Observation on Therapeutic Effects of Acupuncture plus Psychological Intervention for Postpartum Depression
2014-06-27HuangHanling1PengLiZhengSu3WangLushan
Huang Han-ling1, Peng Li, Zheng Su3, Wang Lu-shan
1 Physical Examination Center, Taihe Hospital, Hubei University of Medicine, Shiyan 442000, China
2 Department of Acupuncture and Moxibustion, Taihe Hospital, Hubei University of Medicine, Shiyan 442000, China
3 Outpatient Office, Taihe Hospital, Hubei University of Medicine, Shiyan 442000, China
CLINICAL STUDY
Observation on Therapeutic Effects of Acupuncture plus Psychological Intervention for Postpartum Depression
Huang Han-ling1, Peng Li2, Zheng Su3, Wang Lu-shan2
1 Physical Examination Center, Taihe Hospital, Hubei University of Medicine, Shiyan 442000, China
2 Department of Acupuncture and Moxibustion, Taihe Hospital, Hubei University of Medicine, Shiyan 442000, China
3 Outpatient Office, Taihe Hospital, Hubei University of Medicine, Shiyan 442000, China
Author:Huang Han-ling, undergraduate, attending physician
Objective: To observe the therapeutic effect of acupuncture plus psychological intervention for postpartum depression.
Methods: By random number table, 85 patients with postpartum depression were divided into a treatment group and a control group. Forty-three cases in the treatment group were treated by acupuncture plus psychological intervention, once every day, five sessions per week, and rest at weekend. Forty-two cases in the control group were treated by oral administration of Fluoxetine Hydrochloride, 20 mg, once per day. The two groups were treated continuously for six weeks. The change of the score in Hamilton depression scale (HAMD) was observed and the therapeutic effect was summarized.
Results: The total effective rate was 90.7% in the treatment group and 90.5% in the control group. The difference in the total effective rate between two groups was not statistically significant (P>0.05). In the intra-group comparisons of HAMD scores two, four and six weeks after treatment in both groups with those before treatment, the differences were statistically significant (allP<0.05). In comparison between the two groups at the same time point, the differences in HAMD scores were not statistically significant (allP>0.05). Regarding the adverse events, 5 cases had nausea, 3 cases had dizziness, and 6 cases had poor appetite in the control group; no obvious adverse events happened in the treatment group.
Conclusion: Acupuncture plus psychological intervention for postpartum depression is as same as oral administration of Fluoxetine Hydrochloride in therapeutic effects, but it does not have adverse reaction.
Acupuncture Therapy; Moxibustion Therapy; Suspended Moxibustion; Spondylosis; Neck Pain
In accordance with the fourth edition ofDiagnostic and Statistical Manual of Mental Disorders(DSM-Ⅳ), postpartum depression (PPD) refers to depression occurring within four weeks after delivery. Typical PPD often occurs in two weeks after delivery and the symptoms are obvious in four to six weeks after delivery. The duration can last for 3-6 months. Its symptoms are not different from those in ordinary depression, featured by lassitude and listlessness. Cai ZJ[1]believes that depression is a group of symptoms, clinically characterized by tears, sadness, emotional instability, feeling of guilty, loss of appetite, sleep disorders, memory problem, fatigue, irritability, anxiety, fear and depression. PPD not only influences the health of thelying-in women and the stability of marriage and family, but also results in communicative disorder between mother and baby, unbeneficial to the development of baby’s intelligence and behavior[2]. It has been indicated in the epidemiological investigation that the postpartum period is the highest risky period for depression[3-4]. We treated PPD with acupuncture plus psychological intervention in recent years. Now, the report is given as follows.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria in Western medicine
They were based upon the third edition ofChinese Classification and Diagnosis of Mental Disorders(CCMD-Ⅲ)[5]. The patients suffered from PPD mainly present listlessness, together with four items of the flowing symptoms at least: lack of pleasure or interest, loss of energy or fatigue, psychomotor retardation or agitation, low self esteem, self accusation or guilty, associative difficulty or subjective decline of thinking ability, recurrent thoughts for suicide or suicidal and self-inflecting behavior, sleep disorders like insomnia or hypersomnia, reduced appetite or significant weight loss; and low sexuality. The patients with organic disorders were excluded by inspections of various systems and laboratory inspections.
1.1.2 Diagnostic criteria in Chinese medicine
This disease belongs to depression syndrome in traditional Chinese medicine (TCM). Its diagnostic criteria were based upon theCriteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine[6]: depression, low spirit, stuffy sensation in the chest and distending sensation in the hypochondriac region, frequent sighing, or loss of appetite, insomnia and dreamful sleep, easy frustration and easy crying, accompanied by history of emotional injuries like depression, angry, worries, sadness, and melancholy.
1.2 Inclusion criteria
In conformity with the above diagnostic criteria; Hamilton depression scale (HAMD)[7]score≥17 points, ≤30 points.
1.3 Exclusion criteria
Those with serious cardiac, hepatic and renal diseases, glaucoma and epilepsy; those with organic mental disorders, alcohol dependence, medication dependence; and those with suicidal intention.
1.4 Statistical methods
The SPSS 13.0 version software package was used for analysis. The counting data were processed by Chi-square test. The measuring data were expressed by mean ± standard deviation. The paired samplet-test was adopted for comparison within the group. The independent samplet-test was adopted for comparison between the groups.P<0.05 indicated the statistical significance in difference.
1.5 General data
Total of 85 patients with PPD were selected from the Acupuncture Clinic and Gynecology and Obstetrics Department of our hospital from January of 2010 to October of 2012, and were divided into two groups by random digital table, 43 cases in the treatment group and 42 cases in the control group. The differences in age and duration between the two groups were not statistically significant (P>0.05), indicating the two groups were comparable (Table 1).
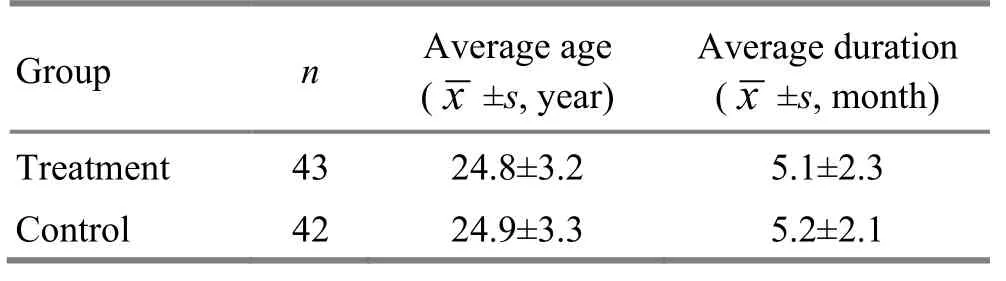
Table 1. Comparison of general data between the two groups
2 Therapeutic Methods
2.1 Treatment group
2.1.1 Acupuncture
Acupoints: Baihui (GV 20), Sishencong (EX-HN 1), Neiguan (PC 6), Taichong (LR 3), Sanyinjiao (SP 6), Zusanli (ST 36).
Operation: After the patient took a supine position and the acupoints were routinely disinfected, the needles of 0.35 mm in diameter and 25 mm in length were inserted subcutaneously into Sishencong (EX-HN 1) with the needle tip toward Baihui (GV 20). The other acupoints were punctured routinely. The needles were manipulated by moderate needling technique after the arrival of the needling sensation, till the patients had sensations of soreness and distending and felt comfortable. The needles were retained for 30 min. The treatment was given for five sessions per week, for totally six weeks.
2.1.2 Psychological intervention
The patients were educated about the healthcare knowledge for stegmonth, how to deal with depressive and anxious emotion. The patients should be cared more attentively and thoughtfully, so as to enable to have better adapting status physically and mentally, to go through the puerperal period, to decrease the incidence of PPD and to eliminate their self-believed incompatibility. In accordance with their individual features, psychological status and pathogenic reason, the patients were given the individualized psychological consultation to relieve their pathogenic factors.
By building up a satisfactory family atmosphere, the family members and relatives, especially husband, were asked to show care and consideration to the patient, so as to enable the patient to enjoy the warm concern from the family. The family members were told to take care of the lying-in woman and baby and manage the housework well, to reduce pressure on the lying-in woman. The husbands and family members were instructed to know the importance of close husband and wife relationship and family care for the physical and mental health of the lying-in women and babies, to intensify the participating consciousness of the lying-in women in housework after delivery, to advocate sharing duties of family members to take care of babies, and to reduce the patients’ fatigue and psychological burden.
The patients were instructed about the nursing knowledge and techniques to breastfeed baby and take care of themselves and newborn, to promptly relieve their confusion.
2.2 Control group
The control group was given oral administration of Fluoxetine Hydrochloride, 20 mg, once per day, for totally six weeks.
3 Therapeutic Effects
3.1 Criteria of therapeutic effects
The therapeutic effects were assessed based upon clinical symptoms and HAMD score after treatment[8].
Cure: The mental symptoms disappeared and HAMD score was reduced to 7 points or below.
Remarkable effect: The mental symptoms disappeared basically and HAMD score were reduced by over 50%.
Effect: The mental symptoms were relieved and HAMD score was reduced by 25%-50%.
Failure: HAMD score was reduced less than 25%.
3.2 Results
3.2.1 Comparison of clinical effects
The results showed that the total effective rate was 90.7% in the treatment group, and 90.5% in the control group. There was no statistical difference in comparison of the total effective rate between the two groups (P>0.05), (Table 2).
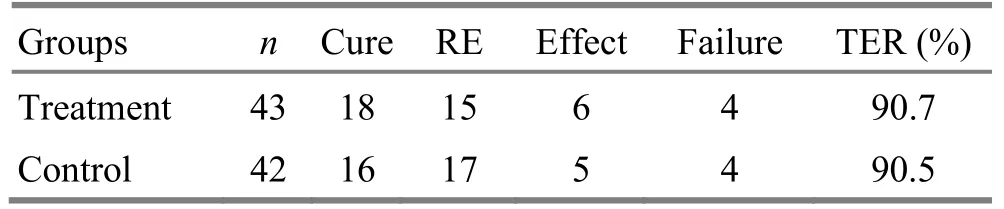
Table 2. Comparison of general data between the two groups (case)
3.2.2 Comparison of HAMD score
In inter-group comparison of HAMD scores after 2, 4 and 6 weeks by pairedt-test, there were not statistical differences between the two groups. In intra-group comparison of HAMD scores after 2, 4 and 6 weeks of the two groups, there were statistical differences in the two groups (allP<0.05), (Table 3).
Table 3. Comparison of HAMD scores before and after treatment (, point)
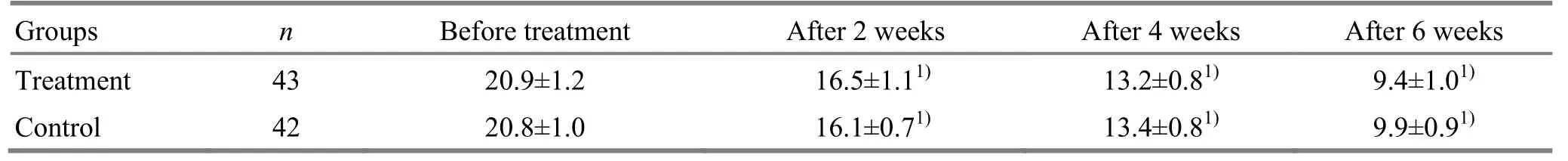
Table 3. Comparison of HAMD scores before and after treatment (, point)
Note: Compared with the same group before treatment,P<0.05
?
3.3 Observation of adverse reaction
After administration of Fluoxetine Hydrochloride, adverse reactions were present in the control group, including nausea in 5 cases, dizziness in 3 cases and loss of appetite in 6 cases. No adverse reaction was present in the treatment group.
4 Discussion
It is believed in TCM that PPD is related to personal disposition, condition of qi and blood in Zang-fu organs, and stimulation from internal and external environment[9]. Those factors can elevate the sensibility and decrease the tolerance to the external stimulation, causing extreme emotional fluctuations.
By regulating the exciting and inhibiting process of the cerebral cortex via the nervous system and immune system, acupuncture is able to balance various neurotransmitters among the intracephalic neuronal synapses, reduce the brain’s reaction to stress, relax the stressful spirit, regulate and treat the physical symptoms and relieve the depressive and anxious state. ‘The head is the gathering site of all yang and the house of the mind’, therefore, Baihui (GV 20) and Sishencong (EX-HN 1) are selected to open orifice, wake up the brain, relieve depression and calm the mind. Hegu (LI 4) is the Yuan-Primordial acupoint of the Large Intestine Meridian, and Taichong (LR 3) is the Yuan-Primordial acupoint of the Liver Meridian. The two acupoints in combination, termed ‘to open the four passes’, can regulate qi andblood and regulate yin and yang of the whole body, to soothe the liver and regulate qi, open the orifice and calm the mind. Neiguan (PC 6), the Luo-Connecting acupoint of the Pericardium Meridian, is used to regulate and nourish the heart qi and calm down the mind. Sanyinjiao (SP 6), a crossing acupoint of three yin meridians of foot, is used to regulate qi and blood in the Liver Meridian, the Spleen Meridian and the Kidney Meridian. Zusanli (ST 36) is used to tonify the stomach qi, to assist the source of qi and blood production. Those acupoints in combination are used to correct deficiency and expel blood stasis for both causative factors and symptoms, in order to realize the effects to soothe the liver, regulate qi, wake up the brain and tranquilize the heart-mind.
The postpartum period is often believed to be a period of maternal adaptation full of stress and even a risky period[10]. Most lying-in women lack experience to nurse themselves and babies, but also hope to be a ‘perfect’ mother. The higher expectation, fatigue from parenting baby and other bad factors in combination would certainly enable the lying-in women to feel their ability not equal to their wishes, leading to a feeling of setback and failure. Therefore, the guidance and social support are highly needed in this period. The purpose of the intervening measure is supposed to strengthen the social support, in order to help the lying-in women to go through their crisis. The social support includes the supports of emotional, information, material and assessment. The pregnant women school can give women adequate knowledge about pregnancy, delivery, baby care and self-nursing, so as to reduce prenatal anxiety and enhanced the confidence. At the same time, family member also should be instructed the importance of family emotional support and housework participation, so that the family members could share the postnatal care of infants. This measure intensifies the emotional and material support. The participation of family members, especially husband, can effectively reduce the fear of the lying-in women about delivery. Concerns and emotional support from husband give the lying-in women a great psychological support. After delivery, the visiting nurse instructs promptly the nursing techniques to take care of baby, solves the anxiety factor and reduces the patients’ stress. Moreover, the targeted psychological treatment is important. The comprehensive effect of above measures intensifies the role of social support and will help the lying-in women to go through the period of weak emotions after delivery.
Fluoxetine Hydrochloride is a serotonin reuptake inhibitor, it is used for control treatment in this study. The results showed that the therapeutic effects are similar in the two groups. In comparison of the clinical effects and HAMD score, the differences are not statistically significant between the two groups (allP>0.05), but adverse reaction is less in the treatment group, indicating that acupuncture plus psychological intervention can be used for clinical treatment of PPD.
Conflict of Interest
There was no potential conflict of interest in this article.
Acknowledgments
This work was supported by Taihe Hospital, Hubei University of Medicine.
Statement of Informed Consent
All of the patients signed the informed consent.
[1] Cai ZJ. Bases and Clinics of Depression. 2nd Edition. Beijing: Science Publishers, 2001: 11.
[2] He Y, Wang XH, He GP. Research progress on postpartum depression and social factors. Zhongguo Xingwei Yixue Zazhi, 2008, 17(9): 859-861.
[3] Maurer-Spurej E, Pittendreigh C, Misri S. Platelet serotonin levels support depression scores for women with postpartum depression. J Psychiatry Neurosci, 2007, 32(1): 23-29.
[4] He P, Zhao JB, Yang HL, Chen JS, Luo J, Pan YH, Hao YT, Di JL. An analysis on the incidence and its sociological factors of postpartum depression. Zhongguo Fuyou Baojian, 2006, 21(10): 1388-1390.
[5] Chinese Society of Psychiatry. Chinese Classification and Diagnosis of Mental Disorders. 3rd Edition. Jinan: Shandong Science and Technology Publishers, 2001: 87-88.
[6] State Administration of Traditional Chinese Medicine. Criteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine. Nanjing: Nanjing University Press, 1994: 21.
[7] Wang XD, Wang XL, Ma H. Manual of Mental Health Assessment Scale. Revised Edition. Beijing: Zhongguo Xinli Weisheng Zazhishe, 1999: 200-223.
[8] Fan L, Fu WB, Meng CR, Zhu XP, Mi JP, Li WX, Wen X. Effect of acupuncture at routine acupoint and non-acupoint on depressive neurosis evaluated with Hamilton depression scale. Zhongguo Linchuang Kangfu, 2005, 9(28): 14-16.
[9] Gao YJ, Gao KX, Zhang XF. A talk on etiology and pathogenesis of traditional Chinese medicine and nursing for postpartum depression. Shaanxi Zhongyi, 2006, 25(9): 28-29.
[10] Logsdon MC, McBride AB, Brikimer JC. Social support and postpartum depression. Res Nurs Health, 1994, 17(6): 449-457.
Translator:Huang Guo-qi
Wang Lushan, lecturer, attending physician.
E-mail: wanglushan5463@163.com
R246.3
: A
Date:July 28, 2014
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Warm Needling Moxibustion at Zhongji (CV 3) and Zusanli (ST 36) for Urinary Retention after Gynecological Surgery
- Therapeutic Efficacy Observation on Acupoint Sticking for Edema Due to Chronic Cardiac Failure
- Therapeutic Efficacy Analysis of Balancing Yin-yang Manipulation for Post-stroke Upper Limb Spasticity
- Acupoint Massage in Relieving Pain after Ureteroscopic Holmium Laser Lithotripsy
- Tuina plus Ultrasonic Therapy for Infantile Muscular Torticollis
- Personal Experience on Palpation of the Spine
