部病理学检查确诊,并且满足下述条件:①所有患者均为初治,且雌激素受体(ER)、孕激素受体(PR)和HER-2均为阴性;②就诊时患者预期生存时间均>4个月;③Karnofsky评分(KPS)>60分;④患者就诊时未见转移病灶;⑤患者实验室指标正常,能够耐受化疗。129例患者年龄30~70岁,平均(58.8±9.8)岁;未婚19例,已婚110例;根据AJCC乳腺癌cTNM分期:Ⅱ期101例,Ⅲ期28例。病理分型:小叶癌58例,导管癌51例,其他类型20例;组织学分级(Elston and Ellis分级法):Ⅰ级19例,Ⅱ级63例,Ⅲ级47例。
1.2 化疗方案 所有患者术后均行紫杉醇和卡铂联合化疗方案。吉西他滨(江苏豪森药业股份有限公司,批准文号:国药准字H20030104)1 000 mg·(m2)-1,静脉滴注30 min,第1,8天;顺铂(扬子江药业,批准文号:国药准字H20053001)25 mg·(m2)-1,静脉滴注,第1~3天;21 d为一个周期,化疗6个周期。患者在治疗期间给予常规托烷司琼止吐。
1.3 实验材料 肿瘤标本来自于手术切除肿瘤组织。ERCC1和Ki67鼠单克隆抗体购自美国Abcam公司,羊抗鼠二抗购自北京金桥中杉生物有限公司;其他化学试剂均为国产分析纯,购自国药集团。
1.4 免疫组化方法 石蜡包埋的标本组织连续切成薄片5 μm,粘附于多聚赖氨酸处理的玻片上,然后在50 ℃烘箱中烤1 h,然后依次用二甲苯及100%,95%,80%和75%乙醇水化,纯化水洗涤3次。将玻片置于含柠檬酸钠的缓冲液中,加热处理8 min,重复2次,磷酸盐缓冲液(phosphate buffered solution,PBS)洗涤3次;在玻片组织部位滴加3%过氧化氢(75%甲醇配制)处理30 min去除内源性的过氧化氢酶。PBS洗涤3次,每次5 min。将稀释的ERCC1和Ki67一抗按照比例稀释,滴加到玻片组织上,4 ℃ 孵育过夜,次日PBS洗涤玻片3次,每次5 min;然后在玻片上滴加10%山羊血清稀释的羊抗鼠的二抗,室温孵育1 h后,用PBS洗涤3次,每次5 min。然后在玻片上滴加二氨基联苯胺(diaminobenzidine,DAB)显色液50 μL,边染色边在显微镜下观察,染色结束后用自来水冲洗,并依次在70%,80%,90%和100%乙醇中脱水,在二甲苯中脱水干燥,并用中性树脂固定,在显微镜下进行固定。
1.5 观察指标和评定标准 分别对患者乳腺癌组织中ERCC1和Ki67的表达水平进行分析,并根据ERCC1和Ki67的阳性或阴性分析其对吉西他滨联合顺铂化疗方案的临床治疗有效率,以及对患者生存率的影响。ERCC1和Ki67评定标准采用分级评分原则,即每张切片在400倍显微镜下随机选取10个视野,计算每个视野中100个细胞中阳性细胞的比例,取其平均值作为ERCC1和Ki67阳性细胞的比例。如阳性细胞比例<10%视为阴性,阳性细胞比例>10%视为阳性[11]。临床有效率采用世界卫生组织制定的关于实体瘤疗效评定标准进行评定,分为完全缓解、部分缓解、稳定和进展。临床有效率(%)=(完全缓解+部分缓解)/总例数×100%。

2 结果
2.1 ERCC1和Ki67表达情况分析结果 见图1所示,ERCC1和Ki67蛋白均表达于细胞核中,呈棕色颗粒形状。129例患者中,ERCC1阴性患者51例,阳性患者78例;Ki67阴性患者42例,阳性患者87例。根据ERCC1和Ki67蛋白表达情况,将患者分为4组:ERCC1-Ki67-双阴性患者18例,ERCC1+Ki67-单阳性患者24例,ERCC1-Ki67+单阳性患者33例,ERCC1+Ki67+双阳性患者54例。4组患者一般资料见表1,患者年龄、TNM分型、病理分型和组织学分级等指标比较差异无统计学意义(P>0.05),具有可比性。
2.2 不同ERCC1和Ki67表达患者临床治疗有效率比较 见表2。与ERCC1-Ki67-比较,ERCC1+Ki67-、ERCC1-Ki67+和ERCC1+Ki67+组患者临床治疗有效率明显降低(P<0.05),与ERCC1+Ki67-和ERCC1-Ki67+比较,ERCC1+Ki67+组患者临床治疗有效率下降更显著(P<0.05)。
2.3 不同ERCC1和Ki67表达患者生存率比较 129例患者随访3~60个月,没有失访者,平均随访(50.9±5.8)个月。根据随访过程中患者死亡情况建立生存曲线,见图2。分析显示ERCC1-Ki67-、ERCC1+Ki67-、ERCC1-Ki67+和ERCC1+Ki67+组患者累积生存率分别为83.33%,62.50%,60.60%和31.48%。采用Log-Rank检验对4组患者累积生存率比较显示,ERCC1+Ki67-、ERCC1-Ki67+患者累积生存率明显高于ERCC1+Ki67+组患者(P<0.05),但是其明显低于ERCC1-Ki67-患者(P<0.05)。
3 讨论
乳腺癌化疗耐药是目前临床面临的主要治疗问题,因此探讨导致化疗耐药的机制是目前临床研究的重点和热点。近年来研究显示,许多基因的异常表达如P-gp等可能参与乳腺癌的化疗耐药性。其中ERCC1是重要的核苷酸剪切修复家族成员之一,其主要参与DNA损伤识别和DNA链的切割,在DNA修复过程中具有重要作用[12-13]。LORD等[14]在非小细胞肺癌患者组织中发现ERCC1 mRNA表达水平与含铂类化疗药物存在密切关系,高表达患者的生存期明显短于低表达患者。另一项前瞻性研究显示ERCC1高表达的患者接受卡铂和吉西他滨联合治疗的临床缓解率明显低于ERCC1低表达患者,证实ERCC1表达水平与铂类化疗药物的敏感性相关[15]。Ki67抗原是与细胞增殖相关的核抗原,参与细胞的有丝分裂,目前研究显示其在肿瘤的发生、浸润和转移等过程中发挥着重要作用[16-17]。近年来,有学者也提出其与肿瘤化疗敏感性相关。一项直肠癌研究显示Ki67高表达的患者对放化疗的敏感性明显降低,接受化疗的Ki67指数较高的患者生存期明显低于Ki67低表达者[18]。但是这两个蛋白在乳腺癌组织中的表达水平与铂类化疗药物敏感性之间是否存在关系,目前报道较少[19]。因此本研究分析不同ERCC1和Ki67表达水平的患者接受铂类化疗后的临床治疗有效率和生存率的变化。
ERCC1-Ki67-患者临床治疗有效率明显高于ERCC1+Ki67-和ERCC1-Ki67+组患者,说明ERCC1和Ki67的高水平表达可能降低患者对铂类化疗药物的敏感性。如果这一结果成立,则ERCC1+Ki67+表达双阳性患者临床治疗有效率则更低。本研究结果如预期,发现ERCC1+Ki67+组患者临床治疗有效率远远低于ERCC1-Ki67+和ERCC1+Ki67-组患者。这一结果充分说明ERCC1和Ki67的高表达与乳腺癌患者铂类化疗的临床治疗有效率呈负相关。即ERCC1和Ki67表达预告,临床治疗有效率越低,并表现出协同叠加效应。
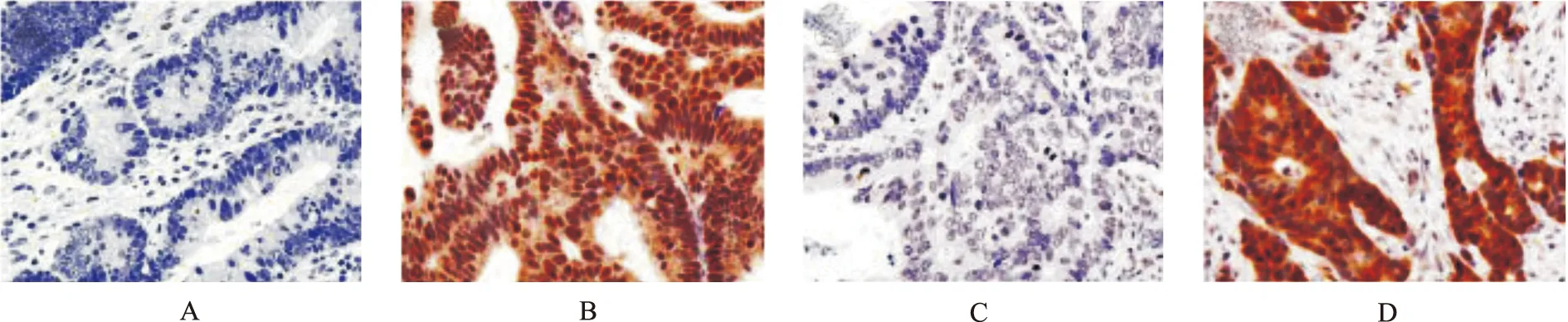
A.ERCC1阴性;B.ERCC1阳性;C.Ki67阴性;D.Ki67阳性

表1 4组患者一般资料比较 例Tab.1 Comparison of baseline data among four groups of patients

表2 4种ERCC1和Ki67表达患者临床治疗有效率比较 例Tab.2 Comparison of clinical effective rate among four groups of patients with different expression of ERCC1 and Ki67

图2 4种ERCC1和Ki67表达水平患者5年累积生存率比较
Fig.2 Comparison of 5-year cumulative survival rate among four groups of patients with different expression of ERCC1 and Ki67
在生存率方面,由于ERCC1和Ki67的高表达直接导致患者对化疗药物的耐药,因此生存时间ERCC1-Ki67-患者>ERCC1+Ki67-和ERCC1-Ki67+患者> ERCC1+Ki67+患者。
综上所述,ERCC1和Ki67在乳腺癌组织中呈高表达,并与铂类化疗药物的敏感性有密切关系。检测其表达水平对于个性化选择化疗药物具有重要意义。但是本研究病例有限,需进一步增加样本量进行统计分析,增加结果的说服力。
[1] SIEGEL R,NAISHADHAM D,JEMAL A.Cancer statistics,2012[J].CA Cancer J Clin,2012,62(1):10-29.
[2] POTHURI B.BRCA1-and BRCA2-related mutations:thera-peutic implications in ovarian cancer[J].Ann Oncol,2013,24(Suppl 8):22-27.
[3] 程军,张士勇,叶云.奥沙利铂临床应用评价分析[J].医药导报,2014,33(4):515-517.
[4] MUALLEM M Z,BRAICU I,NASSIR M,et al.ERCC1 exp-ression as a predictor of resistance to platinum-based chemotherapy in primary ovarian cancer[J].Anticancer Res,2014,34(1):393-399.
[5] 杜培,王沂峰,张晓薇,等.ERCC1和BRCA1表达与原发性上皮性卵巢癌患者临床因素及铂类化疗敏感性的研究[J].医药导报,2014,33(6):747-751.
[6] PATHMANATHAN N,BALLEINE R L.Ki67 and prolife-ration in breast cancer[J].J Clin Pathol,2013,66(6):512-516.
[7] DOWSETT M,NIELSEN T O,A'HERN R,et al.Assessment of Ki67 in breast cancer:recommendations from the international Ki67 in breast cancer working group[J ].J Natl Cancer Inst,2011,103(22):1656-1664.
[8] CIANCIO N,GALASSO M G,CAMPISI R,et al.Prognostic value of p53 and Ki67 expression in fiberoptic bronchial biopsies of patients with non small cell lung cancer[J].Multidiscip Respir Med,2012,7(1):29.
[9] KRIKELIS D,BOBOS M,KARAYANNOPOULOU G,et al.Expression profiling of 21 biomolecules in locally advanced nasopharyngeal carcinomas of Caucasian patients[J].BMC Clin Pathol,2013,(13):1.doi:10.1186/1472-6890-13-1.
[10] ZAJCHOWSKI D A,KARLAN B Y,SHAWVER L K.Treat-ment-related protein biomarker expression differs between primary and recurrent ovarian carcinomas[J].Mol Cancer Ther,2012,11(2):492-502.
[11] 单利,韩志刚,刘莉,等.晚期非小细胞肺癌ERCCl和BRCAl的表达及与顺铂耐药性的临床研究[J].肿瘤,2009,29(6):571-574.
[12] CHEN X,WU J,LU H,et al.Measuring β-tubulin Ⅲ,Bcl-2,and ERCC1 improves pathological complete remission predictive accuracy in breast cancer[J].Cancer Sci,2012,103(2):262-268.
[13] FU J M,ZHOU J,SHI J,et al.Emodin affects ERCC1 exp-ression in breast cancer cells[J].J Transl Med,2012,10 (Suppl 1):7.
[14] LORD R V,BRABENDER J,GANDARA D,et al.Low ER-CC1 expression correlates with prolonged survival after cisplatin plus gemcitabine chemotherapy in non-small cell lung cancer[J].Clin Cancer Res,2002,8(7):2286-2291.
[15] HANDRA-LUCA A,HERNANDEZ J,MOUNTZIOS G,et al.Excision repair cross complementation group 1 immunohistochemical expression predicts objective response and cancer-specific survival in patients treated by cisplatin-based induction chemotherapy for locally advanced head and neck squamous cell carcinoma[J].Clin Cancer Res,2007,13(13):3855-3859.
[16] KONTZOGLOU K,PALLA V,KARAOLANIS G,et al.Cor-relation between Ki67 and breast cancer prognosis[J].Oncology.2013,84(4):219-225.
[17] YERUSHALMI R,WOODS R,RAVDIN P M,et al.Ki67 in breast cancer:prognostic and predictive potential[J].Lancet Oncol,2010,11(2):174-183.
[18] SUROWIAK P,MATERNA V,KAPLENKO I,et al.Topoi-somerase 1A,HER/2neu and Ki67 expression in paired primary and relapse ovarian cancer tissue samples[J].Histol Histopathol,2006,21(7):713-720.
[19] KIM N K,PARK J K,LEE K Y,et al.p53,BCL-2,and Ki-67 expression according to tumor response after concurrent chemoradiotherapy for advanced rectal cancer[J].Ann Surg Oncol,2001,8(5):418-424.
ERCC1 and Ki67 Expression in Patients with Breast Cancer and Relationship Between Its Expression and Sensitivity of Platinum Chemotherapy
WEI Xin1, YANG Julun2
(1.DepartmentofPathology,ZunyiMedicalandPharmaceuticalCollege,Zunyi563000,China;2.DepartmentofPathology,KunmingGeneralHospitalofChengduMilitaryRegion,Kunming650000,China)
Objective To investigate the expressions of excision repair cross complementation group 1 (ERCC1) and Ki67 in patients with breast cancer, and the relationships between their expressions and sensitivity of platinum-based chemotherapy. Methods Totally, 129 cases were pathologically diagnosed as breast cancer.Paclitaxel and carboplatin were used simultaneously.Chemotherapy regimen was as follows: Gemcitabine 1 000 mg·(m2)-1, IV drop on day 1 and 8;cisplatin 25 mg·(m2)-1, IV drop on day 1-3, for six cycles (21 days a cycle).ERCC1 and Ki67 expression in tumor tissue was observed by immunohistochemical analysis.Platinum-based chemotherapy sensitivity and survival of patients with different levels of ERCC1 and Ki67 expression were analyzed. Results In 129 patients, 18 cases were ERCC1 and Ki67 double-negative (ERCC1-Ki67-), and the clinical effective rate and 3-year cumulative survival rate were 88.89% and 83.33%, respectively.Twenty-four cases were ERCC1 positive but Ki67 negative (ERCC1+Ki67-), and the clinical effective rate and 3-year cumulative survival rate were 50.00% and 62.50%, respectively.Thirty-three cases were ERCC1 negative but Ki67 positive (ERCC1-Ki67+), and the clinical effective rate and 3-year cumulative survival rate were 54.55% and 60.60%, respectively.Fifty-four patients were ERCC1 and Ki67 double-positive (ERCC1+Ki67+), and the clinical effective rate and 3-year cumulative survival rate were 22.78% and 31.48%, respectively.Compared with ERCC1-Ki67-group, the clinical treatment efficiencies of cisplatin-based chemotherapy in ERCC1+Ki67-group, ERCC1-Ki67+group, and ERCC1+Ki67+group were significantly decreased (P<0.05).The clinical treatment efficiency in patients of ERCC1+Ki67+group with cisplatin-based chemotherapy was significantly decreased as compared with ERCC1+Ki67-group and ERCC1-Ki67+group (P<0.05).Compared with ERCC1-Ki67-group, three-year cumulative survival rate in patients of ERCC1+Ki67-group and ERCC1-Ki67+group, ERCC1+Ki67+group was significantly decreased (P<0.05).Compared with ERCC1+Ki67-group and ERCC1-Ki67+group, three-year cumulative survival rate in patients of the ERCC1+Ki67+group was significantly decreased (P<0.05). Conclusion The expression levels of ERCC1 and Ki67 in breast cancer were high.Their expression levels are closely related with clinical efficiency of platinum-based chemotherapy.
Chemotherapy drugs;Cancer, breast;Excision repair cross complementation group 1;Ki67;Chemosensitivity
2014-09-29
2014-12-20
魏昕(1975-),女,贵州遵义人,副教授,学士,研究方向:病理学与病理生理学、乳腺癌。电话:(0)18877339318,E-mail:gfdxj8641@163.com。
R979.1;R737.9
B
1004-0781(2015)10-1314-05
10.3870/j.issn.1004-0781.2015.10.014
