Qi-guiding Needling Based on Meridian Differentiation for Lumbar Disc Herniation: A Multi-centered, Randomized Controlled Trial
2014-06-27WuYaochiSunYijunZhangJunfengLiYan2ZhangYiyi3WangChongmiao
Wu Yao-chi, Sun Yi-jun, Zhang Jun-feng, Li Yan2, Zhang Yi-yi3, Wang Chong-miao
1 Shanghai Jiao Tong University Affiliated Sixth People’s Hospital, Shanghai 200233, China
2 Tianshan Hospital of Traditional Chinese Medicine, Changning District, Shanghai, Shanghai 200051, China
3 Hongqiao Community Health Service Center, Changning District, Shanghai, Shanghai 200051, China
SPECIAL TOPIC STUDY
Qi-guiding Needling Based on Meridian Differentiation for Lumbar Disc Herniation: A Multi-centered, Randomized Controlled Trial
Wu Yao-chi1, Sun Yi-jun1, Zhang Jun-feng1, Li Yan2, Zhang Yi-yi3, Wang Chong-miao1
1 Shanghai Jiao Tong University Affiliated Sixth People’s Hospital, Shanghai 200233, China
2 Tianshan Hospital of Traditional Chinese Medicine, Changning District, Shanghai, Shanghai 200051, China
3 Hongqiao Community Health Service Center, Changning District, Shanghai, Shanghai 200051, China
Author:Wu Yao-chi, master of medicine, professor, doctoral supervisor
Objective: To observe the efficacy of acupoint selection by meridian differentiation plus qi-guiding needling in treating lumbar disc herniation (LDH).
Methods: By using the random number table, 549 patients with LDH were randomized into two groups. Two hundred and eighty participants in the observation group were intervened by selecting acupoints by meridian differentiation associated with qi-guiding needling method, and the other 269 participants in the control group were by selecting acupoints by meridian differentiation plus electroacupuncture. At the end of intervention, the changes of conduction velocities of the common peroneal nerve, superficial peroneal nerve, and tibial nerve were observed, and the therapeutic efficacies were compared.
Results: The total effective rate was 87.5% in the observation group versus 86.6% in the control group, and the difference was statistically insignificant (P>0.05). The recovery rate was 51.8% in the observation group versus 37.2% in the control group, and the difference was statistically significant (P<0.05).
Conclusion: Selecting acupoints by meridian differentiation associated with qi-guiding needling can produce a similar total effective rate to selecting acupoints by meridian differentiation plus electroacupuncture, while its recovery rate is comparatively higher.
Acupuncture Therapy; Electroacupuncture; Low Back Pain; Spondylosis; Randomized Controlled Trial
Lumbar disc herniation (LDH) is caused by compression or stimulation of the extruded nucleus to the nerve root, cauda equina, or spinal cord at the corresponding segment due to external force or degeneration of intervertebral disc and subsequent tears of fibrous ring. It’s characterized by low back pain, radiating pain to lower extremities, or numbness[1-2]. Acupuncture-moxibustion is a commonly used conservative therapy for LDH, with confirmed efficacy and insignificant adverse reactions[3].
Since the year 2012, by adopting a multi-centered, large-sample, randomized controlled trial protocol, we observed the clinical efficacy of selecting acupoints based on meridian differentiation associated with qi-guiding acupuncture, compared to the same acupoint selection method plus electroacupuncture (EA).
1 Clinical Materials
1.1 Diagnostic criteria
By referring the diagnostic criteria of LDH from theCriteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine[4]andShanghai Diagnostic and Therapeutic Guidelines of Traditional Chinese Medicine[5]: a history of trauma or chronic strain, or cold contraction of low back, and chronic low back pain in the majority of the patients before onset; young adults are mainly affected; pain radiating from low back to lower extremities, aggravated by increased abdominal pressure (such as cough and sneeze); lateral curve of the spine instead of the normal physiological curve, and tender points beside the affected spine segment causing radiating pain to the lower extremity, with limited motility of low back; supersensitivity or dysesthesia of lower extremities in the charge of the affected nerves, and muscular atrophy may found in long-term sufferers; positive straight leg raising test, decreased or diminished knee and Achilles reflexes, and reduced extension of the big toe; lateral curve, diminished physiological curve of lumbar verbebrae, narrowed intervertebral spaces, and osteophyte found by X-ray, CT scan or MRI (the ruptured discs can also be located and measured by CT or MRI examination).
1.2 Inclusion criteria
In conformity with the above diagnostic criteria of LDH; age 18-65 years old, with no sex predilection; having signed the informed consent form and can follow the treatment protocol.
1.3 Exclusion criteria
Against the above inclusion criteria; severe diseases involving cardiovascular, cerebrovascular, liver, kidney, or hematopoietic system; moderate or above level of osteoporosis, abdominal aorta sclerosis, or mental disorders; spinal tumor, tuberculosis, or ankylosing spondylitis; disassociated or ossified extruded nucleus detected by CT scan, severe spinal canal stenosis due to ossification, or calcification of posterior longitudinal ligament; relapsed LDH after spinal surgery; pregnant women; cauda equina syndrome manifested by numbness around the saddle area, or having problems with urination and defecation; motor dysfunction such as foot drop.
1.4 Statistical methods
After data collection, the SPSS 19.0 version software was used for processing. The intra-group comparison of measurement data was performed byt-test; regarding the inter-group comparisons of the change of measurement data, the Wilcoxon test was used for abnormal distribution, and Fisher’s exact test for data containing 0 or theoretical value less than 5.
1.5 General data
The enrolled subjects were from Shanghai Jiao Tong University Affiliated Sixth People’s Hospital, Tianshan Hospital of Traditional Chinese Medicine, or Hongqiao Community Health Service Center, either inpatient or outpatient, from December 1, 2012 to March 30, 2014. Totally 549 subjects were randomized into two groups by enveloping randomization, 280 cases in the observation group and 269 in the control group. The statistical analyses showed that there were no significant differences in comparing the gender, age, disease duration, or meridian differentiation of lumbago between the two groups (allP>0.05), indicating the comparability (Table 1).

Table 1. Comparison of genera data
2 Treatment Methods
2.1 Observation group
Patients in the observation group were treated with acupoint selection based on meridian differentiation plus qi-guiding acupuncture[6].
Lumbago affecting the Taiyang Meridian: Shenshu (BL 23), Dachangshu (BL 25), Zhibian (BL 54), Huantiao (GB 30), Juliao (GB 29), Yinmen (BL 37), Weizhong (BL 40), Chengshan (BL 57), and Kunlun (BL 60).
Lumbago affecting the Yangming Meridian: Shenshu (BL 23), Dachangshu (BL 25), Qichong (ST 30), Biguan (ST 31), Futu (ST 32), Tiaokou (ST 38), and Zusanli (ST 36).
Lumbago affecting the Shaoyang Meridian: Shenshu (BL 23), Dachangshu (BL 25), Huantiao (GB 30), Fengshi (GB 31), and Yanglingquan (GB 34).
Operation: After sterilization with 75% alcohol, filiform needles of 0.30 mm in diameter and 40 mm or 75 mm in length were punctured into the acupoints, by 2.5 cun in Huantiao (GB 30) and Juliao(GB 29), and 1.2 cun for the rest points. When qi was obtained by lifting-thrusting and twirling manipulations, reducing qi-guiding needling was applied to Weizhong (BL 40), Tiaokou (ST 38), and Yanglingquan (GB 34), to induce the needling sensation to the posterior aspect of bottom or lower back; when Huantiao (GB 30), Juliao (GB 29) and Biguan (ST 31) were needled, the needling sensation should reach to the lower body till calf or foot. Reinforcing qi-guiding needling method was applied to Dachangshu (BL 25) to induce the needling sensation to lumbosacral region, and to Shenshu (BL 23) to produce a distending sensation in lower back, and the patient should feel full of bliss when treated. During the acupuncture treatment, frequent twirling and lifting-thrusting manipulations were performed to promote qi, associated with pressing along the meridian course. The needles were retained for 20 min, manipulated once every 5 min. The treatment was given once every other day, 10 times as a treatment course.
2.2 Control group
The acupoint-selection method was as same as that in the observation group.
Operation: EA was used instead of qi-guiding needling method, while the size of needle and needling depth were the same as those in the observation group[7]. Moderate reinforcing-reducing needling manipulations were performed when qi was obtained, 1 min for each acupoint, to produce tingling, distending, and sore needling sensations in the treated areas. When Huantiao (GB 30) and Juliao (GB 29) were needled, the tip of the needle should be towards the external genitals, producing radiating tingling feeling. Then two pair of acupoints were selected to connect with G6805-Ⅱ EA apparatus, with continuous wave at 4.0 Hz, and intensity 2 mA. The needles were retained for 20 min, and the treatment was given once every other day, 10 times as a treatment course.
The therapeutic efficacies of the two groups were evaluated after 10 sessions of treatment.
3 Observation of Therapeutic Efficacies
3.1 Observation indexes
The conduction velocities of the common peroneal nerve, superficial peroneal nerve, and tibial nerve were tested before and after intervention[2,8].
3.2 Criteria of therapeutic efficacy
The trained specific researchers were in charge of collecting, recording, keeping and analyzing the relevant data, while the clinical practitioners were not involved in the evaluation of therapeutic efficacy. The criteria of therapeutic efficacy were made based on the corresponding criteria from theCriteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine[4]andShanghai Diagnostic and Therapeutic Guidelines of Traditional Chinese Medicine[5].
Recovery: Lumbago was gone, straight leg lift≥70°, and patient could go back to work.
Improved: Lumbago was reduced, and motor function of lower back was improved.
Invalid: Symptoms and signs were not improved.
3.3 Treatment results
3.3.1 Comparison of therapeutic efficacy
The difference in total effective rate between the two groups was statistically insignificant (P>0.05), indicating that the two treatment protocols both can produce content efficacies in treating LDH. The recovery rate in the observation group was significantly higher than that in the control group (P<0.05), (Table 2).
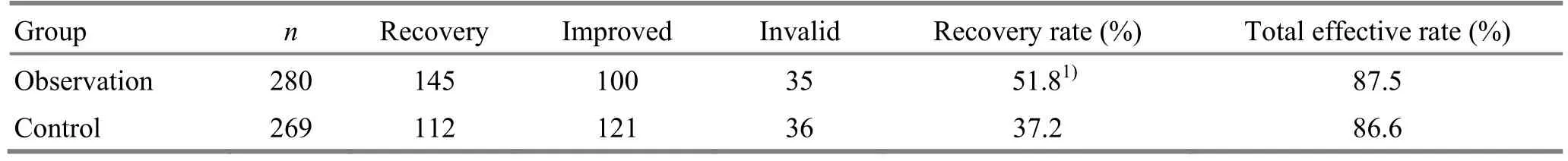
Table 2. Comparison of clinical efficacies (case)
3.3.2 Comparison of the nerve conduction velocity
Before intervention, there were no significant differences in comparing the conduction velocities of the common peroneal nerve, superficial peroneal nerve, and tibial nerve between the two groups (P>0.05). After intervention, the conduction velocities of the common peroneal nerve and superficial peroneal nerve were increased significantly in the observation group (P<0.05), also significantly different from those in the control group (P<0.01,P<0.05). There were no significant changes of the three nerve conduction velocities in the control group after intervention (allP>0.05). The conduction velocity of the tibial nerve was not significantly changed in the two groups after intervention (P>0.05). The results suggest that the improvements of the conduction velocities of the common peroneal nerve and superficial peroneal nerve in the observation group are more significant than those in the control group (Table 3).
Table 3. Comparison of the conduction velocities of the common peroneal nerve, superficial peroneal nerve, and tibial nerve (m/s)

Table 3. Comparison of the conduction velocities of the common peroneal nerve, superficial peroneal nerve, and tibial nerve (m/s)
Note: Intra-group comparison, 1) P<0.01, 2) P<0.05; compared with the control group, 3) P<0.01, 4) P<0.05
?
4 Discussion
According to traditional Chinese medicine (TCM), LDH falls under the scope of lumbago or Bi-Impediment syndrome, caused by congenital insufficiency and deficiency of liver and kidney, or damaged meridians and collaterals, and qi-blood stagnation, or contraction of wind, cold, damp, or heat, and blockage in meridians and collaterals.
The lumbago induced by LDH usually locates at the pathways of yang meridians[9]. Lu Shou-yan believed that lumbago is caused by the following factors: lumbar sprain under heavy loading; cold or damp invading meridians; stagnation of turbid yin pathogens due to deficiency of liver, kidney, and the Governor Vessel; meridian qi blocked by tumor or mass. Taiyang lumbago is manifested by pain along the Foot Taiyang Meridian from lower back to calf; Shaoyang lumbago is by pain affecting along the Foot Shaoyang Meridian; while Yangming lumbago is by pain affecting the Foot Yangming Meridian. The physician has to differentiate the affected meridian before treatment for achieving better efficacy[10].
The qi-guiding needling was first recorded byLing Shu(Spiritual Pivot): qi is guided or induced by slowly inserting and removing the needle. In his clinic, Lu Shou-yan often used qi-guiding needling to induce qi by the needling direction, i.e. to needle towards upward for guiding qi to go up, and vice versa, followed by twirling, lifting and thrusting manipulations for promoting qi-arrival, and sometimes also combined with other methods such as pressing along meridians. With this method, he could achieve content efficacy rapidly.
It’s showed that the nerve conduction velocities were increased by certain extent in the two groups after intervention, indicating that the two treatment protocols both can accelerate the nerve conduction velocity in calf. After intervention, the conduction velocities of common peroneal never and superficial peroneal nerve in the observation group were significant different from those in the control group, suggesting that qi-guiding needling based on meridian differentiation can more significantly enhance the conduction velocities of the two nerves compared to EA based on meridian differentiation. This is possibly because that qi-guiding needling can improve the ultra-microstructure and promote the healing of nerves[11].
Meridian differentiation can unblock the three meridians, thus to kill pain by diminishing the blockages. Huantiao (GB 30) connects both the Foot Taiyang Meridian and Foot Shaoyang Meridian, functioning to expell wind and resolve dampness, and strengthen lower back and knees; the topical points, such as Shenshu (BL 23), Dachangshu (BL 25), Zhibian (BL 54), Juliao (GB 29), Yinmen (BL 37), and Weizhong (BL 40), work together with the distal points to relieve lumbago; Qichong (ST 30), Biguan (ST 31), Futu (ST 32), and Tiaokou (ST 38) can activate qi of the Yangming Meridian; as the Influential Point of Tendons, Yanglingquan (GB 34) is a crucial point for regulating and unblocking the Shaoyang Meridians and easing pain.
Although there was no significant difference in comparing the total effective rate between qi-guiding needling based on meridian differentiation and electroacupuncture based on meridian differentiation, the former produced a higher recovery rate compared to the latter, indicating that this qi-guiding needling method based on meridian differentiation, highly recommended by Lu Shou-yan, is indeed effective in treating LDH, and worthy of further research.
Conflict of Interest
The authors declared that there was no conflict of interest in this article.
Acknowledgments
This work was supported by the Important Special Project of Science and Technology Commission of Shanghai Municipality (No.10DZ1950700); Lu’s Acupuncture Inheritance Study of Shanghai Schools of Traditional Chinese Medicine (No. ZYSNXD-CC-HPGC-JD-004).
Statement of Informed Consent
Informed consent was obtained from all individual participants included in this study.
[1] Hu YG. Lumbar Disc Herniation. 2nd Edition. Beijing: People’s Medical Publishing House, 1995: 146-150.
[2] Zhu WM, Wu YC, Zhang JF, Fan YZ, Li SS. Therapeutic observation of tuina plus acupoint injection for lumbar disc herniation. Zhongguo Yundong Yixue Zazhi, 2010, 29(6): 708-709.
[3] Cheng XN. China Acupuncture-moxibustion Science. Beijing: People's Medical Publishing House, 1987: 192-284.
[4] State Administration of Traditional Chinese Medicine. Criteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine. Nanjing: Nanjing University Press, 1993: 201-202.
[5] Shanghai Municipal Health Bureau. Shanghai Diagnostic and Therapeutic Guidelines of Traditional Chinese Medicine. 2nd Edition. Shanghai: Publishing House of Shanghai University of Traditional Chinese Medicine, 2003: 393-394.
[6] Wu SD. Theory and Case Collection of Lu Shou-yan's Acupuncture and Moxibustion. 2nd Volume. Beijing: People's Medical Publishing House, 2006: 165-177.
[7] Wu YC, Zhang BM. Clinical observations on electroacupuncture treatment of lumbar intervetebral disc protrusion. Shanghai Zhenjiu Zazhi, 2004, 23(5): 15-17.
[8] Wu YC, Sun YJ, Zhang JF, Huang CF, Xie YY, Zhou JH, Li SS. Observation study on effects of electroacupuncture on the muscle condition and MNCV in rabbits with lumbar nerve root compression. Zhongguo Zhenjiu, 2011: 31(11): 1009-1014.
[9] Qiu ML. Acupuncture-moxibustion Science. Shanghai: Shanghai Science and Technology Press, 1988: 63-64.
[10] Lu SY, Zhu RG. Medical Case Collection of Lu Shou-yan and Zhu Ru-gong’s Acupuncture and Moxibustion. Beijing: People’s Military Medical Press, 2009: 99-100.
[11] Sun YJ, Wu YC, Zhang JF, Zhang P, Tang ZY. Effects of electroacupuncture on muscle state and electrophysiological change in rabbits with lumbar nerve root compression. Chin J Integr Med, 2013, 19(6): 446-452.
Translator:Hong Jue
Wang Chong-miao, bachelor, chief physician.
E-mail: 18930177222@163.com
R246.2
: A
Date:July 12, 2014
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Warm Needling Moxibustion at Zhongji (CV 3) and Zusanli (ST 36) for Urinary Retention after Gynecological Surgery
- Therapeutic Efficacy Observation on Acupoint Sticking for Edema Due to Chronic Cardiac Failure
- Therapeutic Efficacy Analysis of Balancing Yin-yang Manipulation for Post-stroke Upper Limb Spasticity
- Acupoint Massage in Relieving Pain after Ureteroscopic Holmium Laser Lithotripsy
- Tuina plus Ultrasonic Therapy for Infantile Muscular Torticollis
- Personal Experience on Palpation of the Spine
